Abstract
Background/Objective
There is evidence that living with obesity can affect an individual’s pay and employment, but there is little evidence on the impact of weight-management interventions in improving labour market outcomes of individuals. We evaluate the impact of bariatric surgery on monthly earnings and employee status among working-age adults, and examine variations across sociodemographic characteristics.
Methods
This population-based, retrospective longitudinal cohort study for England included 40,662 individuals who had a bariatric surgery procedure and obesity diagnosis between 1 April 2014 and 31 December 2022, with no bariatric surgery history in the previous 5 years, and were 25 to 64 years old at the date of surgery. 49,921 individuals sampled from the general population who had not had bariatric surgery were also included, matched by age and sex. The main outcome measures were monthly employee pay—for all months and only months where the individual was in paid employment—expressed in 2023 prices and paid employee status.
Results
Among people living with obesity who had bariatric surgery, there was a sustained increase in monthly employee pay from 6 months after surgery with a mean increase of £84 per month (95% confidence interval [Cl]: 63–106) 5 years after surgery compared with the 6 months before surgery. There was a sustained increase in the probability of being a paid employee from 4 months after bariatric surgery, with a mean increase of 4.3 percentage points (95% Cl: 3.7–4.9) 5 years after surgery.
Conclusion
Bariatric surgery is associated with an increased probability of being employed, resulting in increased earnings. This suggests that living with obesity negatively impacts labour market outcomes and that obesity management interventions are likely to generate economic benefits both to individuals and on a macroeconomic level by increasing the likelihood of employment of people living with obesity.
Similar content being viewed by others
Introduction
Poor health can affect an individual’s ability to work, impacting on employment, income, productivity, and overall wellbeing [1]. There is some evidence that ill-health can affect labour market outcomes [2], but little evidence on the impact of health interventions in improving labour market outcomes of individuals. Demonstrating the effect of health interventions on economic outcomes could help increase the funding allocated to healthcare for the working age population and the labour market supply, as well as support economic growth.
Prevalence of obesity has been increasing globally [3]. In England, 29% of adults aged 18 years and over were estimated to be living with obesity in 2022 and 64% living with overweight (including obesity) [4]. Obesity is associated with a wide range of chronic conditions, including type 2 diabetes, sleep apnoea, heart failure and hypertension, as well as premature morbidity [5, 6]. The increase in risk of morbidity and mortality with increased BMI is larger among those under 50 years of age [6]. Obesity can affect an individual’s labour market status through generally poorer health, via development of obesity related health conditions or through social discrimination [7]. There is evidence that people living with obesity are less likely to be in paid employment [8], earn less on average than people not living with obesity, particularly among women [9], and have higher levels of sick leave [10, 11]. Therefore, interventions to tackle obesity could improve labour market outcomes.
Bariatric surgery is the most effective obesity intervention for sustained weight-loss [12], leading to lower disease risk, particularly for type 2 diabetes, sleep apnea, nonalcoholic steatohepatitis and hypertension [13, 14]. There is also observational evidence of a beneficial effect across multiple outcomes such as cancer [15] and reduced all-cause mortality [16,17,18]. It is, therefore, an ideal intervention to study the impact of weight-loss on employment. In the 2022–2023 financial year in England, ~4500 bariatric surgical procedures or gastric balloon procedures (not including revision procedures) were carried out [19]. However, there is limited evidence on the impact of bariatric surgery and other obesity care interventions on labour market outcomes. There is significant interest from governments in understanding these impacts, for example in understanding the impacts of weight-loss drugs in the UK [20].
Previous studies have reported inconsistent findings on the impact of bariatric surgery on labour market outcomes; however, these have largely been based on small sample sizes with limited follow-up [21,22,23,24,25,26]. Nationwide studies using register data have been conducted in Scandinavian countries, where linked population-level employment and health datasets are established, and in Belgium using health insurance data. Findings from these studies are inconclusive, with some reporting no changes in employment or earnings and others a positive or negative effect [27,28,29,30].
To our knowledge, no whole population study on the labour market impacts of bariatric surgery has been conducted in the UK. The UK has a publicly funded healthcare system that is free at the point of use. There are high levels of economic inactivity (people neither working nor seeking work) due to long-term ill health, which remains elevated compared with pre-pandemic levels [31]. Therefore, this provides an ideal setting to investigate the labour market impacts of health interventions. We used a population-level linked dataset for England, comprising electronic health records, sociodemographic information, and pay data for employees collected for tax purposes, to evaluate the long-term impact of bariatric surgery on pay and employment. We further examined heterogeneity in effects by sociodemographic characteristics.
