Abstract
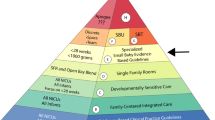
Survival and outcomes for extremely premature (EP) infants have improved and even infants born at 23 and 24 weeks that were previously considered non-viable are now routinely surviving. This review describes our particular institution’s basis for and process of creating and sustaining a small baby program for a quaternary, referral-based neonatal intensive care unit. Through multi-disciplinary collaboration, small baby guidelines were developed that established uniform care and optimized evidence-based practice for the care of this unique patient population. A focus on parent-centered care while removing noxious stimuli for the patient has improved neurodevelopmental outcomes. Data collection, quality improvement, and ongoing research are incorporated in the small baby program to establish and sustain best practices and outcomes for the EP patient. Through the establishment of a small baby unit, we have improved survival, decreased short-term morbidities, and improved neurodevelopmental outcomes for the EP infant in our region.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Norman M, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004–2007 and 2014–2016. JAMA. 2019;321:1188–99.
Stoll BJ, et al. Neonatal outcomes of extremely preterm infants from the NICHD neonatal research network. Pediatrics. 2010;126:443–56.
Backes CH, et al. A proactive approach to neonates born at 23 weeks of gestation. Obstet Gynecol. 2015;126:939–46.
Backes CH, et al. Outcomes following a comprehensive versus a selective approach for infants born at 22 weeks of gestation. J Perinatol. 2019;39:39–47.
Brilli RJ, et al. The preventable harm index: an effective motivator to facilitate the drive to zero. J Pediatr. 2010;157:681–3.
Doerfler ME, et al. Methods for reducing sepsis mortality in emergency departments and inpatient units. Jt Comm J Qual Patient Saf. 2015;41:205–11.
James D, Pennardt AM. Trauma care principles. StatPearls. 2020. Treasure Island, FL.
Nankervis CA, et al. Implementation of a multidisciplinary guideline-driven approach to the care of the extremely premature infant improved hospital outcomes. Acta Paediatr. 2010;99:188–93.
Shah PS, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr. 2016;177:144–52. e6
Smith LK, et al., An international comparison of death classification at 22 to 25 weeks’ gestational age. Pediatrics, 2018;142.
Schneider K, et al. End-of-life decisions 20 years after EURONIC: neonatologists’ self-reported practices, attitudes, and treatment choices in Germany, Switzerland, and Austria. J Pediatr. 2019;207:154–60.
Merritt TA, Gold M, Holland J. A critical evaluation of clinical practice guidelines in neonatal medicine: does their use improve quality and lower costs?. J Eval Clin Pract. 1999;5:169–77.
Boundy EO, et al. Kangaroo Mother Care and Neonatal Outcomes: A Meta-analysis. Pediatrics. 2016;137:e20152238. https://doi.org/10.1542/peds.2015-2238.
Nyqvist KH. et al. Towards universal Kangaroo mother care: recommendations and report from the first European conference and seventh international workshop on Kangaroo mother care. Acta Paediatr. 2010;99:820–6.
Gonya J, et al. Empowerment programme for parents of extremely premature infants significantly reduced length of stay and readmission rates. Acta Paediatr. 2014;103:727–31.
Ment LR, et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics. 1994;93:543–50.
Nelin TD, et al. Outcomes following indomethacin prophylaxis in extremely preterm infants in an all-referral NICU. J Perinatol. 2017;37:932–7.
Pishevar N, et al. Predicting survival in infants born at <27 weeks gestation admitted to an all referral neonatal intensive care unit: a pilot study. J Perinatol. 2020;40:750–7.
Ezenwa B, et al. Effects of practice change on outcomes of extremely preterm infants with patent ductus arteriosus. Acta Paediatr. 2019;108:88–93.
Robbins M, et al. Early extubation attempts reduce length of stay in extremely preterm infants even if re-intubation is necessary. J Neonatal Perinat Med. 2015;8:91–7.
Moorehead PA, et al. Factors associated with survival of <27 week infants in an all-referral neonatal intensive care unit. J Neonatal Perinat Med. 2012;5:105–11.
Trittmann JK, Nelin LD, Klebanoff MA. Bronchopulmonary dysplasia and neurodevelopmental outcome in extremely preterm neonates. Eur J Pediatr. 2013;172:1173–80.
Coccia C, et al. Management of extremely low-birth-weight infants. Acta Paediatr Suppl. 1992;382:10–2.
Kastenberg ZJ, et al. Effect of deregionalized care on mortality in very low-birth-weight infants with necrotizing enterocolitis. JAMA Pediatr. 2015;169:26–32.
O’Callaghan N, Dee A, Philip RK. Evidence-based design for neonatal units: a systematic review. Matern Health Neonatol Perinatol. 2019;5:6.
Pineda RG, et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J Pediatr. 2014;164:52–60. e2
Gonya J, et al. Human interaction in the NICU and its association with outcomes on the brief infant-toddler social and emotional assessment (BITSEA). Early Hum Dev. 2018;127:6–14.
Erdei C, et al. The growth and development unit. A proposed approach for enhancing infant neurodevelopment and family-centered care in the neonatal intensive care unit. J Perinatol. 2019;39:1684–7.
Cong X, et al. The impact of cumulative pain/stress on neurobehavioral development of preterm infants in the NICU. Early Hum Dev. 2017;108:9–16.
Acknowledgements
The authors would like to thank all of the providers from the various disciplines that have coalesced around a unifying goal of improving outcomes in our most vulnerable patients. From its inception to today, the growth and success of the Small Baby Program at Nationwide Children’s Hospital would not be possible without such a selfless and collaborative effort. Furthermore, we want to recognize and thank all our patients and their families, from whom we learn every day.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
OF, LDN, and EGS have no conflicts of interest to declare. KMR is a Board Member of the Children’s Hospital Neonatal Consortium and receives financial compensation in this role.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fathi, O., Nelin, L.D., Shepherd, E.G. et al. Development of a small baby unit to improve outcomes for the extremely premature infant. J Perinatol 42, 157–164 (2022). https://doi.org/10.1038/s41372-021-00984-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-00984-0
This article is cited by
-
Neonatal intensive care unit discharge education interventions and their effects on maternal sensitivity and neurocognitive development of premature infants: a protocol for a systematic review
Systematic Reviews (2025)
-
Blood cultures and predicting positivity in extremely preterm infants admitted to an outborn level IV NICU
BMC Pediatrics (2025)
-
It’s the little things. A framework and guidance for programs to care for infants 22–23 weeks’ gestational age
Journal of Perinatology (2025)
-
Double Jeopardy: A Distinct Mortality Pattern Among Preterm Infants with Congenital Heart Disease
Pediatric Cardiology (2025)
-
A pivotal moment in the evolution of neonatal care
Journal of Perinatology (2023)