Abstract
Background
Bronchopulmonary Dysplasia (BPD) is the most common prematurity complication. Although several practices have been proposed for BPD prevention, none of these in isolation prevent BPD.
Methods
Our initiative focused on two key drivers: oxygen management and noninvasive ventilation strategies. We created best practice guidelines and followed outcome measures using Shewhart control charts.
Results
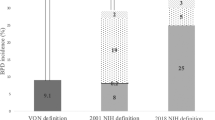
PDSAs of protocols preceded a large-scale rollout of a “0.21 by 28” campaign in 2014 leading to a special cause reduction in the “any BPD” rate, and a decrease in severe BPD (from 57 to 29%). At the end of 2017, we reinvigorated the project, which led to dramatic decreases in the “any BPD” rate to 41% and the “severe BPD” rate to 21%.
Conclusions
A multidisciplinary QI initiative focused on process improvement geared towards the pathophysiological contributors of BPD has successfully reduced the rate of BPD in an all referral level IV NICU.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Northway WH Jr., Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N. Engl J Med. 1967;276:357–68.
Doyle LW, Anderson PJ. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14:391–5.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Walsh MC, Szefler S, Davis J, Allen M, Van Marter L, Abman S, et al. Summary proceedings from the bronchopulmonary dysplasia group. Pediatrics. 2006;117:S52–6.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. J Am Med Assoc. 2015;314:1039–51.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Abman SH, Collaco JM, Shepherd EG, Keszler M, Cuevas-Guaman M, Welty SE, et al. Interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr. 2017;181:12–28 e1.
Zysman-Colman Z, Tremblay GM, Bandeali S, Landry JS. Bronchopulmonary dysplasia—trends over three decades. Paediatr Child Health. 2013;18:86–90.
Shepherd EG, Knupp AM, Welty SE, Susey KM, Gardner WP, Gest AL. An interdisciplinary bronchopulmonary dysplasia program is associated with improved neurodevelopmental outcomes and fewer rehospitalizations. J Perinatol. 2012;32:33–8.
Nankervis CA, Martin EM, Crane ML, Samson KS, Welty SE, Nelin LD. Implementation of a multidisciplinary guideline-driven approach to the care of the extremely premature infant improved hospital outcomes. Acta Paediatr. 2010;99:188–93.
Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines; Graham R, Mancher M, Miller Wolman D, et al., editors. Clinical Practice Guidelines We Can Trust. Washington (DC): National Academies Press (US); 2011. 6, Promoting Adoption of Clinical Practice Guidelines. Available from: https://www.ncbi.nlm.nih.gov/books/NBK209543/.
Brilli RJ, Allen S, Davis JT. Revisiting the quality chasm. Pediatrics. 2014;133:763–5.
Brilli RJ, Crandall WV, Berry JC, Stoverock L, Rosen K, Budin L, et al. A patient/family-centered strategic plan can drive significant improvement. Adv Pediatr. 2014;61:197–214.
Langley GJ. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Francisco: Jossey-Bass; 2009.
Murthy K, Porta NFM, Lagatta JM, Zaniletti I, Truog WE, Grover TR, et al. Inter-center variation in death or tracheostomy placement in infants with severe bronchopulmonary dysplasia. J Perinatol. 2017;37:723–7.
Wheeler TA, Davis JT, Brilli RJ. The aggregate point rule for identifying shifts on P charts and U charts. Pediatr Qual Saf. 2018;3:e103.
Nist MD, Rodgers EA, Ruth BM, Bertoni CB, Bartman T, Keller LA, et al. Skin rounds: a quality improvement approach to enhance skin care in the neonatal intensive care unit. Adv Neonatal Care. 2016;16 Suppl 5S :S33–41.
Doyle LW, Carse E, Adams AM, Ranganathan S, Opie G, Cheong JLY, et al. Ventilation in extremely preterm infants and respiratory function at 8 years. N Engl J Med. 2017;377:329–37.
Nelin LD, Bhandari V. How to decrease bronchopulmonary dysplasia in your neonatal intensive care unit today and “tomorrow”. F1000Res. 2017;6:539.
Jobe AH. The new BPD. NeoReviews. 2006;7:e531–45.
Wai KC, Kohn MA, Ballard RA, Truog WE, Black DM, Asselin JM, et al. Early cumulative supplemental oxygen predicts bronchopulmonary dysplasia in high risk extremely low gestational age newborns. J Pediatr 2016;177:97–102 e2.
Lennox L, Maher L, Reed J. Navigating the sustainability landscape: a systematic review of sustainability approaches in healthcare. Implement Sci. 2018;13:27.
Keller RL, Eichenwald EC, Hibbs AM, Rogers EE, Wai KC, Black DM, et al. The randomized, controlled trial of late surfactant: effects on respiratory outcomes at 1-year corrected age. J Pediatr. 2017;183:19–25 e2.
Ballard RA, Keller RL, Black DM, Ballard PL, Merrill JD, Eichenwald EC, et al. Randomized trial of late surfactant treatment in ventilated preterm infants receiving inhaled nitric oxide. J Pediatr. 2016;168:23–9 e4.
Stevens TP, Dylag A, Panthagani I, Pryhuber G, Halterman J. Effect of cumulative oxygen exposure on respiratory symptoms during infancy among VLBW infants without bronchopulmonary dysplasia. Pediatr Pulmonol. 2010;45:371–9.
Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2016:CD001243. https://doi.org/10.1002/14651858.CD001243.pub3.
Fischer HS, Buhrer C. Avoiding endotracheal ventilation to prevent bronchopulmonary dysplasia: a meta-analysis. Pediatrics. 2013;132:e1351–60.
Robbins M, Trittmann J, Martin E, Reber KM, Nelin L, Shepherd E. Early extubation attempts reduce length of stay in extremely preterm infants even if re-intubation is necessary. J Neonatal Perinat Med. 2015;8:91–7.
Author information
Authors and Affiliations
Contributions
RB, ES, LN, GR, and TB conceptualized and designed the study, coordinated and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. AE designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bapat, R., Nelin, L., Shepherd, E. et al. A multidisciplinary quality improvement effort to reduce bronchopulmonary dysplasia incidence. J Perinatol 40, 681–687 (2020). https://doi.org/10.1038/s41372-019-0574-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-019-0574-8
This article is cited by
-
Decreasing early invasive mechanical ventilation exposure in preterm infants: a quality improvement initiative
Journal of Perinatology (2025)
-
Managing established bronchopulmonary dysplasia without using routine blood gas measurements
Journal of Perinatology (2024)
-
Epigenetic modifications in the development of bronchopulmonary dysplasia: a review
Pediatric Research (2024)
-
Synergistic effects of achieving perinatal interventions on bronchopulmonary dysplasia in preterm infants
European Journal of Pediatrics (2024)
-
Advancements in neonatology through quality improvement
Journal of Perinatology (2022)