Abstract
Vascular dysfunction has been shown to negatively impact physical function, with arterial stiffening being linked to worsening balance function. Estimated pulse wave velocity (ePWV), derived from age and blood pressure (BP), is an emerging method of assessing vascular function that can be widely used in large, observational studies. Whether ePWV is associated with balance function in US adults remains unknown. A total of 3276 adult men and women from the 2021–2023 National Health and Nutrition Examination Survey who completed BP and balance function measures were included in this study. Balance function was assessed using the Modified Romberg Test of Standing Balance on Firm and Compliant Support Surfaces (MRT). ePWV was used to assess vascular function and derived from a regression equation using age and mean blood pressure. A general linear model was then used to determine whether ePWV is significantly associated with the number of MRT conditions passed. The model showed that, after covarying for age, systolic BP, diastolic BP, gender, race/ethnicity, educational attainment, socioeconomic status, alcohol, smoking, body mass index, and physical activity levels, ePWV was significantly and inversely related to the number of MRT conditions passed (β = −0.398, p < 0.001). Higher ePWV is associated with worsened balance control in a nationally representative sample of US adults. As ePWV only requires age and BP, measures that are taken routinely at physical examinations, future studies should longitudinally examine associations between ePWV and balance function in a clinical setting.
Similar content being viewed by others
Introduction
Vascular dysfunction is a robust facilitator for disability and functional impairment in adults [1,2,3,4]. Arterial stiffness has been linked to end-target organ damage due to increased pulsatile hemodynamics [5,6,7], which may negatively impact physical function (i.e., gait speed, muscular power) and morbidity in adults [1, 3, 4]. Specifically, deficits in balance function is a major risk factor for falls and subsequent disability [8, 9], with failure during the Modified Romberg Test of Standing Balance on Firm and Compliant Support Surfaces (assesses balance function) associated with at least a 2x increased risk for a fall in the past year [10]. Over 14 million adults in the United States (US) report falling each year [9], with accidental falls being the leading cause of injury and injury-related deaths among older adults in the US [8]. Thus, accessible methods to determine vascular health and balance function are needed for widespread screening to reduce disability and morbidity in the US adult population.
Recent studies have supported the link between arterial stiffness and balance function. Systolic hypertension is associated with worsened postural stability in older adults [11], while higher carotid-femoral pulse wave velocity (cfPWV), a measure for central arterial stiffness, is significantly associated with worsened postural control in older adults [12]. Furthermore, as vascular remodeling begins in early adulthood [13], vascular links to balance control are not limited to older adults such that vascular contributions to worsening balance control may begin in young adulthood. Likewise, we previously showed that carotid-femoral pulse wave velocity (cfPWV) independently predicts postural sway in 112 young adults (18–35 years old) [14], indicating that arterial stiffening may influence balance control throughout adulthood. However, even with these clinically important findings, it is acknowledged that the limited number of participants and narrow age range hinder the generalization of our findings. To address these limitations, we sought to use population data from the National Health and Nutrition Examination Survey (NHANES) and assess vascular function via estimated pulse wave velocity (ePWV), derived from age and blood pressure [15], which can be widely used in large, observational studies. Whether ePWV is associated with balance function remains unknown.
Therefore, the purpose of this study is to examine whether ePWV, an emerging measure of vascular aging, is associated with balance function in a nationally representative sample of US adults from NHANES. It is hypothesized that higher ePWV will be significantly associated with worsened balance function in US adults.
Methods
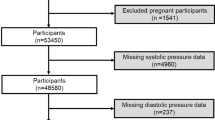
Study design
Data for this cross-sectional study were obtained from the 2021–2023 NHANES cycle. NHANES is a nationally representative survey of the civilian, non-institutionalized US population. NHANES sample selection utilizes a complex, stratified, multistage probability design to eliminate potential selection bias. All methods utilized in the NHANES protocol were approved by the National Center for Health Statistics Research Ethics Review Board and all participants provided informed consent. All methods were performed in accordance with relevant guidelines and regulations. The data for this study and the descriptions for the study procedures are publicly available online at https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?Cycle=2021-2023. The 2021–2023 NHANES dataset includes 12,592 participants. Participants were excluded from this analysis if they were <18 years or ≥65 years old (n = 7025). Participants who did not attempt at least one trial for the Modified Romberg Test of Standing Balance on Firm and Compliant Support Surfaces, had missing blood pressure (BP) data, or had invalid physical activity data (n = 2291) were excluded from the final analysis. Final analyses were performed on 3276 US adult men and women. As the sample size for the present study was determined based on existing data from the 2021–2023 NHANES cycle, a priori sample size calculations were not conducted. However, post-hoc power analysis (G*Power v3.1) demonstrated that the current sample size (n = 3276) achieved a statistical power of >99%.