Methods
Study data
We used a linked, individual-level dataset for residents of England, combining: (1) Hospital Episode Statistics (HES) Admitted Patient Care (APC) records from 1 April 2009 to 31 December 2022 [32]; (2) sociodemographic characteristics from Census 2011, or from Census 2021 if there was no link for the individual to Census 2011 (10% of individuals had no link to the 2011 Census) [33]; (3) Office for National Statistics (ONS) death registrations for deaths that occurred from 1 January 2014 to 31 December 2022 and were registered by 31 December 2022. [34]; (4) Office for National Statistics (ONS) birth registrations for births that occurred from 1 January 2014 to 31 December 2022 and were registered by 31 December 2023 [35]; (5) Pay As You Earn (PAYE) Real Time Information (RTI) records from His Majesty’s Revenue and Customs (HMRC) covering 1 April 2014 to 31 December 2022. These are records of gross earnings paid to employees and recorded for tax purposes for the UK government, and are calendarised to monthly observations on employee status and pay [36].
The PAYE dataset was linked to the Census 2011 and 2021 through the ONS Demographic Index [37], which contains longitudinally linked administrative data providing information on the population in England and Wales [38, 39]. The HES and death registration datasets were linked to the 2011 Census through the linkage of 2011 Census and NHS Patient Registers 2011–13 and the 2021 Census through the linkage of 2021 Census and 2021 NHS Patient Demographic Service [40]. All datasets were de-identified, prior to being harmonised and analysed.
Study population and follow-up
We included individuals who had at least one episode in HES starting on or after 1 April 2014 and finishing on or before 31 December 2022, recording a primary or secondary Office of Population Censuses and Surveys (OPCS) code for bariatric surgery, concurrently with either a primary International Classification of Diseases (ICD-10) code for obesity or a secondary code for obesity and a primary code for an obesity-related condition (code lists in Supplementary Table 1). Individuals were excluded if they had at least one record in HES for a prior bariatric surgery procedure with episode end from 1 April 2009 and episode start on or before 31 March 2014. The procedure date of each individual’s first episode for bariatric surgery with an obesity diagnosis in the follow-up period was assigned as their index date.
An unexposed sample was created of individuals enumerated in the 2011 Census who did not have a record for bariatric surgery in HES either in the follow-up time (episode end date from 1 April 2014 to 31 December 2022) or in the five years prior. The purpose of this sample was to adjust more accurately for time-varying confounders, which would be partially collinear with the within-individual treatment effect in the exposed cohort. In order to apply the age-based study inclusion criteria to the unexposed cohort, an index date was randomly assigned to individuals in the unexposed sample using the same distribution of operation dates as the bariatric surgery cohort (Supplementary Text 1). The unexposed population was sampled using stratified sampling by sex and five-year age band (for age at index date) to match the age-sex distribution in the bariatric surgery cohort.
We restricted the sample to individuals who could be linked to a valid Census record for at least one of the 2011 or 2021 Censuses, were resident in England and could be linked to at least one encrypted National Insurance number (NINo: the unique ID for each individual with data held by HMRC, including those paid via the PAYE system) and the Patient Registers 2011–13 (for individuals with a 2011 Census ID) or the 2019 Patient Demographic Service (for individuals with a 2021 Census ID) to enable linkage to the HES and deaths datasets. The sample was further restricted to individuals aged 25 to 64 years on the index date and who did not turn 65 of age before the end of that month, to include only individuals of working age and exclude the majority of students.
Individuals were followed up for a maximum of five years pre- and post-surgery, between 1 April 2014 and 31 December 2022 (the calendar time covered by reliable PAYE data for outcomes). Follow-up time was right-censored at the earliest of death or turning age 69, and left-censored before turning age 21, to provide four years of potential follow up time before and after surgery.
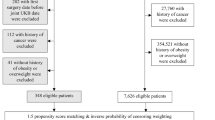
The dataset linking and sample selection process for both exposed and unexposed cohorts is illustrated in Supplementary Fig. 1 and a sample flow is provided in Supplementary Tables 2 and 3.
Exposure and outcome variables
The exposure was time before or after the bariatric surgery procedure, with the 6 months before surgery being the reference period. Exposure time was included as monthly time periods for the month of surgery and the following five months to capture short-term effects after surgery; and as six-monthly periods thereafter to capture long-term effects. The time before surgery was also included in the exposure time variable as six-monthly periods to enable testing for pre-surgery trends. The month in which surgery occurred was defined as exposure month 1. The reference period, to which all time periods were compared, is the six months before surgery (exposure time 0). The exposure time was fixed at 0 for individuals in the unexposed sample.
