Abstract
Subgaleal hemorrhages (SH) involve bleeding in the expansive compartment between the periosteum of the skull and the galea aponeurotica. The potentially rapid accumulation of blood in this space is responsible for the clinical severity, as neonates with SH can present with acute hypovolemia, shock and multiorgan failure. SH is associated with instrumented delivery, especially with use of vacuum extraction. Although infrequent, the incidence of SH has not decreased over the past several decades, despite improvements in obstetrical care. Management of severe SH is complex and requires cardiovascular support, management of co-existent encephalopathy, and most importantly correction of coagulopathy and anemia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Malmstrom T. Vacuum extractor, an obstetrical instrument. Acta Obstet Gynecol Scand Suppl. 1954;33:1–31.
Plauche WC. Subgaleal hematoma. A complication of instrumental delivery. JAMA. 1980;244:1597–8.
Christensen R, Baer V, Henry E, Christensen R. Neonatal subgaleal hemorrhage in a multihospital healthcare system: prevalence, associations, and outcomes. e-J Neonatol Res. 2011;1:1–8.
Greer FR. Vitamin K deficiency and hemorrhage in infancy. Clin Perinatol. 1995;22:759–77.
Moorehead PC, Chan AKC, Lemyre B, Winikoff R, Scott H, Hawes SA, et al. A practical guide to the management of the fetus and newborn with hemophilia. Clin Appl Thromb Hemost. 2018;24:29S–41S.
Govaert P, Vanhaesebrouck P, De Praeter C, Moens K, Leroy J. Vacuum extraction, bone injury and neonatal subgaleal bleeding. Eur J Pediatr. 1992;151:532–5.
Doumouchtsis SK, Arulkumaran S. Head trauma after instrumental births. Clin Perinatol. 2008;35:69–83. viii
Levin G, Mankuta D, Eventov-Friedman S, Ezra Y, Elchalal U, Yagel S, et al. Neonatal subgaleal hemorrhage unrelated to assisted vaginal delivery: clinical course and outcomes. Arch Gynecol Obstet. 2020;301:93–9.
Colditz MJ, Lai MM, Cartwright DW, Colditz PB. Subgaleal haemorrhage in the newborn: A call for early diagnosis and aggressive management. J Paediatr Child Health. 2015;51:140–6.
Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164:1452–3.
McQuivey RW. Vacuum-assisted delivery: a review. J Matern Fetal Neonatal Med. 2004;16:171–80.
Chang HY, Peng CC, Kao HA, Hsu CH, Hung HY, Chang JH. Neonatal subgaleal hemorrhage: clinical presentation, treatment, and predictors of poor prognosis. Pediatr Int. 2007;49:903–7.
Christensen TR, Bahr TM, Henry E, Ling CY, Hanton TH, Page JM, et al. Neonatal subgaleal hemorrhage: twenty years of trends in incidence, associations, and outcomes. J Perinatol. 2023;43:573–7.
El-Dib M, Parziale MP, Johnson L, Benson CB, Grant PE, Robinson J, et al. Encephalopathy in neonates with subgaleal hemorrhage is a key predictor of outcome. Pediatr Res. 2019;86:234–41.
Shah NA, Wusthoff CJ. Intracranial Hemorrhage in the Neonate. Neonatal Netw. 2016;35:67–71.
Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32:228–32.
Doumouchtsis SK, Arulkumaran S. Head injuries after instrumental vaginal deliveries. Curr Opin Obstet Gynecol. 2006;18:129–34.
Uchil D, Arulkumaran S. Neonatal subgaleal hemorrhage and its relationship to delivery by vacuum extraction. Obstet Gynecol Surv. 2003;58:687–93.
Adedoyin OT, Johnson AW, Mokuolu OA, Ajayi OA. Acute renal failure complicating neonatal sub-galeal hemorrhage. Pediatr Nephrol. 2003;18:848–9.
Coe K, Lail C. Peritoneal dialysis in the neonatal intensive care unit. Management of acute renal failure after a severe subgaleal hemorrhage. Adv Neonatal Care. 2007;7:179–86.
Swanson AE, Veldman A, Wallace EM, Malhotra A. Subgaleal hemorrhage: risk factors and outcomes. Acta Obstet Gynecol Scand. 2012;91:260–3.
Angelis D, Savani R, Chalak L. Nitric oxide and the brain. Part 1: Mechanisms of regulation, transport and effects on the developing brain. Pediatr Res. 2021;89:738–45.
