Abstract
The integration of BTK and BCL2 inhibitors into the treatment of patients with chronic lymphocytic leukemia (CLL) represents a paradigm shift and has led to significant improvements in clinical outcomes, including prolonged survival and enhanced quality of life. However, despite the efficacy of these agents, resistance to targeted therapy remains a major challenge, ultimately resulting in treatment failure and disease progression for a significant proportion of patients. Related to this, diagnostic testing for genetic variants associated with resistance, such as mutations in BTK, PLCG2 and BCL2, may become an increasingly common part of clinical routine practice. Addressing the need for placing the current knowledge in context, here we summarize the evidence from clinical studies and examine the underlying biology of both genetic and non-genetic resistance. Furthermore, we outline methodological approaches for the detection of gene alterations associated with targeted therapy resistance, discuss how to interpret these findings and highlight interpretation challenges. Finally, we offer insights into the clinical relevance of identifying genetic resistance to inform personalized treatment strategies and improve patient outcomes.
Similar content being viewed by others
Introduction
Targeted therapies using BTK inhibitors (BTKi) and/or BCL2 inhibitors (BCL2i) represent a paradigm shift in the management of patients with chronic lymphocytic leukemia (CLL) and have led to significant improvements in patient outcomes. Despite their efficacy, resistance to these targeted therapies may occur, resulting in treatment failure and disease progression for a significant proportion of patients. The specific resistance mechanisms observed and the timing of their onset show significant variation and are the result of an interplay of many factors including intrinsic disease characteristics, exposure to previous therapies and duration of exposure to the targeted agent (i.e. continuous versus time-limited therapy).
Understanding mechanisms of resistance to targeted agents may be highly informative for tailoring treatment both at the individual patient level as well as for clinical trials. Moreover, research into resistance mechanisms can impart crucial insights into disease and drug biology which may, in turn, inform the development of future therapeutic agents and approaches. In addition, diagnostic testing for genomic variants associated with resistance is becoming an increasingly common part of routine clinical practice. Herein, we summarize the landscape of resistance mechanisms observed during targeted treatment of CLL and their relevance for current clinical practice. We also provide a practical perspective on the approaches for the detection and interpretation of genomic alterations in the diagnostic laboratory that may help standardize practice in clinical trials and potentially in future clinical practice.
Btk-directed therapies
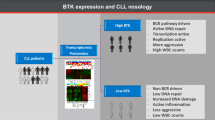
CLL cell survival is highly dependent on tonic signaling from the B cell receptor (BcR) which is transmitted through an intracellular signaling pathway with the tyrosine kinase BTK playing a critical role. As such, disrupting BTK function in CLL (which can be achieved through targeted inhibitor therapy or targeted degradation) has emerged as a highly effective therapeutic approach.
While most patients treated with BTK inhibitors (BTKis) will achieve at least a partial response (PR) [1,2,3,4], an initial worsening of lymphocytosis concurrent with shrinking of nodal disease, captured as PR with lymphocytosis (PR-L), is common with BTKi and due to redistribution of CLL cells from lymph nodes to the blood [5]. Importantly, initial progressive and persistent lymphocytosis in this context is not an indicator of resistance [6] and usually wanes after a few months of treatment. Primary resistance to BTKi treatment is very rare in frontline-treated patients and remains relatively uncommon even in heavily pretreated patients and should prompt a reevaluation of the diagnosis (i.e. presence of Richter transformation) [7,8,9,10].
Disease progression after an initial and prolonged response to BTK inhibition is the more typically observed clinical scenario. CLL progression can happen after discontinuing BTKi treatment (e.g. due to toxicity) or in the context of continuous BTKi treatment (i.e., secondary resistance) [11]. Relapses occurring after BTKi discontinuation do not necessarily indicate secondary resistance. In fact, patients with good response to BTKi therapy who then discontinue due to adverse events can enjoy prolonged stability without progression.