Two outcomes were analysed: monthly employee pay (numerical: 2023 Sterling values); and paid employee status (numerical: 0/1). Being a paid employee was defined as receiving any monthly pay greater than zero. For the pay outcome, analyses were conducted on both the full dataset (employee pay overall) and on a dataset including only the months for which individuals were a paid employee (employee pay among those in employment).
Information on all variables included in the models is reported in Supplementary Table 4.
Statistical analysis
We described the data using either mean or percentage for a range of sociodemographic variables for the exposed and unexposed individuals, and compared the two groups using standardised mean differences. Standardised mean differences greater than 10% in absolute value indicated a large imbalance between the groups [41].
We compared the unadjusted outcomes (employee pay overall; employee pay among paid employees; paid employee status) over exposure time for the exposed and unexposed individuals. We also compared the unadjusted outcomes over calendar time and age.
We analysed the change in monthly earnings and employee status following surgery, with individuals acting as their own controls. We fitted linear regression models (or linear probability models in the case of employment status as an outcome), with individual-level and calendar-time fixed effects; exposure time was included in the model with a reference level of the six-month period before surgery for the exposed group and all time periods for the unexposed group (Supplementary Text 2). Individual fixed effects capture confounding that does not vary within individuals over time; calendar month-year fixed effects were included as there could be factors which vary over calendar time for all individuals, such as background labour market conditions in the macroeconomy. The model was also adjusted for age in years (on the last day of each month) as a time-varying covariate, to account for changes due to ageing. Age was modelled as a natural cubic spline with four internal knots at the 20th, 40th, 60th and 80th centiles and boundary knots at the 10th and 90th centiles of its distribution; the number of knots was chosen by minimising the BIC.
We estimated robust standard errors accounting for within-individual correlation to accompany the estimated treatment effects, as well as 95% confidence intervals.
Secondary analyses are described in Supplementary Text 3, sensitivity analyses in Supplementary Text 4 and placebo tests in Supplementary Text 5.
All analyses were carried out in R version 3.5.1. Dataset linkage and cleaning was carried out in SparklyR using Spark version 2.4.0. The statistical software package “lfe” version 3.0.0 was used to carry out the fixed effects linear regression modelling.
Results
Characteristics of the study population
We identified 43,968 individuals who had bariatric surgery with a hospital obesity diagnosis during follow-up, with no prior history of bariatric surgery. After restricting to those aged 25–64 years at time of surgery, resident in England and who could link to census and PAYE datasets, 40,662 individuals (92.5%) remained for analysis (Supplementary Table 2). We included a cohort of 49,921 sex- and age-matched individuals in Census 2011 who had not had bariatric surgery (Supplementary Table 3).
The characteristics of the study population are shown in Table 1 (variables are defined in Supplementary Table 4). Individuals who were living with obesity and had bariatric surgery had a mean age of 45 years, 80% were female and 85% were of White ethnicity. Compared with the cohort who had not had bariatric surgery, those who had a bariatric surgery procedure were broadly similar by ethnic group distribution, but were less likely of Asian and more likely of Black ethnicity. The largest differences between the two groups were observed for morbidity measured using the Charlson Comorbidity Score [42, 43] (Supplementary Text 6, Supplementary Table 5), disability, region of residence and area-level socioeconomic deprivation, with people who had bariatric surgery more likely to have a higher burden of morbidity, have a disability and live in more deprived areas.
The overall median follow-up was 88 months, with a maximum of 105 months for both those who had bariatric surgery and those who did not. In those with bariatric surgery, median follow-up time was 48 months pre-surgery and 57 months post-surgery (Supplementary Table 6).
The most common bariatric procedures were Roux-en-Y bypass (20,427; 50.2%) and sleeve gastrectomy (15,329; 37.7%) (Supplementary Table 7). The number of procedures performed each month remained consistent until the COVID-19 pandemic, where large decreases were seen in the number of operations performed (Supplementary Fig. 2).
Unadjusted analyses
The unadjusted analyses do not account for differences between individuals who underwent bariatric surgery and those who did not, such as socioeconomic status, or changes over time such as aging and background economic conditions. Among individuals who underwent bariatric surgery, the employment rate was 56.2% in the pre-surgery and 52.9% in the post-surgery period (Supplementary Table 8). Unadjusted median monthly deflated earnings (with no winsorisation applied) were £1368 in the pre-surgery and £1337 in the post-surgery period; corresponding figures when omitting months for which people were not in work were £2437 and £2528. Earnings and employment rate were higher among those who did not undergo bariatric surgery, with median monthly earnings of £1828 overall and £2901 among those in work only, and an overall employment rate of 64.7%. Employment rate and overall earnings were lower post- than pre-index date, as they were for those who underwent bariatric surgery.