Boo NY, Foong KW, Mahdy ZA, Yong SC, Jaafar R. Risk factors associated with subaponeurotic haemorrhage in full-term infants exposed to vacuum extraction. BJOG. 2005;112:1516–21.
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013;2013:CD003311.
Isweisi E, Moore CM, Hurley T, Sola-Visner M, McCallion N, Ainle FN, et al. Haematological issues in neonates with neonatal encephalopathy treated with hypothermia. Semin Fetal Neonatal Med. 2021;26:101270.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl J Med. 2005;353:1574–84.
Chang HY, Cheng KS, Liu YP, Hung HF, Fu HW. Neonatal infected subgaleal hematoma: an unusual complication of early-onset E. coli sepsis. Pediatr Neonatol. 2015;56:126–8.
Salloum S, Sit W, Walton MM, Kamian K. Infected subgaleal hematoma in a 4-month-old girl. Am J Emerg Med. 2021;39:250.e5–e6.
Pollack S, Kassis I, Soudack M, Sprecher H, Sujov P, Guilburd JN, et al. Infected subgaleal hematoma in a neonate. Pediatr Infect Dis J. 2007;26:757–9.
Brook I. Infected neonatal cephalohematomas caused by anaerobic bacteria. J Perinat Med. 2005;33:255–8.
Kilani RA, Wetmore J. Neonatal subgaleal hematoma: presentation and outcome-radiological findings and factors associated with mortality. Am J Perinatol. 2006;23:41–8.
Kong CW, To WWK. Precision of vacuum cup placement and its association with subgaleal hemorrhage and associated morbidity in term neonates. Arch Gynecol Obstet. 2024;309:1411–9.
Levin G, Mankuta D, Eventov-Friedman S, Ezra Y, Koren A, Yagel S, et al. Factors associated with the severity of neonatal subgaleal haemorrhage following vacuum assisted delivery. Eur J Obstet Gynecol Reprod Biol. 2020;245:205–9.
Schreiber H, Cohen G, Farladansky-Gershnabel S, Shechter Maor G, Sharon-Weiner M, Biron-Shental T. Adverse outcomes in vacuum-assisted delivery after detachment of non-metal cup: a retrospective cohort study. Arch Gynecol Obstet. 2022;305:359–64.
Levin G, Elchalal U, Yagel S, Eventov-Friedman S, Ezra Y, Sompolinsky Y, et al. Risk factors associated with subgaleal hemorrhage in neonates exposed to vacuum extraction. Acta Obstet Gynecol Scand. 2019;98:1464–72.
Vacca A. Vacuum-assisted delivery. Best Pr Res Clin Obstet Gynaecol. 2002;16:17–30.
Kabiri D, Lipschuetz M, Cohen SM, Yagel O, Levitt L, Herzberg S, et al. Vacuum extraction failure is associated with a large head circumference. J Matern Fetal Neonatal Med. 2019;32:3325–30.
Guedalia J, Lipschuetz M, Daoud-Sabag L, Cohen SM, NovoselskyPersky M, Yagel S, et al. Prediction of neonatal subgaleal hemorrhage using first stage of labor data: A machine-learning based model. J Gynecol Obstet Hum Reprod. 2022;51:102320.
Gilboa Y, Kivilevitch Z, Kedem A, Spira M, Borkowski T, Moran O, et al. Caput succedaneum thickness in prolonged second stage of labour: a clinical evaluation. Aust N. Z J Obstet Gynaecol. 2013;53:459–63.
Gerscovich EO, McGahan JP, Jain KA, Gillen MA. Caput succedaneum mimicking a cephalocele. J Clin Ultrasound. 2003;31:98–102.
Sultan AH, Kamm MA, Bartram CI, Hudson CN. Anal sphincter trauma during instrumental delivery. Int J Gynaecol Obstet. 1993;43:263–70.
Fitzpatrick M, Behan M, O’Connell PR, O’Herlihy C. Randomised clinical trial to assess anal sphincter function following forceps or vacuum assisted vaginal delivery. BJOG 2003;110:424–9.
Li C, Miao JK, Xu Y, Hua YY, Ma Q, Zhou LL, et al. Prenatal, perinatal and neonatal risk factors for perinatal arterial ischaemic stroke: a systematic review and meta-analysis. Eur J Neurol. 2017;24:1006–15.