Estimated pulse wave velocity
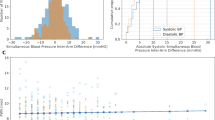
Brachial systolic (SBP) and diastolic blood pressure (DBP) measurements were taken using an electronic, oscillometric BP measurement device with an appropriately sized cuff in the seated position following a quiet 5-min rest (Omron HEM-907XL). Three consecutive measures were completed 60 s apart, with SBP and DBP averaged across all three measures. Mean arterial pressure (MAP) was then calculated as [DBP + ((0.4)(SBP–DBP))]. ePWV was subsequently calculated based on age and MAP using the following algorithm [16]: 9.587–(0.402*age) + (4.560*0.001*age2)–(2.261*0.00001*age2*MAP) + (3.176*0.001*MAP)–(1.832*0.01*MAP). It should be noted that while MAP is traditionally calculated as [DBP + (1/3)(SBP–DBP)], a form factor of 0.4 has been shown to be more closely association with end-target organ damage [16, 17]. As such, this method for calculating MAP is the standard for studies exploring the association of ePWV with clinical outcomes and is in agreement with the Reference Values for Arterial Stiffness Collaboration [16,17,18,19,20,21].
Balance function
Balance function was assessed using the Modified Romberg Test of Standing Balance on Firm and Compliant Support Surfaces (MRT). Detailed descriptions for MRT procedures are provided on the NHANES website (https://wwwn.cdc.gov/Nchs/Data/Nhanes/Public/2021/DataFiles/BAX_L.htm). In summary, the MRT assesses an individual’s ability to stand unassisted in five different conditions: (1) bare floor with eyes open, (2) bare floor with eyes closed, (3) dense foam surface with eyes open, (4) dense foam surface with eyes closed, and (5) dense foam surface with eyes closed while moving head slowly from side-to-side. Participants were given two trials to pass the requisite time interval for each condition. For conditions 1 and 2, a time interval of 15 s was considered passing, and for conditions 3 through 5, a time interval of 20 s was considered passing. Participants who did not complete the time interval for the requisite condition on both trials were considered to be failed. Participants were then reported as having passed or failed the MRT condition, and pass/fail status was reported for all five conditions.
Covariates for ePWV and balance function
Potential covariates for the relationship between ePWV and balance function included age (years), gender (male/female), race/ethnicity (Mexican American, other Hispanic, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian, other race/multiracial), educational attainment (highest grade or level of school completed, or the highest degree achieved), socioeconomic status (SES; ratio of family income to poverty level), alcohol consumption (average number of alcoholic beverages per day in the last year, included as a covariate due to high alcohol consumption having inverse relations with arterial stiffness and postural stability [22, 23]), smoking status (whether or not participant had smoked 100 cigarettes in their lifetime [yes/no]), body mass index (BMI; weight-to-height ratio as kg/m2) and self-reported leisure-time moderate-to-vigorous physical activity levels (MVPA; minutes per week) [24].
Statistical analysis
We performed all analyses by adjusting for the complex, multistage survey sampling design of NHANES. Descriptive statistics are reported using both unweighted (mean ± standard deviation (SD) and n, %) and weighted (mean ± standard error (SE) and frequency, %) results. The association between ePWV and the number of MRT conditions passed was assessed using bivariate two-tailed Pearson correlation coefficient. A general linear model was then used to determine whether ePWV was significantly associated with the number of MRT conditions passed. Two general linear models were performed: (1) unadjusted and (2) adjusted for the constituent components of ePWV (age, SBP, and DBP) and additional covariates including gender, race/ethnicity, educational attainment, SES, alcohol, smoking, BMI, and MVPA. We also included an adjusted model without age, SBP, or DBP to account for potential issues of multicollinearity with ePWV. Additional general linear models stratified by gender were performed to account for potential gender differences in ePWV and balance function. All statistical analyses were performed using IBM SPSS Statistics version 28 (SPSS Inc., Chicago, IL) and statistical significance was set a priori at p < 0.05.
