Abstract
Background
The relationship between body mass index (BMI) and liver stiffness in older people remains unclear. This study aimed to examine the association between BMI and the risk of elevated liver stiffness in older people.
Methods
2736 participants from the West China Health and Aging Cohort Study (WCHAC) were included in the present study. Liver stiffness was assessed using transient elastography (TE). The association of the 5-year average BMI level with elevated liver stiffness risk was estimated using multinomial logistic regression. The group-based trajectory model (GBTM) was applied to identify BMI trajectories. Additionally, restricted cubic spline analysis was conducted to explore the dose-response association between BMI and the risk of elevated liver stiffness.
Results
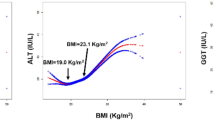
Participants in the second BMI quartile (21.93–23.58) had the lowest prevalence of elevated liver stiffness, and then the risk increased with higher BMI quartiles (BMI Q4 vs. Q2, OR = 2.05, 95% CI: 1.37–3.11 and Q5 vs. Q2, OR = 2.82, 95% CI: 1.78–4.39). There were five BMI trajectories over the five-year period: low-normal-weight stable (7.42%), moderate-normal-weight stable (29.10%), low-level-overweight stable (36.22%), high-level-overweight stable (20.32%) and stable obesity (6.94%). Participants in the moderate-normal-weight stable group had the lowest prevalence of elevated liver stiffness. Compared with this group, the adjusted ORs (95% CI) elevated liver stiffness prevalence were 2.02 (1.39–2.97) for the high-level-overweight stable, and 2.83 (1.72–4.64) for the group of people with stable obesity. Dose-response analysis revealed a U-shaped relationship between BMI and elevated liver stiffness risk, suggesting an optimal BMI range of 21.8–24.3 kg/m² for older people to minimize elevated liver stiffness risk.
Conclusions
Our study elucidated the U-shaped relationship between BMI and the risk of elevated liver stiffness as measured by TE, and the optimal BMI range from 21.8 to 24.3 kg/m2 for the lowest risk of elevated liver stiffness in older people.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The dataset that supports this article is from the WCHAC project. Data sharing requires approval, and further details on how to request the datasets can be provided upon inquiry. The full analysis code is available from the corresponding author.
Code availability
The dataset that supports this article is from the WCHAC project. Data sharing requires approval, and further details on how to request the datasets can be provided upon inquiry. The full analysis code is available from the corresponding author.
References
Younossi ZM, Wong G, Anstee QM, Henry L. The global burden of liver disease. Clin Gastroenterol Hepatol. 2023;21:1978–91. https://doi.org/10.1016/j.cgh.2023.04.015.
Devarbhavi H, Asrani SK, Arab JP, Nartey YA, Pose E, Kamath PS. Global burden of liver disease: 2023 update. J Hepatol. 2023;79:516–37. https://doi.org/10.1016/j.jhep.2023.03.017.
Maeso-Díaz R, Gracia-Sancho J. Aging and chronic liver disease. Semin Liver Dis. 2020;40:373–84. https://doi.org/10.1055/s-0040-1715446.
United Nations, Department of Economic and Social Affairs. World Social Report 2023: Leaving No One Behind in an Ageing World. New York: United Nations; 2023. Available from: https://desapublications.un.org/publications/world-socialreport-2023-leaving-no-one-behind-ageing-world.
Stebbing J, Farouk L, Panos G, Anderson M, Jiao LR, Mandalia S, et al. A meta-analysis of transient elastography for the detection of hepatic fibrosis. J Clin Gastroenterol. 2010;44:214–9. https://doi.org/10.1097/MCG.0b013e3181b4af1f.
Mueller S, Sandrin L. Liver stiffness: a novel parameter for the diagnosis of liver disease. Hepat Med. 2010;2:49–67. https://doi.org/10.2147/hmer.s7394.
Semmler G, Yang Z, Fritz L, Köck F, Hofer BS, Balcar L, et al. Dynamics in liver stiffness measurements predict outcomes in advanced chronic liver disease. Gastroenterology. 2023;165:1041–52. https://doi.org/10.1053/j.gastro.2023.06.030.
Singh S, Fujii LL, Murad MH, Wang Z, Asrani SK, Ehman RL, et al. Liver stiffness is associated with risk of decompensation, liver cancer, and death in patients with chronic liver diseases: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1573–84.e1-2. https://doi.org/10.1016/j.cgh.2013.07.034.
Wang J, Li J, Zhou Q, Zhang D, Bi Q, Wu Y, et al. Liver stiffness measurement predicted liver-related events and all-cause mortality: a systematic review and nonlinear dose-response meta-analysis. Hepatol Commun. 2018;2:467–76. https://doi.org/10.1002/hep4.1154.
Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–97.e10. https://doi.org/10.1053/j.gastro.2015.04.043.
Ciardullo S, Pizzi M, Pizzi P, Oltolini A, Muraca E, Perseghin G. Prevalence of elevated liver stiffness among potential candidates for bariatric surgery in the United States. Obes Surg. 2022;32:712–9. https://doi.org/10.1007/s11695-021-05885-x.
Atallah E, Grove JI, Crooks C, Burden-Teh E, Abhishek A, Moreea S, et al. Risk of liver fibrosis associated with long-term methotrexate therapy may be overestimated. J Hepatol. 2023;78:989–97. https://doi.org/10.1016/j.jhep.2022.12.034.
Das K, Sarkar R, Ahmed SM, Mridha AR, Mukherjee PS, Das K, et al. Normal” liver stiffness measure (LSM) values are higher in both lean and obese individuals: a population-based study from a developing country. Hepatology. 2012;55:584–93. https://doi.org/10.1002/hep.24694.
Wong GL, Chan HL, Choi PC, Chan AW, Lo AO, Chim AM, et al. Association between anthropometric parameters and measurements of liver stiffness by transient elastography. Clin Gastroenterol Hepatol. 2013;11:295–302.e1-3. https://doi.org/10.1016/j.cgh.2012.09.025.
Liu Y, Yuan S, Zuo J, Liu S, Tang X, Li X, et al. A J-shaped relationship between body mass index and the risk of elevated liver stiffness: a cross-sectional study. Eur J Med Res. 2023;28:557 https://doi.org/10.1186/s40001-023-01543-3.
Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27:2015–23. https://doi.org/10.1177/0962280216673085.
Dai H, Li F, Bragazzi NL, Wang J, Chen Z, Yuan H, et al. Distinct developmental trajectories of body mass index and diabetes risk: a 5-year longitudinal study of Chinese adults. J Diabetes Investig. 2020;11:466–74. https://doi.org/10.1111/jdi.13133.
Fan B, Yang Y, Dayimu A, Zhou G, Liu Y, Li S, et al. Body mass index trajectories during young adulthood and incident hypertension: a longitudinal cohort in Chinese population. J Am Heart Assoc. 2019;8:e011937 https://doi.org/10.1161/jaha.119.011937.
Murayama H, Shaw BA. Heterogeneity in trajectories of body mass index and their associations with mortality in old age: a literature review. J Obes Metab Syndr. 2017;26:181–7. https://doi.org/10.7570/jomes.2017.26.3.181.
Wang M, Yi Y, Roebothan B, Colbourne J, Maddalena V, Sun G, et al. Trajectories of body mass index among Canadian seniors and associated mortality risk. BMC Public Health. 2017;17:929 https://doi.org/10.1186/s12889-017-4917-0.
Wu X, Liao J, Chen X, Xiao J, Dui X, Ma T, et al. The independent and combined associations of nocturnal sleep duration, sleep midpoint, and sleep onset latency with global cognitive function in older Chinese adults. Geroscience. 2025; https://doi.org/10.1007/s11357-024-01476-7.
Friedrich-Rust M, Poynard T, Castera L. Critical comparison of elastography methods to assess chronic liver disease. Nat Rev Gastroenterol Hepatol. 2016;13:402–11. https://doi.org/10.1038/nrgastro.2016.86.
Boursier J, Zarski JP, de Ledinghen V, Rousselet MC, Sturm N, Lebail B, et al. Determination of reliability criteria for liver stiffness evaluation by transient elastography. Hepatology. 2013;57:1182–91. https://doi.org/10.1002/hep.25993.
Lim JK, Flamm SL, Singh S, Falck-Ytter YT. American gastroenterological association institute guideline on the role of elastography in the evaluation of liver fibrosis. Gastroenterology. 2017;152:1536–43. https://doi.org/10.1053/j.gastro.2017.03.017.
Jain V, Poddar U, Negi TS, Saraswat VA, Krishnani N, Yachha SK, et al. Utility and accuracy of transient elastography in determining liver fibrosis: a case-control study. Eur J Pediatr. 2020;179:671–7. https://doi.org/10.1007/s00431-019-03561-y.
Serra-Burriel M, Graupera I, Torán P, Thiele M, Roulot D, Wai-Sun Wong V, et al. Transient elastography for screening of liver fibrosis: cost-effectiveness analysis from six prospective cohorts in Europe and Asia. J Hepatol. 2019;71:1141–51. https://doi.org/10.1016/j.jhep.2019.08.019.
Kim BK, Kim SU, Choi GH, Han WK, Park MS, Kim EH, et al. Normal” liver stiffness values differ between men and women: a prospective study for healthy living liver and kidney donors in a native Korean population. J Gastroenterol Hepatol. 2012;27:781–8. https://doi.org/10.1111/j.1440-1746.2011.06962.x.