Govaert P, Vanhaesebrouck P, de Praeter C. Traumatic neonatal intracranial bleeding and stroke. Arch Dis Child. 1992;67:840–5.
Verma GL, Spalding JJ, Wilkinson MD, Hofmeyr GJ, Vannevel V, O’Mahony F. Instruments for assisted vaginal birth. Cochrane Database Syst Rev. 2021;9:CD005455
Plauche WC. Fetal cranial injuries related to delivery with the Malmstrom vacuum extractor. Obstet Gynecol. 1979;53:750–7.
Williams MC, Knuppel RA, O’Brien WF, Weiss A, Spellacy WN, Pietrantoni M. Obstetric correlates of neonatal retinal hemorrhage. Obstet Gynecol. 1993;81:688–94.
Goordyal D, Anderson J, Alazmani A, Culmer P. An engineering perspective of vacuum assisted delivery devices in obstetrics: A review. Proc Inst Mech Eng H. 2021;235:3–16.
Chan C, Pazandak C, Angelis D. Implementation of morbidity and mortality conference in a community hospital NICU and narrative review. Front Pediatr. 2023;11:1321296.
Legge N, Guaran R. Critical bleeding protocol for infants used for a catastrophic subgaleal haemorrhage. J Paediatr Child Health. 2022;58:542–5.
Morgan KM, Yazer MH, Triulzi DJ, Strotmeyer S, Gaines BA, Leeper CM. Safety profile of low-titer group O whole blood in pediatric patients with massive hemorrhage. Transfusion. 2021;61(Suppl 1):S8–S14.
Carr NR, Hulse WL, Bahr TM, Davidson JM, Ilstrup SJ, Christensen RD. First report of transfusing low-titer cold-stored type O whole blood to an extremely-low-birth-weight neonate after acute blood loss. Transfusion. 2022;62:1923–6.
Dunbar NM, Yazer MH, Biomedical Excellence for Safer Transfusion C, the SSI. Safety of the use of group A plasma in trauma: the STAT study. Transfusion. 2017;57:1879–84.
Strauss T, Kenet G, Schushan-Eisen I, Mazkereth R, Kuint J. Rescue recombinant activated factor VII for neonatal subgaleal hemorrhage. Isr Med Assoc J. 2009;11:639–40.
Hedner U. Recombinant factor VIIa: its background, development and clinical use. Curr Opin Hematol. 2007;14:225–9.
Novomedlink. Serious arterial and venous thrombotic events following administration of NovoSeven® RT have been reported: Novo Nordisk; 2024. https://www.novomedlink.com/
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N. Engl J Med. 2005;352:777–85.
Shapiro AD. Recombinant factor VIIa in the treatment of bleeding in hemophilic children with inhibitors. Semin Thromb Hemost. 2000;26:413–9.
Arkin S, Cooper HA, Hutter JJ, Miller S, Schmidt ML, Seibel NL, et al. Activated recombinant human coagulation factor VII therapy for intracranial hemorrhage in patients with hemophilia A or B with inhibitors. Results of the novoseven emergency-use program. Haemostasis. 1998;28:93–8.
Hunseler C, Kribs A, Eifinger F, Roth B. Recombinant activated factor seven in acute life-threatening bleeding in neonates: report on three cases and review of literature. J Perinatol. 2006;26:706–13.
Hirasaki Y, Suematsu Y, Yasuda T, Tajima K. Thromboelastometry to guide recombinant activated factor VII therapy for postoperative refractory intracranial bleeding. Anesth Analg. 2010;110:261–2.
Tengborn L, Blomback M, Berntorp E. Tranexamic acid-an old drug still going strong and making a revival. Thromb Res. 2015;135:231–42.
Camarasa MA, Olle G, Serra-Prat M, Martin A, Sanchez M, Ricos P, et al. Efficacy of aminocaproic, tranexamic acids in the control of bleeding during total knee replacement: a randomized clinical trial. Br J Anaesth. 2006;96:576–82.
Boese CK, Centeno L, Walters RW. Blood conservation using Tranexamic acid is not superior to Epsilon-Aminocaproic acid after total knee arthroplasty. J Bone Jt Surg Am. 2017;99:1621–8.
Keijzer, Wilschut DE R, Houmes RJ, van de Ven KP, van den Hout L, Sluijter I, et al. Congenital diaphragmatic hernia: to repair on or off extracorporeal membrane oxygenation? J Pediatr Surg. 2012;47:631–6.