Results
Participant characteristics
Participant characteristics are presented in Table 1. Participants in our cohort ranged in age from 20–64 years old, with 70.7% being overweight or obese and 26.7% having hypertension. We had an approximately even split between male and female participants (male = 50.5%, female = 49.4%), with most participants being NH White (57.5%). For the MRT conditions, 0.2% of participants did not pass any conditions, 0.4% passed one condition, 0.4% passed two conditions, 12.2% passed three conditions, 29.5% (passed four conditions, and 57.3% passed all five conditions.
Association between ePWV and balance function
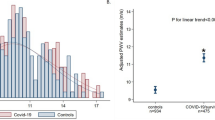
Higher ePWV was significantly associated with a lower number of MRT conditions passed (r = −0.293, p < 0.001). Table 2 presents results from the general linear model evaluating the relationship between ePWV and the number of MRT conditions passed. Unadjusted analysis showed that ePWV was significantly and inversely associated with the number of MRT conditions passed, with ePWV accounting for 8.6% of the variance in the number of MRT conditions passed (Estimate = −0.146 [95% CI: −0.166–−0.126], p < 0.001). Adjusted analysis included age, SBP, and DBP, gender, race/ethnicity, educational attainment, SES, alcohol consumption, smoking, BMI, and MVPA. The overall fit of the model was statistically significant, with the model accounting for 15.2% of the variance in the number of MRT conditions passed. ePWV remained inversely and significantly associated with the number of MRT conditions passed (Estimate = −0.248 [95% CI: −0.385–−0.110], p = 0.002), while SBP, DBP, SES, educational attainment, and alcohol consumption were also significant contributors to the overall model fit (p < 0.05). Finally, to address potential issues of multicollinearity between ePWV and its components, we removed age, SBP, and DBP from the general linear model. The removal of these variables did not change our overall results, as the overall fit of the model remained statistically significant (R2 = 0.124), with ePWV being inversely and significantly associated with the number of MRT conditions passed (Estimate = −0.148 [95% CI: −0.179–−0.118], p < 0.001). Educational attainment, smoking, and alcohol consumption were also significant contributors to the overall model fit (p < 0.05). Results from adjusted analysis without age, SBP, and DBP are shown in Supplementary Table S1.
Sex-specific analysis
We previously found that female sex was inversely related to balance function in young adults [14]; therefore, we also ran separate unadjusted and adjusted analyses for males and females. In this study, we found consistent results between males and females, in that ePWV was significantly associated with the number of MRT conditions passed in unadjusted and adjusted analyses for both sexes. In unadjusted analysis, ePWV was significantly and inversely related to the number of MRT conditions passed (males: estimate = −0.121 [95% CI: −0.166–−0.077], p < 0.001; females estimate = −0.169 [95% CI: −0.192–−0.146], p < 0.001). In adjusted analysis for age, SBP, and DBP, race/ethnicity, educational attainment, SES, alcohol consumption, smoking, BMI, and MVPA; ePWV remained inversely and significantly associated with the number of MRT conditions passed for both males and females (males: −0.350 [95% CI: −0.557–−0.143], p = 0.003; females: estimate = −0.199 [95% CI: −0.294–−0.105], p < 0.001). Results from sex-specific analysis are shown in Supplementary Table S2.
Discussion
The present study utilized a nationally representative dataset of the US population to investigate whether vascular function is associated with balance function in US adults. To pursue our study aim, we utilized useful and reliable tools for measuring vascular aging (ePWV) and balance function (MRT), which are applicable to this population-based study [15, 16]. We found that ePWV was inversely related to the number of MRT conditions passed. In both unadjusted and adjusted models, higher ePWV was significantly associated with a lower number of MRT conditions passed, with these findings consistent in both males and females. Overall, these findings suggest that higher ePWV is associated with worsened balance control in US adult men and women, and that ePWV may provide novel insight into the relationship between vascular aging and balance function.
Findings from the present study support the emerging literature connecting vascular aging with worsened balance function. Previous research regarding the association between vascular aging and balance function has been limited to connecting balance function with clinical CVD outcomes, such as stroke and chronic heart failure [25, 26]. Balance disorders have been found to predict CVD mortality [24], while balance function is significantly impaired following CVDs and cerebrovascular diseases [25,26,27]. More recently, studies have begun focusing on pre-clinical markers of CVD risk to relate vascular aging to balance function in older adults. Turusheva et al. [28] found that a higher cardio-ankle vascular index, a novel measure of whole-body arterial stiffness, was related to an increased risk for a fall-related injury in older adults (OR: 3.52, 95% CI: 1.03–12.04); while Peultier-Celli et al. [12] found that higher cfPWV was associated with worsened postural control among older adults in both eyes open and eyes closed conditions (p < 0.05 for both conditions). Together, these findings indicate that older adults with higher arterial stiffness may have more difficulty with balance control and thus an increased likelihood for fall-related injuries. We previously [14] observed that increased Mobil-O-Graph PWV significantly predicted a larger postural sway during the eyes closed standing on a foam surface condition in young adults, even after adjustment for measures of physical fitness (standardized β = 0.44, p = 0.009). The findings from our present study further extend upon these previous findings by revealing that increased ePWV is inversely associated with the number of conditions passed on the MRT in a nationally representative sample of young- and middle-aged US adults.