The unadjusted monthly mean deflated employee pay for people who underwent bariatric surgery, overall and among those in work, followed similar trends in exposure time as those for people who did not undergo bariatric surgery. However, there was a reduction in the month of and following the operation for pay overall and among those in work, before a recovery to the pre-operation levels (Fig. 1). There was a similar post-operation drop and recovery in the probability of employment for the people who underwent bariatric surgery. However, there was also a steeper decline in the probability of employment leading up to the operation than the overall decline in the probability of employment seen among the people who did not undergo bariatric surgery. Trends in pay and employment were broadly similar with some small differences by calendar time and age differed slightly between those who had bariatric surgery and those who did not (Supplementary Text 7 and Supplementary Figs. 3 and 4).
Unadjusted mean monthly employee pay and probability of being a paid employee over time before and after surgery for individuals with an obesity diagnosis who underwent bariatric surgery and individuals who did not undergo bariatric surgery 1. Pay is expressed in 2023 prices. 2. Month 0 is the month in which the surgery occurred for the treated cohort and a randomly assigned month for the unexposed sample.
Effect of bariatric surgery on employee pay and paid employee status
Bariatric surgery was associated with a sustained increase in the probability of being a paid employee (Fig. 2; Supplementary Table 9). Compared to pre-surgery level, the probability of being a paid employee decreased by 0.8 (95% Cl: 0.6–1.0) percentage points in the month after surgery, increasing to pre-surgery levels by the third month after the month of surgery. The employment probability then increased by 1.5 (95% Cl: 1.3–1.8) percentage points in months 6–12 after surgery and continued increasing, reaching a maximum of 4.3 (3.7–4.9) percentage points higher than pre-surgery levels in the months 54–60 after surgery. There was evidence of pre-surgery trends, with increased probabilities in the months before surgery compared to the 6 months immediately prior to surgery.
Effect of bariatric surgery on monthly employee pay and probability of being a paid employee before and after surgery 1. Month 0 to 1 is the month in which the surgery occurred for the treated cohort and a randomly assigned month for the unexposed sample. 2. Months -6 to 0 is the reference period to which all other time periods are compared.
Bariatric surgery was associated with a sustained average increase in employee pay, following a short decrease in pay in the first few months following surgery. Compared with the pre-surgery levels, employee earnings decreased in the month after surgery by an average of £117 (95% Cl: 110–124), before increasing to pre-surgery levels by the fourth month after surgery (Fig. 2; Supplementary Table 10). Compared to the six months before surgery, employee pay then increased to £61 (95% Cl: 49–72) more than pre-surgery levels in months 18–24 after surgery, and continued to gradually increase compared to the six months before surgery to £84 (63–106) more than pre-surgery levels in months 54–60 after surgery. There were no pre-surgery trends for employee pay overall.
By contrast, bariatric surgery was not strongly associated with an increase in pay among those in work, where only the months in which individuals were in paid employment were included in the analysis (Fig. 2; Supplementary Table 11). Pay among those in work initially decreased in the month after surgery, by an average of £206 (95% Cl: 194–218) compared with pre-surgery levels, before increasing to pre-surgery levels by the fifth month after surgery. However, employee pay among those in work remained only slightly above or the same as pre-surgery levels in the following months, with a maximum of £21 (95% Cl: 6–36) more than pre-surgery levels in months 18–24 after surgery.
There were no pre-surgery trends for employee pay overall and only a very small, possible downward trend in the pre-surgery trends for employee pay among those in work.
Secondary analyses
For most of the treatment interactions investigated, the overall trends were broadly similar for each group, with an initial decrease followed by an increase in employee pay and probability of paid employment and no change in pay among those in paid employment (Supplementary Text 3, Supplementary Figs. 5–22 and Supplementary Table 12). There was a higher increase in pay and probability of paid employment after bariatric surgery among those who had a higher burden of morbidity, however pretrends make the interpretation of the pay outcome in particular more challenging.
Sensitivity analyses
Results from sensitivity analysis looking at the impact of the timing and length of the reference period were consistent with the findings of the main analysis (Supplementary Text 4 and Supplementary Tables 13–18). There were slightly higher estimates of the association of surgery with the probability of being a paid employee when omitting data from the COVID-19 pandemic period, starting from 12 months after surgery (Supplementary Table 19). Results from placebo tests supported the robustness of the analysis method (Supplementary Text 5 and Supplementary Figs. 23 and 24).
