Abstract
Objective
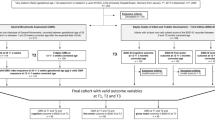
To apply automated movement analysis to the general movements assessment (GMA) to build a predictive model for motor impairment (MI).
Study design
A retrospective cohort study including infants ≤306/7 weeks GA or BW ≤1500 g seen at 3–5 months was conducted. Automated video analysis was used to develop a multivariable model to identify MI, defined as Bayley motor composite score <85 or cerebral palsy (CP).
Results
One hundred and fifty two videos were analyzed. Median GA and BW were 275/7 weeks and 955 g, respectively. MI and CP rates were 22% (N = 33) and 14% (N = 22). Minimum, mean, and mean vertical velocity of the infant’s silhouette correlated significantly with MI. Sensitivity, specificity, positive and negative predictive values, and accuracy of automated GMA were 79%, 63%, 37%, 91%, and 66%, respectively. C-statistic indicated good fit (C = 0.77).
Conclusions
Automated movement analysis predicts MI in preterm infants. Further refinement of this technology is required for clinical application.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Adde L, Helbostad JL, Jensenius AR, Taraldsen G, Støen R. Using computer-based video analysis in the study of fidgety movements. Early Hum Dev. 2009;85:541–7.
Kanemaru N, Watanabe H, Kihara H, Nakano H, Takaya R, Nakamura T, et al. Specific characteristics of spontaneous movements in preterm infants at term age are associated with developmental delays at age 3 years. Dev Med Child Neurol. 2013;55:713–21.
Karch D, Kim KS, Wochner K, Pietz J, Dickhaus H, Philippi H. Quantification of the segmental kinematics of spontaneous infant movements. J Biomech. 2008;41:2860–7.
Philippi H, Karch D, Kang KS, Wochner K, Pietz J, Dickhaus H, et al. Computer-based analysis of general movements reveals stereotypies predicting cerebral palsy. Dev Med Child Neurol. 2014;56:960–7.
Stephens BE, Vohr BR. Neurodevelopmental outcome of the premature infant. Pedia Clin North Am. 2009;56:631–46. Table of Contents
Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev. 2015;24:CD005495.
Herskind A, Greisen G, Nielsen JB. Early identification and intervention in cerebral palsy. Dev Med Child Neurol. 2015;57:29–36.
Morgan C, Darrah J, Gordon AM, Harbourne R, Spittle A, Johnson R, et al. Effectiveness of motor interventions in infants with cerebral palsy: a systematic review. Dev Med Child Neurol. 2016;58:900–9.
Himmelmann K. Epidemiology of cerebral palsy. In: Dulac O, Lassonde M, Sarnat H editors. ML OD, BS H, editors. Handbook of clinical neurology. vol. 111, Ch. 15. London: Elsevier; 2013. p. 163–7.
Ashwal S, Russman BS, Blasco PA, Miller G, Sandler A, Shevell M, et al. Practice parameter: diagnostic assessment of the child with cerebral palsy: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2004;62:851–63.
Bosanquet M, Copeland L, Ware R, Boyd R. A systematic review of tests to predict cerebral palsy in young children. Dev Med Child Neurol. 2013;55:418–26.
Darsaklis V, Snider LM, Majnemer A, Mazer B. Predictive validity of Prechtl’s Method on the Qualitative Assessment of General Movements: a systematic review of the evidence. Dev Med Child Neurol. 2011;53:896–906.
Novak I, Morgan C, Majnemer A, Boychuk Z, Payton C, Msall M, et al., editors. Early detection and diagnosis of high-risk of cerebral palsy and cerebral palsy: International recommendations. American Academy for Cerebral Palsy and Developmental Medicine Annual Meeting; September 2016.
Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, et al. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 2017;171:897–907.
Spittle AJ, Boyd RN, Inder TE, Doyle LW. Predicting motor development in very preterm infants at 12 months’ corrected age: the role of qualitative magnetic resonance imaging and general movements assessments. Pediatrics. 2009;123:512–7.
Spittle AJ, Spencer-Smith MM, Cheong JL, Eeles AL, Lee KJ, Anderson PJ, et al. General movements in very preterm children and neurodevelopment at 2 and 4 years. Pediatrics. 2013;132:e452–8.
Sustersic B, Sustar K, Paro-Panjan D. General movements of preterm infants in relation to their motor competence between 5 and 6 years. Eur J Paediatr Neurol. 2012;16:724–9.
Noble Y, Boyd R. Neonatal assessments for the preterm infant up to 4 months corrected age: a systematic review. Dev Med Child Neurol. 2012;54:129–39.
Spittle AJ, Cameron K, Doyle LW, Cheong JL, Group VICS. Motor impairment trends in extremely preterm children: 1991–2005. Pediatrics 2018;141:e20173410.
Einspieler C, Prechtl HF. Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment Retard Dev Disabil Res Rev. 2005;11:61–7.
Stahl A, Schellewald C, Stavdahl Ø, Aamo OM, Adde L, Kirkerød H. An optical flow-based method to predict infantile cerebral palsy. IEEE Trans Neural Syst Rehabil Eng. 2012;20:605–14.