You SC, Kim KJ, Kim SU, Kim BK, Park JY, Kim DY, et al. Factors associated with significant liver fibrosis assessed using transient elastography in general population. World J Gastroenterol. 2015;21:1158–66. https://doi.org/10.3748/wjg.v21.i4.1158.
Wong VW, Vergniol J, Wong GL, Foucher J, Chan HL, Le Bail B, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology. 2010;51:454–62. https://doi.org/10.1002/hep.23312.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. https://doi.org/10.1146/annurev.clinpsy.121208.131413.
Zhang W, Chen Y, Chen N. Body mass index and trajectories of the cognition among Chinese middle and old-aged adults. BMC Geriatr. 2022;22:613 https://doi.org/10.1186/s12877-022-03301-2.
Wang Y, Li W, Chen S, Zhang J, Liu X, Jiang J, et al. PM(2.5) constituents associated with childhood obesity and larger BMI growth trajectory: a 14-year longitudinal study. Environ Int. 2024;183:108417 https://doi.org/10.1016/j.envint.2024.108417.
van de Schoot R, Sijbrandij M, Winter SD, Depaoli S, Vermunt JK. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct Equ Model. 2017;24:451–67. https://doi.org/10.1080/10705511.2016.1247646.
Nagin DS. Group-based trajectory modeling: an overview. Ann Nutr Metab. 2014;65:205–10. https://doi.org/10.1159/000360229.
Álvarez-Bustos A, Carnicero-Carreño JA, Sanchez-Sanchez JL, Garcia-Garcia FJ, Alonso-Bouzón C, Rodríguez-Mañas L. Associations between frailty trajectories and frailty status and adverse outcomes in community-dwelling older adults. J Cachexia Sarcopenia Muscle. 2022;13:230–9. https://doi.org/10.1002/jcsm.12888.
Azzu V, Vacca M, Virtue S, Allison M, Vidal-Puig A. Adipose tissue-liver cross talk in the control of whole-body metabolism: implications in nonalcoholic fatty liver disease. Gastroenterology. 2020;158:1899–912. https://doi.org/10.1053/j.gastro.2019.12.054.
Unger RH. Lipid overload and overflow: metabolic trauma and the metabolic syndrome. Trends Endocrinol Metab. 2003;14:398–403. https://doi.org/10.1016/j.tem.2003.09.008.
Bijnen M, Josefs T, Cuijpers I, Maalsen CJ, van de Gaar J, Vroomen M, et al. Adipose tissue macrophages induce hepatic neutrophil recruitment and macrophage accumulation in mice. Gut. 2018;67:1317–27. https://doi.org/10.1136/gutjnl-2016-313654.
Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24:908–22. https://doi.org/10.1038/s41591-018-0104-9.
Cuntz U, Voderholzer U. Liver damage is related to the degree of being underweight in anorexia nervosa and improves rapidly with weight gain. Nutrients. 2022;14:2378 https://doi.org/10.3390/nu14122378.
Ichimiya T, Yamakawa T, Hirano T, Yokoyama Y, Hayashi Y, Hirayama D, et al. Autophagy and autophagy-related diseases: a review. Int J Mol Sci. 2020;21:8974 https://doi.org/10.3390/ijms21238974.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96. https://doi.org/10.1016/s0140-6736(09)60318-4.
Winter JE, MacInnis RJ, Nowson CA. The influence of age the BMI and all-cause mortality association: a meta-analysis. J Nutr Health Aging. 2017;21:1254–8. https://doi.org/10.1007/s12603-016-0837-4.
EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237–64. https://doi.org/10.1016/j.jhep.2015.04.006.
Acknowledgements
All authors involved in this study extend their gratitude to the staff of the West China Health and Aging Cohort research team for their dedicated work. We would also like to express our sincere appreciation to Shenzhen Huibo Medical Equipment Co., Ltd. for providing the FibroScan equipment, which was instrumental in conducting liver stiffness measurements and crucial to the success of our study.
Funding
This study was supported by funds from National Key R&D Program of China (2020YFC2006505).
Author information
Authors and Affiliations
Contributions
LLv, LLong, JLi, and JLiao contributed to the study design, data analysis, interpretation, and drafting of the manuscript. YZ, NY, JX, TM, XC, XD, XL, TZ, and HZ contributed to the acquisition of data and critical revision of the manuscript for important intellectual content. JLiao and JLi supervised the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
All participants or their proxy respondents provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lv, L., Long, L., Zheng, Y. et al. A U-shaped relationship between body mass index and the risk of elevated liver stiffness in older people: evidence from the 5‐year retrospective cohort study. Int J Obes 49, 2110–2116 (2025). https://doi.org/10.1038/s41366-025-01849-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01849-8