Discussion
Main findings
In this nationwide study in England, we found that bariatric surgery led to an increase in the probability of employment sustained from four months to five years after surgery (the end of the follow-up period). Individuals were on average 3.7 percentage points more likely to be in paid employment 1–5 years after surgery, reaching a maximum of 4.3 percentage points more likely to be in paid employment 54 to 60 months after surgery. This was also reflected in overall earnings: The total average cumulative increase in pay over 5 years after surgery was £3180, which is a substantial part of the cost of surgery [44]. however, there was little change in pay among only those in paid employment after the initial decrease, suggesting that the increase in pay was largely driven by the increased likelihood of being in paid employment, rather than changes in the rate of pay or hours worked.
The higher probability of being in paid employment after surgery, leading to increased overall pay, is likely to be driven by intentional weight-loss maintenance as a result of having had bariatric surgery, leading to an increase in general health, a lower likelihood of developing obesity related conditions, lower levels of social discrimination or stigma [45], or a combination of these factors. This either enables individuals who had left the workforce to return or decreases the rate at which individuals are leaving the workforce. The secondary analysis showing that the increase in probability of paid employment after bariatric surgery is larger among individuals with a higher burden of morbidity supports better health being a driver of the improvements in economic outcomes.
Comparison with other studies
There is substantial evidence that a higher BMI is associated with lower pay, lower probability of employment, and high levels of sickness leave [8,9,10,11]. However, evidence for the effect of bariatric surgery on these outcomes is more limited, often based on smaller sample sizes [21,22,23,24,25,26]. A UK based study of 1011 bariatric surgery patients found an increase in employment post-surgery [25]. However, follow-up was limited to 30 months and no comparison group who had not undergone bariatric surgery was included. To our knowledge, four nationwide, registry-based studies on the labour market effects of bariatric surgery have been carried out, with none in the UK. In Sweden, no change in pay or employment was observed over the 5 years after surgery (15,828 individuals who underwent bariatric surgery) [27]; in Denmark, an increased probability of being in full-time employment 1–3 years after surgery was found but not in the longer term. There was a sustained increase in the probability of being in full-time employment for men, craftsmen and office workers (5450 individuals who underwent bariatric surgery) [28]. The third study, also conducted in Denmark, showed a lower risk of unemployment 5 years after surgery among men, but a higher risk in women and a higher risk of sickness absence up to 5 years after surgery in both men and women (10,328 individuals who underwent bariatric surgery) [30]. A fourth study, in Belgium, found higher levels of employment 3 years after bariatric surgery (16,276 individuals who underwent bariatric surgery) [29].
Contrary to the Scandinavian registry-based studies, we found a sustained increase in employment after bariatric surgery in both men and women; however, we did not observe a change in pay among those in employment. Some differences could be related to the national differences in healthcare or the labour market and welfare system.
Strengths and limitations of this study
To our knowledge, this is the largest population-wide study of labour market outcomes of bariatric surgery internationally, and the only such study outside of Scandinavia and Belgium. This investigation was made possible by a new national linked dataset comprising electronic health records, sociodemographic information and monthly pay records, which is the first linked dataset containing labour market and health data with near-complete coverage for individuals in England.
We did not have reliable data on hours worked, therefore we could not distinguish changes in hours worked from changes in rate of pay. In addition, individuals who were self-employed were not included in the PAYE dataset and would be classed as not a paid employee in our analysis, along with people who were employed but not receiving pay (for example, due to maternity leave or sick leave). We also did not have information on benefits received, such as sick leave and disability benefit, which could be impacted by having bariatric surgery [26].
We used a sample of people from the general population who had not undergone bariatric surgery to better account for time-varying confounding, independently of the effect of bariatric surgery. There were large differences between those who underwent bariatric surgery and those who did not for some sociodemographic characteristics, such as area-level socioeconomic deprivation, with a higher proportion of people who underwent bariatric surgery living in more deprived areas than in the general population. This may have contributed to the pre-surgery trends seen in some subgroups. An unexposed group constructed of the population eligible for bariatric surgery, but who did not undergo surgery, using information such as BMI (not available for this analysis) could be used as a comparison group, which may enable time-varying confounders (i.e., calendar time and ageing) to be better accounted for.
Bariatric surgery is highly effective, making it an ideal intervention to study the impact of weight-loss on employment outcomes. However, only a small percentage of the population eligible for bariatric surgery receive it, and the population who do differs from those eligible but who do not receive bariatric surgery [46]. Further studies of alternative obesity care interventions, such as pharmaceutical interventions and weight-management programmes, are needed to enable comparisons between different interventions and employment outcomes.
The impact of bariatric surgery on economic outcomes is one of the factors to consider when appraising the impacts, positive and negative, of the procedure, alongside impacts to individual’s health, changes to future healthcare utilisation and potential complications. However, the impact of bariatric surgery on an individual’s economic outcomes are not usually considered when calculating cost-effectiveness [47, 48], or are estimated based on strong assumptions [12, 24, 49]. Estimates such as those produced by this analysis will aid in providing a more complete picture of the impact of bariatric surgery, supporting more robust health-economic appraisal [50].