Mechanisms of resistance
BTK variants
One of the most common on-target resistance mechanisms to BTK directed therapies is the acquisition of genomic variants within the CLL cell which alter the amino acid sequence of the BTK protein and affect the binding/activity of various BTK directed therapies. The incidence of acquired BTK variants (which may be observed at a range of cancer cell fraction [CCF]) at progression on BTKi therapy varies between 10-80% depending on clinical context, mode of progression and the specific BTKi used (Table 1).
Acquired variants in BTK observed in the context of BTK-directed therapies can broadly be considered in three main groups (Fig. 1):
-
(i)
Variants that alter drug binding but have little to no effect on the kinase function of the BTK protein. This group includes BTK Cys481Ser, the first and most common BTK inhibitor resistance variant described, which converts the covalent interaction between ibrutinib (and indeed other covalent BTKis) and BTK to a reversible non-covalent interaction. This allows ATP to re-compete with covalent BTK inhibitors due to their short plasma half-life, which re-establishes enzyme activity and downstream signaling [12, 13].
-
(ii)
Variants that alter drug binding but also disrupt normal BTK kinase function. Examples of this group of variants (variably termed ‘kinase-impaired’ or ‘kinase-dead’) include BTK Leu528Trp, Cys481Arg and Val416Leu [14, 15]. Whilst the precise mechanism through which BTK signaling is preserved in the presence of these kinase-impaired BTK variants is still being elucidated, experimental data to date strongly support that these variants induce a scaffolding neofunction involving BTK that results in novel interactions with other intracellular signaling kinases (HCK and ILK) to re-establish downstream signaling [14, 16]. Importantly, the phenomenon of ‘kinase-impaired’ variants being associated with bypassing mechanisms involving alternative intracellular kinases has been observed in other contexts, most notably kinase-impaired BRAF variants [17].
-
(iii)
The final group of variants are those affecting the Thr474 codon (most commonly Thr474Ile). Thr474 functions as a gatekeeper residue controlling access to the catalytic domain and mutations at this position disrupt a hydrogen network between multiple amino acids resulting in decreased ability of covalent and non-covalent inhibitors to bind to BTK [18]. Indeed, the BTK Thr474Ile is paralogous to ABL1 Thr315Ile [19], the gatekeeper mutation conferring TKI resistance in CML. In addition, Thr474 mutations have been observed to increase BTK kinase activity in in vitro models [14, 20] however the precise biological and clinical implications of this increased kinase activity is unclear. Notably an increased intrinsic kinase activity is also observed with ABL1 Thr315Ile [21, 22]. Co-occurrence of Thr474Ile and Cys481 mutations have been observed in clinical cohorts, primarily thus far in patients treated with acalabrutinib [23].
Commonly observed acquired BTK variants are summarized in Table 2 and Fig. 2.
Figure 2a depicts variants observed in BTK, Fig. 2b in PLCG2, and Fig. 2c in BCL2. Variants are indicated by blue (missense) or gray (in-frame changes) lollipops positioned on a linear schematic of the protein sequence with domains annotated. Figure created by ProteinPaint (Zhou et al., Nat Genet 2016; PMID: 26711108).
Gain of function PLCG2 variants
Numerous missense variants have been observed in PLCG2 in the context of BTKi therapy including Arg665, Ser707, Leu845 and Met1141 codons (Table 2 and Fig. 2). PLCG2 is the direct downstream target of BTK and these variants result in hypermorphic PLCG2 function by both potentially constitutive activation as well as hyper-sensitivity to upstream signaling (Fig. 1) [24]. Indeed, many of the somatic PLCG2 variants observed in the context of BTKi therapy overlap with those occurring in autoimmune PLCG2-associated immune dysregulation (APLAID), an inherited syndrome caused by germline gain-of-function PLCG2 variants [25]. Notably, PLCG2 variants are rarely seen alone but rather more frequently observed in conjunction with BTK variants, commonly at very low CCF [12]. Whether and how often these variants occur in the same cell as BTK variants has yet to be definitively established.