Støen R, Songstad NT, Silberg IE, Fjørtoft T, Jensenius AR, Adde L. Computer-based video analysis identifies infants with absence of fidgety movements. Pediatr Res. 2017;82:665–70.
Einspieler C, Prechtl H, Bos A, Ferrari F, Cioni G. Prechtl’s method on the qualitative assessment of general movements in preterm, term and young infants (inl. CD-ROM). London: MacKeith Press, distributed by Cambridge University Press; 2004.
Brox T, Malik J. Large displacement optical flow: descriptor matching in variational motion estimation. IEEE Trans Pattern Anal Mach Intell. 2011;33:500–13.
Orlandi S, Raghuram K, Smith CR, Mansueto D, Church P, Shah V, et al. Detection of atypical and typical infant movements using computer-based video analysis 40th annual international conference of the IEEE Engineering in Medicine and Biology Society; Honolulu, HI2018.
Kanemaru N, Watanabe H, Kihara H, Nakano H, Nakamura T, Nakano J, et al. Jerky spontaneous movements at term age in preterm infants who later developed cerebral palsy. Early Hum Dev. 2014;90:387–92.
Spittle AJ, Spencer-Smith MM, Eeles AL, Lee KJ, Lorefice LE, Anderson PJ, et al. Does the Bayley-III Motor Scale at 2 years predict motor outcome at 4 years in very preterm children? Dev Med Child Neurol. 2013;55:448–52.
Bayley N. Bayley Scales of infant and toddler development. Administration manual. 3rd ed. San Antonio, TX: Pearson; 2006.
Bayley N. Bayley Scales of infant and toddler development. Technical manual. 3rd ed. San Antonio, TX: Harcourt Assessment Inc; 2006.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2016;102:F235–F234.
Austin PC, Tu JV. Automated variable selection methods for logistic regression produced unstable models for predicting acute myocardial infarction mortality. J Clin Epidemiol. 2004;57:1138–46.
Austin P, Tu J. Bootstrap methods for developing predictive models. Am Stat. 2004;58:131–7.
Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87.
Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd ed. New Jersey: John Wiley & Sons; 2013.
Hadders-Algra M. General movements: a window for early identification of children at high risk for developmental disorders. J Pediatr. 2004;145(2 Suppl.):S12–8.
van Dyk J, Church P, Dell S, To T, Luther M, Shah V. Prediction of long-term neurodevelopmental outcome in preterm infants using trajectories of general movement assessments. J Perinatol. 2018;38:1398–406.
Einspieler C, Marschik PB, Pansy J, Scheuchenegger A, Krieber M, Yang H, et al. The general movement optimality score: a detailed assessment of general movements during preterm and term age. Dev Med Child Neurol. 2016;58:361–8.
Kwong AKL, Fitzgerald TL, Doyle LW, Cheong JLY, Spittle AJ. Predictive validity of spontaneous early infant movement for later cerebral palsy: a systematic review. Dev Med Child Neurol. 2018;60:480–9.
Einspieler C, Prechtl HF, Ferrari F, Cioni G, Bos AF. The qualitative assessment of general movements in preterm, term and young infants-review of the methodology. Early Hum Dev. 1997;50:47–60.
Prechtl HF. Qualitative changes of spontaneous movements in fetus and preterm infant are a marker of neurological dysfunction. Early Hum Dev. 1990;23:151–8.
Harrell F. Regression modeling strategies with applications to linear models, logistic regression, and survival analysis. New York, NY: Springer; 2001.
Adde L, Helbostad J, Jensenius AR, Langaas M, Støen R. Identification of fidgety movements and prediction of CP by the use of computer-based video analysis is more accurate when based on two video recordings. Physiother Theory Pract. 2013;29:469–75.
Spittle AJ, Olsen J, Kwong A, Doyle LW, Marschik PB, Einspieler C, et al. The Baby Moves prospective cohort study protocol: using a smartphone application with the General Movements Assessment to predict neurodevelopmental outcomes at age 2 years for extremely preterm or extremely low birthweight infants. BMJ Open. 2016;6:e013446.
Acknowledgements
The authors gratefully acknowledge all the members of the PRISM laboratory at Holland Bloorview Kids Rehabilitation Hospital for providing us with guidance and equipment for the study. We also acknowledge all the members of the Neonatal Follow-up Clinic at Sunnybrook for assisting with this project. This Project is partially supported by Brain Canada Foundation through the Canada Brain Research Fund, with the financial support of Health Canada and the funding partners.
Funding
This project is partially supported by Brain Canada Foundation through the Canada Brain Research Fund, with the financial support of Health Canada and their funding partners.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raghuram, K., Orlandi, S., Shah, V. et al. Automated movement analysis to predict motor impairment in preterm infants: a retrospective study. J Perinatol 39, 1362–1369 (2019). https://doi.org/10.1038/s41372-019-0464-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-019-0464-0
This article is cited by
-
Towards novel classification of infants’ movement patterns supported by computerized video analysis
Journal of NeuroEngineering and Rehabilitation (2024)
-
A 3D pose estimation framework for preterm infants hospitalized in the Neonatal Unit
Multimedia Tools and Applications (2023)
-
Novel AI driven approach to classify infant motor functions
Scientific Reports (2021)