Hensey OJ, Morgan ME, Cooke RW. Tranexamic acid in the prevention of periventricular haemorrhage. Arch Dis Child. 1984;59:719–21.
Maeda T, Sasabuchi Y, Matsui H, Ohnishi Y, Miyata S, Yasunaga H. Safety of Tranexamic acid in pediatric cardiac surgery: a nationwide database study. J Cardiothorac Vasc Anesth. 2017;31:549–53.
Wesley MC, Pereira LM, Scharp LA, Emani SM, McGowan FX Jr, DiNardo JA. Pharmacokinetics of tranexamic acid in neonates, infants, and children undergoing cardiac surgery with cardiopulmonary bypass. Anesthesiology. 2015;122:746–58.
Yee BE, Wissler RN, Zanghi CN, Feng C, Eaton MP. The effective concentration of tranexamic acid for inhibition of fibrinolysis in neonatal plasma in vitro. Anesth Analg. 2013;117:767–72.
Gertler R, Gruber M, Grassin-Delyle S, Urien S, Martin K, Tassani-Prell P, et al. Pharmacokinetics of tranexamic acid in neonates and infants undergoing cardiac surgery. Br J Clin Pharm. 2017;83:1745–57.
Sillero Rde O. Massive subgaleal hematoma. J Trauma. 2008;65:963.
Stalder MW, Dorafshar AH, Redett RJ. Calcified subgaleal hematoma with secondary cranial deformity in a patient with Kasabach-Merritt phenomenon. J Craniofac Surg. 2011;22:208–11.
Amar AP, Aryan HE, Meltzer HS, Levy ML. Neonatal subgaleal hematoma causing brain compression: report of two cases and review of the literature. Neurosurgery. 2003;52:1470–4. discussion 4
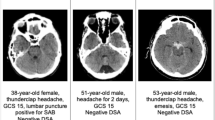
Tschauner S, Sorantin E. Imaging After Birth Trauma and in Suspected Non-accidental or Inflicted Injury. Springer, Cham; 2023.
Acuna J, Adhikari S. Point-of-care Ultrasound to distinguish subgaleal and Cephalohematoma: Case report. Clin Pr Cases Emerg Med. 2021;2:198–201.
Sorokan ST, Jefferies AL, Miller SP. Imaging the term neonatal brain. Paediatr Child Health. 2018;23:322–8.
Cory MJ, Durand P, Sillero R, Morin L, Savani R, Chalak L, et al. Vein of Galen aneurysmal malformation: rationalizing medical management of neonatal heart failure. Pediatr Res. 2023;93:39–48.
Kralik SF, Supakul N, Wu IC, Delso G, Radhakrishnan R, Ho CY, et al. Black bone MRI with 3D reconstruction for the detection of skull fractures in children with suspected abusive head trauma. Neuroradiology. 2019;61:81–7.
Acknowledgements
We would like to acknowledge the Crystal Charity Ball and the NeuroNICU program at the University of Texas Southwestern Medical Center for supporting this project. Figure 1 was created by Spyridoula Angeli, a high school student. For accuracy of anatomical structures, illustrations from Netter’s Atlas of Anatomy and Sobotta Human Atlas of Anatomy as well as various radiographic images were used.
Author information
Authors and Affiliations
Contributions
DA contributed to the concept of the paper, wrote the initial and revised drafts of this manuscript, and approved the final manuscript as submitted. KB critically reviewed the manuscript and approved it as submitted. GV, NB, SG, PV, RS, TS, KM, and RL contributed equally to the conceptualization of the paper, reviewed, and revised the manuscript, and approved the final manuscript as submitted. TS is a first-year neonatology fellow, while PV is a medical student at University of Texas, Southwestern Medical Center.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Babata, K., Vadlamudi, G., Bailey, N.A. et al. Subgaleal hemorrhage in neonates: a comprehensive review and summary recommendations. J Perinatol 45, 167–179 (2025). https://doi.org/10.1038/s41372-024-02116-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02116-w
This article is cited by
-
A collaborative “THRIVE Fetus to Five” neonatal brain program review
Pediatric Research (2026)
-
Risk factors for subgaleal hemorrhage and adverse early neonatal outcomes: a single-center cohort study with exclusive use of forceps
Journal of Perinatology (2025)