Conclusions
In our study, bariatric surgery resulted in a sustained increase in the probability of being a paid employee from four months after surgery over the five-year follow-up period, leading to increased earnings. This suggests that living with obesity negatively impacts labour market outcomes and obesity care interventions are likely to generate substantial economic benefits by increasing earnings and employment of people living with obesity, mediated by intentional weight-loss maintenance due to having had bariatric surgery [51].
Data availability
The source data used in this study is subject to controlled access due to its sensitive nature.
Code availability
The code used for the analysis is available on Github [52].
References
Department for Work and Pensions, Department of Health and Social Care. A study of work and health transitions: analysis of Understanding Society [Internet]. 2021. Available from: https://www.gov.uk/government/publications/a-study-of-work-and-health-transitions-analysis-of-understanding-society/a-study-of-work-and-health-transitions-analysis-of-understanding-society#key-findings
Pintor MP, Fumagalli E, Sukrcke M. The impact of health on labour market outcomes: a rapid systematic review. Health Policy (New York). 2024;143. 105057.
Phelps NH, Singleton RK, Zhou B, Heap RA, Mishra A, Bennett JE, et al. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403:1027–50.
NHS England. Health Survey for England, 2022 Part 2. Adult overweight and obesity. 2024. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2022-part-2/adult-overweight-and-obesity
Haase CL, Eriksen KT, Lopes S, Satylganova A, Schnecke V, McEwan P. Body mass index and risk of obesity-related conditions in a cohort of 2.9 million people: evidence from a UK primary care database. Obes Sci Pract. 2021;7:137–147.
Bhaskaran K, dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol [Internet]. 2018;6:944–53.
Dolado JJ, Minale L, Guerra A. Uncovering the roots of obesity-based wage discrimination: the role of job characteristics. Labour Econ [Internet]. 2023;85:102425.
Campbell DD, Green M, Davies N, Demou E, Ward J, Howe LD, et al. Effects of increased body mass index on employment status: a Mendelian randomisation study. Int J Obes [Internet]. 2021;45:1790–801.
Han E, Norton EC, Stearns SC. Weight and wages: fat versus lean paychecks. Health Econ. 2009;18:535–48.
Cawley J. An economy of scales: a selective review of obesity’s economic causes, consequences, and solutions. J Health Econ [Internet]. 2015;43:244–68.
Bramming M, Jorgensen MB, Christensen AI, Lau CJ, Egan KK, Tolstrup JS. BMI and labor market participation : a cohort study of transitions between work, unemployment, and sickness absence. Obesity. 2019;27:1703–10.
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation [Internet]. Vol. 13, Health Technology Assessment. 2009. Available from: https://www.journalslibrary.nihr.ac.uk/hta/hta13410/#/abstract
Noria SF, Grantcharov T. Biological effects of bariatric surgery on obesity-related comorbidities. Can J Surg. 2013;56:47–57.
Fakhry TK, Mhaskar R, Schwitalla T, Muradova E, Gonzalvo JP, Murr MM. Bariatric surgery improves nonalcoholic fatty liver disease: a contemporary systematic review and meta-analysis. Surg Obes Relat Dis. 2019;15:502–511.
Wilson RB, Lathigara D, Kaushal D. Systematic review and meta-analysis of the impact of bariatric surgery on future cancer risk. Int J Mol Sci. 2023;24:6192.
Wiggins T, Guidozzi N, Welbourn R, Ahmed AR, Markar SR. Association of bariatric surgery with all-cause mortality and incidence of obesity-related disease at a population level: a systematic review and meta-analysis. PLoS Med [Internet]. 2020;17:1–18.
Syn NL, Cummings DE, Wang LZ, Lin DJ, Zhao JJ, Loh M, et al. Association of metabolic–bariatric surgery with long-term survival in adults with and without diabetes: a one-stage meta-analysis of matched cohort and prospective controlled studies with 174 772 participants. Lancet. 2021;397:1830–41.
Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement [Internet]. Vol. 8, Health Technology Assessment. 2004 Jan. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673605177186
NHS England. National Obesity Audit - Primary Bariatric Surgical Procedures [Internet]. [cited 2024 Oct 2]. Available from: https://app.powerbi.com/view?r=eyJrIjoiOTIwMGU5YzctOTQ1OC00NTg4LWEwNzEtY2I0MWY1YzNkZWNmIiwidCI6IjM3YzM1NGIyLTg1YjAtNDdmNS1iMjIyLTA3YjQ4ZDc3NGVlMyJ9
BBC. Unemployed could get weight loss jabs to return to work [Internet]. Available from: https://www.bbc.co.uk/news/articles/cjd54zd0ezjo
Alfonso-cristancho R, King WC, Mitchell JE, Ramanathan R, Sullivan SD, Belle SH, et al. Longitudinal evaluation of work status and productivity after bariatric surgery. JAMA. 2017;316:1595–7.