Potential mechanisms for the contribution of vascular aging to worsened balance function include increases in hemodynamic pulsatility due to arterial stiffness, leading to damage to the structures governing balance function [7, 29,30,31]. Balance function is governed by a complex set of sensorimotor systems. Inputs from visual, proprioceptive, and vestibular systems are integrated by the central nervous system, which then sends signals to the musculoskeletal system to control motor output [31]. Arterial stiffening has been linked to end-target organ damage due to increased pulsatile hemodynamics [6], and the sensorimotor structures governing balance function could be particularly vulnerable to these consequences of arterial stiffening. Hemodynamic pulsatility due to arterial stiffening may lead to damage of the retinal arterioles, cerebrovasculature, and arteries feeding the inner ear [7, 29, 30], potentially causing injury to the visual, proprioceptive, and vestibular structures responsible for balance control, leading to a worsening of balance function. Indeed, cross-sectional studies have found that higher arterial stiffness is associated with damage to the aforementioned sensorimotor structures [7, 29, 30], even in young- to middle-aged adults [29], supporting these potential mechanisms connecting arterial stiffness to balance function.
Furthermore, the findings from the present study suggest that the clinical utility of ePWV extends beyond CVD outcomes, providing valuable insight into physical functioning. ePWV is a well-established independent predictor for all-cause mortality and clinical CVD outcomes [16, 19, 20, 32], with improvements in ePWV via antihypertensive interventions even predicting lower risk for all-cause mortality in the Systolic Blood Pressure Intervention Trial [33]. Recently, associations for ePWV have also been connected to cognitive vascular aging, with ePWV being related to cognitive performance and the incidence of dementia in older adults [17, 18]. Although cognitive performance and vascular dementia are associated with worsened balance function [34,35,36], the connection between ePWV and balance function had yet to be explored. To our knowledge, the present study is the first to associate ePWV with a measure of physical function. We found that, even after adjustment for the constituent components of the ePWV equation and additional confounders, ePWV was significantly associated with the number of conditions passed on the MRT. These findings suggest that ePWV provides insight into the relationship between vascular aging and balance function. Additionally, we found that these significant associations were consistent in both males and females. Our observations of significant associations between ePWV and balance function across genders, as well as the practicality of ePWV due to only requiring age and BP, suggests that ePWV may be a useful clinical tool for general practitioners to identify men and women with poor balance control who may be at a high risk for falls and fall-related injuries.
Limitations
Due to the nature of population datasets, unbalanced samples (i.e., for age, race) may limit the generalizability of our findings. The cross-sectional study design means that causality and temporality between ePWV and balance function cannot be inferred from these findings. NHANES also uses questionnaire data for the sociodemographic and physical activity variables, subjecting our findings to recall and response bias. Finally, although we did not use the gold standard measure of arterial stiffness (cfPWV), ePWV has been shown to significantly predict all-cause mortality, major CVD events, and cerebrovascular events independently of traditional CVD risk factors (including cfPWV) [15, 19, 20, 32] and may be a more appropriate and practical measure for providing insight into vascular aging in large, epidemiological studies due to only requiring age and BP.
Conclusion
In conclusion, we found that increased ePWV is associated with worsened balance control in US adult men and women. As ePWV only requires age and BP, measures that are regularly taken during routine physical examinations, it may be an accessible and practical tool for general practitioners to identify individuals at a high risk for balance disorders, falls, and fall-related injuries. Future research should explore ePWV as a potential target for interventions aimed at improving balance control and lowering fall risk among US adults.
Summary
What is known about this topic?
-
Vascular dysfunction has been shown to negatively impact indices of physical function, such as gait speed and muscular power, in adults.
-
Recent studies have supported a link between arterial stiffness and balance function, with higher carotid-femoral pulse wave velocity associated with worsened postural control in older adults and higher postural sway in younger adults.
-
Estimated pulse wave velocity (ePWV) is an independent predictor for all-cause mortality and clinical CVD outcomes, and is associated with worsening cognitive performance and dementia.