Andersen JR, Hernæs UJ V, Hufthammer KO, Villy V. Employment status and sick-leave following obesity surgery: a five-year prospective cohort study. PeerJ. 2015;1–12.
Turchiano M, Saunders JK, Fernandez G, Navie L, Labrador L, Parikh M. Bariatric surgery may improve employment status in unemployed, underserved, severely obese patients. Obes Surg. 2014;24:692–5.
Tarride JE, Breau R, Sharma AM, Hong D, Gmora S, Guertin JR, et al. The effect of bariatric surgery on mobility, health-related quality of life, healthcare resource utilization, and employment status. Obes Surg [Internet]. 2017;27:349–56.
Courtney MJ, Mahawar K, Burnell P, Jennings N, Balupuri S, Schroeder N, et al. Occupational outcomes of obesity surgery—do the employed return to work, and do the unemployed find work? Obes Surg. 2018;28:963–9.
Hawkins SC, Osborne A, Finlay IG, Alagaratnam S, Edmond J, Welbourn R. Paid work increases and state benefit claims decrease after bariatric surgery. Obes Surg. 2007;17:434–437.
Norrbäck M, Neovius M, Ottosson J, Näslund I, Bruze G. Earnings and work loss from 5 years before to 5 years after bariatric surgery: a cohort study. PLoS One. 2023;18:1–13.
Juhl CB, Holst R, Mundbjerg LH, Stolberg C, Gran JM, Thomsen GF. Effect of bariatric surgery on employment status — a 7 years controlled nationwide registry study. BMJ Open. 2021:1–10.
Van den Eynde A, De Cock D, Fabri V, Kestens W, Di Zinno T, Brabant S, et al. Back to work after bariatric surgery? A belgian population study. Obes Surg [Internet]. 2022;32:2625–31.
Bramming M, Becker U, Jørgensen MB, Neermark S, Bisgaard T, Tolstrup JS. Bariatric surgery and risk of unemployment and sickness absence. Obes Surg. 2022;32:720–8.
Office for National Statistics. LFS: Econ. inactivity reasons: Long Term Sick: UK: 16-64:000s:SA [Internet]. 2024 [cited 2024 Oct 2]. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peoplenotinwork/economicinactivity/timeseries/lf69/lms
NHS Digital. Hospital Episode Statistics (HES) [Internet]. [cited 2024 Apr 30]. Available from: https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics
Office for National Statistics. Census [Internet]. Available from: https://www.ons.gov.uk/census
Office for National Statistics. User guide to mortality statistics [Internet]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/methodologies/userguidetomortalitystatisticsjuly2017
Office for National Statistics. User guide to birth statistics. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/methodologies/userguidetobirthstatistics
Office for National Statistics. Monthly earnings and employment estimates from Pay As You Earn Real Time Information (PAYE RTI) data: methods [Internet]. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/methodologies/monthlyearningsandemploymentestimatesfrompayasyouearnrealtimeinformationpayertidatamethods
Office for National Statistics. 2011 Census linkage to DWP master key and encrypted NINo [Internet]. (2024). Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/methodologies/2011censuslinkagetodwpmasterkeyandencryptednino
Archer R, Kenning E, Lloyd S, Vellanki P, Groom P, Ankeru S, et al. Evaluating Statistical Quality in the Demographic Index [Internet]. Available from: https://uksa.statisticsauthority.gov.uk/wp-content/uploads/2023/02/EAP182-Quality-work-for-Demographic-Index-MDQA.pdf
Office for National Statistics. Reference Data Management Framework [Internet]. Available from: https://www.ons.gov.uk/aboutus/whatwedo/programmesandprojects/referencedatamanagementframework
Office for National Statistics. Census 2021 to Personal Demographics Service linkage report [Internet]. (2023). Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/methodologies/census2021topersonaldemographicsservicelinkagereport
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
NHS England. National Cost Collection Data Publication: National Schedule 2022/23 [Internet]. p. Admitted Patient Care. Available from: https://app.powerbi.com/view?r=eyJrIjoiOTQwZjIwMjUtNDgwMi00MThmLWJhM2MtNmM5YWY2MTkwM2M4IiwidCI6IjM3YzM1NGIyLTg1YjAtNDdmNS1iMjIyLTA3YjQ4ZDc3NGVlMyJ9
Rooth DO. Obesity, attractiveness, and differential treatment in hiring. J Hum Resour. 2009;44:710–35.