What this study adds
-
This study found that higher ePWV is associated with worse balance control in US adult men and women, suggesting ePWV may provide novel insight into the relationship between vascular aging and balance function.
-
The present study adds to existing literature by suggesting that the clinical utility of ePWV extends beyond CVD outcomes, potentially providing valuable insight into physical functioning.
Data availability
The data for this study and the descriptions for the study procedures are publicly available online at https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?Cycle=2021-2023.
References
Dorff A, Bradford C, Hunsaker A, Atkinson J, Rhees J, Leach OK, et al. Vascular dysfunction and the age-related decline in critical power. Exp. Physiol. 2024;109:240–54.
De Lima EP, Tanaka M, Lamas CB, Quesada K, Detregiachi CRP, Araújo AC, et al. Vascular impairment, muscle atrophy, and cognitive decline: critical age-related conditions. Biomedicines. 2024;12:2096.
Heffernan KS, Chalé A, Hau C, Cloutier GJ, Phillips EM, Warner P, et al. Systemic vascular function is associated with muscular power in older adults. J. Aging Res. 2012;2012:386387.
Heffernan KS, Manini TM, Hsu F-C, Blair SN, Nicklas BJ, Kritchevsky SB, et al. Relation of pulse pressure to long-distance gait speed in community-dwelling older adults: findings from the LIFE-P study. PLoS ONE. 2012;7:e49544.
Vasan RS, Short MI, Niiranen TJ, Xanthakis V, DeCarli C, Cheng S, et al. Interrelations between arterial stiffness, target organ damage, and cardiovascular disease outcomes. J. Am. Heart Assoc. 2019;8:e012141.
Scuteri A, Morrell CH, Fegatelli DA, Fiorillo E, Delitala A, Orru M, et al. Arterial stiffness and multiple organ damage: a longitudinal study in population. Aging Clin. Exp. Res. 2020;32:781–8.
Poels MM, Zaccai K, Verwoert GC, Vernooij MW, Hofman A, van der Lugt A, et al. Arterial stiffness and cerebral small vessel disease: the Rotterdam Scan Study. Stroke. 2012;43:2637–42.
Kakara R, Bergen G, Burns E, Stevens M. Nonfatal and fatal falls among adults aged ≥65 years - United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 2023;72:938–43.
Colón-Emeric CS, McDermott CL, Lee DS, Berry SD. Risk assessment and prevention of falls in older community-dwelling adults: a review. Jama. 2024;331:1397–406.
Agrawal Y, Carey JP, Hoffman HJ, Sklare DA, Schubert MC. The modified romberg balance test: normative data in U.S. adults. Otol. Neurotol. 2011;32:1309–11.
Hausdorff JM, Herman T, Baltadjieva R, Gurevich T, Giladi N. Balance and gait in older adults with systemic hypertension. Am. J. Cardiol. 2003;91:643–5.
Peultier-Celli L, Lion A, Buatois S, Watfa G, Gueguen R, Benetos A, et al. Relation of arterial stiffness with postural control in older people. Eur. Geriatr. Med. 2021;12:871–9.
Agbaje AO. Arterial stiffness precedes hypertension and metabolic risks in youth: a review. J. Hypertens. 2022;40:1887–96.
Cilhoroz BT, Heckel AR, DeBlois JP, Keller A, Sosnoff JJ, Heffernan KS. Arterial stiffness and augmentation index are associated with balance function in young adults. Eur. J. Appl. Physiol. 2023;123:891–9.
Greve SV, Laurent S, Olsen MH. Estimated pulse wave velocity calculated from age and mean arterial blood pressure. Pulse. 2017;4:175–9.
Greve SV, Blicher MK, Kruger R, Sehestedt T, Gram-Kampmann E, Rasmussen S, et al. Estimated carotid-femoral pulse wave velocity has similar predictive value as measured carotid-femoral pulse wave velocity. J. Hypertens. 2016;34:1279–89.
Heffernan KS, Wilmoth JM, London AS. Estimated pulse wave velocity is associated with a higher risk of dementia in the health and retirement study. Am. J. Hypertens. 2024;37:909–15.
Heffernan KS, Stoner L, Meyer ML, Loprinzi PD. Association between estimated pulse wave velocity and cognitive performance in older Black and White adults in NHANES. J. Alzheimers Dis. 2022;88:985–93.
Jae SY, Heffernan KS, Kurl S, Kunutsor SK, Laukkanen JA. Association between estimated pulse wave velocity and the risk of stroke in middle-aged men. Int. J. Stroke. 2021;16:551–5.