Coulman KD, Margelyte R, Jones T, Blazeby JM, Macleod J, Owen-Smith A, et al. Access to publicly funded weight management services in England using routine data from primary and secondary care (2007–2020): an observational cohort study. PLoS Med [Internet]. 2023;20:1–29.
Boyers D, Retat L, Jacobsen E, Avenell A, Aveyard P, Corbould E, et al. Cost-effectiveness of bariatric surgery and non-surgical weight management programmes for adults with severe obesity: a decision analysis model. Int J Obes. 2021;45:2179–2190.
Gulliford MC, Charlton J, Booth HP, Fildes A, Khan O, Reddy M, et al. Costs and outcomes of increasing access to bariatric surgery for obesity: cohort study and cost-effectiveness analysis using electronic health records. Heal Serv Deliv Res. 2016;4:1–120.
Office of Health Economics. Shedding the pounds: Obesity management, NICE guidance and bariatric surgery in England [Internet]. 2010. Available from: https://www.ohe.org/publications/shedding-pounds-obesity-management-nice-guidance-and-bariatric-surgery-england/
McLaughlin J, Rejon CS, Bell M, Schwander B, Coulman K, McLeod H. Holistic modelling as a catalyst for effective obesity policy. BMJ. 2024;386:e077139.
Department of Health and Social Care. Summary letter from Lord Darzi to the Secretary of State for Health and Social Care [Internet]. 2024. Available from: https://www.gov.uk/government/publications/independent-investigation-of-the-nhs-in-england/summary-letter-from-lord-darzi-to-the-secretary-of-state-for-health-and-social-care
Office for National Statistics. ONS-Health-modelling-hub/bariatric_surgery_lmo [Internet]. Available from: https://github.com/ONS-Health-modelling-hub/bariatric_surgery_lmo
Acknowledgements
KK is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM), NIHR Global Research Centre for Multiple Long Term Conditions, NIHR Cross NIHR Collaboration for Multiple Long Term Conditions, NIHR Leicester Biomedical Research Centre (BRC) and the British Heart Foundation (BHF) Centre of Excellence. JV is supported by the NIHR Applied Research Collaboration North West London, and by CW + , the official charity of Chelsea and Westminster Hospital NHS Foundation Trust. KDC, receives funding from The NIHR Bristol Biomedical Research Centre (BRC-1215-20011) at University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS, or the UK Department of Health and Social Care.
Funding
This work was funded by the Labour Markets Evaluation and Pilots Fund (2024 to 2025) and the Office for National Statistics.
Author information
Authors and Affiliations
Contributions
DA and VN conceived and designed the study. TD prepared the deidentified datasets for linking. CRB, carried out the analysis. CRB, DA, FZ, KDC, JV, KK, DJP, RS, NI, CR and VN contributed to discussions on the methods and the interpretation of the results, which shaped the analysis. CRB drafted the manuscript. CRB, DA, FZ, KDC, JV, KK, DJP, RS, NI, CR and VN revised the manuscript and approved the final version to be submitted. VN is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
FZ has received consulting fees from Servier, Menarini, and Daiichi Sankyo, unrelated to this study, as well as honoraria from the European Association for the Study of Diabetes for providing methodological support in the development of clinical guidelines, also not related to this study. KK has acted as a consultant, speaker or received grants for investigator-initiated studies for Astra Zeneca, Bayer, Novo Nordisk, Sanofi-Aventis, Servier, Lilly and Merck Sharp & Dohme, Boehringer Ingelheim, Oramed Pharmaceuticals, Pfizer, Roche, Daiichi-Sankyo, Applied Therapeutics, Embecta and Nestle Health Science. DP has been funded by the Royal College of Surgeons of England. He receives consulting fees from Johnson and Johnson, GSK, Novo Nordisk and Pfizer and payments for lectures, presentations, and educational events from Johnson and Johnson, Medtronic, Novo Nordisk and Sandoz. JV was the national clinical director for diabetes and obesity at NHS England from April 2013 to September 2023.
Ethics approval
Ethical approval was obtained from the National Statistician’s Data Ethics Advisory Committee (NSDEC23[18]). All methods were performed in accordance with the relevant guidelines and regulations. This study does not include experiments involving human participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bermingham, C.R., Ayoubkhani, D., Zaccardi, F. et al. Impact of bariatric surgery on monthly earnings and employment: a national linked data study in England, 2014–2022. Int J Obes (2026). https://doi.org/10.1038/s41366-025-01995-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41366-025-01995-z