Laugesen E, Olesen KKW, Peters CD, Buus NH, Maeng M, Botker HE, et al. Estimated pulse wave velocity is associated with all‐cause mortality during 8.5 years follow‐up in patients undergoing elective coronary angiography. J. Am. Heart Assoc. 2022;11:e025173.
Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur. Heart J. 2010;31:2338–50.
Rosenbloom MJ, Rohlfing T, O’Reilly AW, Sassoon SA, Pfefferbaum A, Sullivan EV. Improvement in memory and static balance with abstinence in alcoholic men and women: selective relations with change in brain structure. Psychiatry Res. 2007;155:91–102.
Del Giorno R, Maddalena A, Bassetti S, Gabutti L. Association between alcohol intake and arterial stiffness in healthy adults: a systematic review. Nutrients. 2022;14:1207.
Cao C, Cade WT, Li S, McMillan J, Friedenreich C, Yang L. Association of balance function with all-cause and cause-specific mortality among US Adults. JAMA Otolaryngol. Head. Neck Surg. 2021;147:460–8.
Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. Bmj. 1995;311:83–6.
Ozcan EB, Saglam M, Vardar-Yagli N, Calik-Kutukcu E, Inal-Ince D, Altinsoy M, et al. Impaired balance and gait characteristics in patients with chronic heart failure. Heart Lung Circ. 2022;31:832–40.
Manemann SM, Chamberlain AM, Boyd CM, Miller DM, Poe KL, Cheville A, et al. Fall risk and outcomes among patients hospitalized with cardiovascular disease in the community. Circ. Cardiovasc. Qual. Outcomes. 2018;11:e004199.
Turusheva A, Frolova E, Kotovskaya Y, Petrosyan Y, Dumbadze R. Association between arterial stiffness, frailty and fall-related injuries in older adults. Vasc. Health Risk Manag. 2020;16:307–16.
Holwerda SW, Kardon RH, Hashimoto R, Full JM, Nellis JK, DuBose LE, et al. Aortic stiffness is associated with changes in retinal arteriole flow pulsatility mediated by local vasodilation in healthy young/middle-age adults. J. Appl. Physiol. 2020;129:84–93.
Huang Y, Yuan Y, Wang Y, Hui Z, Shang X, Chen Y, et al. Effects of blood pressure and arterial stiffness on retinal neurodegeneration: cross-sectional and longitudinal evidence from UK Biobank and Chinese cohorts. Hypertension. 2023;80:629–39.
Peterka RJ. Sensory integration for human balance control. Handb. Clin. Neurol. 2018;159:27–42.
Cheng W, Kong F, Pan H, Luan S, Yang S, Chen S. Superior predictive value of estimated pulse wave velocity for all-cause and cardiovascular disease mortality risk in U.S. general adults. BMC Public. Health. 2024;24:600.
Vlachopoulos C, Terentes-Printzios D, Laurent S, Nilsson PM, Protogerou AD, Aznaouridis K, et al. Association of estimated pulse wave velocity with survival: a secondary analysis of SPRINT. JAMA Netw. Open. 2019;2:e1912831.
Kim HJ, Jeong S, Oh YH, Suh MJ. Association of balance impairment with risk of incident dementia among older adults. J. Of. Prev. Alzheimer’s Dis. 2024;11:130–7.
Yan J, Luan F, Wang M, Dong W, Zhang X, Li M, et al. Prospective association between standing balance and cognitive function in middle-aged and older Chinese adults. Front. Psychol. 2022;13:931216.
Moretti R, Torre P, Antonello RM, Esposito F, Bellini G. Gait and equilibrium in subcortical vascular dementia. Curr. Gerontol. Geriatr. Res. 2011;2011:263507.
Funding
No financial assistance was received to support this study.
Author information
Authors and Affiliations
Contributions
ARH: Writing – review & editing, Writing – original draft, Formal Analysis, Visualization, Conceptualization. ACG: Writing – review & editing, Visualization, Formal analysis, Conceptualization. WC: Writing – review & editing, Writing – original draft, Visualization, Formal analysis, Conceptualization. JYK: Writing – review & editing, Supervision, Project administration, Conceptualization.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heckel, A.R., Glasgow, A.C., Cho, W. et al. The association between estimated pulse wave velocity and balance function in U.S. adults. J Hum Hypertens 39, 764–769 (2025). https://doi.org/10.1038/s41371-025-01062-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01062-0