Genomic and non-genomic alterations beyond the BcR pathway
A variable proportion of patients with secondary resistance to BTK directed therapies have no detectable BTK/PLCG2 resistance variants (Table 1). Multiple potential mechanisms have been proposed to be mediating resistance in the BTK/PLCG2 wildtype setting, including variants in EGR2 and NF-κB pathway genes along with deletions of chromosomes 2p and 8p [26,27,28]. Activated AKT together with deregulated PTEN and FOXO3a have been previously observed in ibrutinib-resistant CLL cells [29] as well as GAB1 upregulation leading to tonic AKT activity and increased homing capacity [30]. In addition, a “functional resistance” is thought to result from decreased dependence on proximal BcR signaling or its bypass through other pathways including the mitogen-activated protein kinase (MAPK) pathway [31] and the Toll-like receptor (TLR) pathways [31,32,33]. The precise frequency and contribution of these abnormalities to disease resistance and their specificity for BTK-directed therapies require further study.
Tumor microenvironment
Ibrutinib treatment has also been shown to have a negative impact on the anti-tumor properties of nurse-like cells (NLCs) in the tumor microenvironment (TME) which displayed reduced phagocytic ability, while expressing immunosuppressive cytokines, overall preventing ibrutinib-mediated primary CLL cell apoptosis [34, 35]. Furthermore, treatment of CLL cells with ibrutinib and venetoclax, after coculturing the tumor cells with TME agonists such as interleukin-10 (IL-10), CD40L, and CpG-ODNs (TLR-9 specific agonists), led to the activation of the NF-κB signaling pathway (especially alternative NF-κB). Subsequently, it induced the expression of the anti-apoptotic proteins MCL-1 and BCL-XL, promoting resistance to the combination therapy [36].
Covalent BTK inhibitors
The covalent BTKis (acalabrutinib, ibrutinib and zanubrutinib) share a similar mechanism of action in that they all bind irreversibly (covalently) to the Cys481 residue of BTK. Ibrutinib was the first agent in this class to enter clinical use which was followed by acalabrutinib and zanubrutinib with increasing kinome selectivity for BTK over other related kinases [37].
The pattern of BTK resistance variants observed differs significantly across the different covalent BTKis. BTK Cys481Ser is the dominant resistance variant observed in patients treated with ibrutinib, while kinase-impaired and Thr474 variants are more rarely observed [23]. In contrast, whilst Cys481Ser is the most frequently observed variant in patients with disease resistant to acalabrutinib, these patients also have a significantly higher incidence of Thr474 variants (typically observed in conjunction with a Cys481Ser variant) [23]. Finally, the BTK variant profile of zanubrutinib and tirabrutinib resistance differs again with Cys481Ser still being most common, but significantly higher rates of kinase-impaired BTK variants (commonly BTK Leu528Trp) than either ibrutinib or acalabrutinib [38, 39].
Non covalent BTK inhibitors
The non-covalent BTK inhibitors (ncBTKi) were designed to overcome the loss of covalent BTKi binding site that results from BTK Cys481 variants [40]. Pirtobrutinib is currently the most advanced ncBTKi clinically, having received accelerated approval from the FDA in December 2023 for patients with CLL after prior BTKi and venetoclax exposure. The BRUIN trial confirmed a high response rate (82%) in relapsed/refractory CLL including in those with Cys481Ser variants (comprising 38% of the cohort) [10]. Patients with disease progressing on pirtobrutinib in the BRUIN study showed a relatively high rate of acquired kinase-impaired BTK variants, particularly Thr474 and Leu528Trp [27/49 (55.5%) of tested cases with clinical progression] [41, 42]. Other ncBTKi have been studied clinically including vecabrutinib and nemtabrutinib, however, there have been no reports of BTK variants at clinical progression on these agents to date.
BTK “degrader” therapy
An emerging class of BTK-directed therapies are the proteolysis-targeting chimeras (PROTACs) which result in selective degradation of the BTK protein through complexing with E3 ligases [43]. In this way, these agents offer an attractive mechanism for overcoming various BTK resistance variants observed on cBTKi or ncBTKi therapies [14]. Several agents are under evaluation (NX-5948, NX-2127, BGB-16673) and have shown encouraging safety and efficacy in phase 1 trials among heavily pretreated patients with CLL after BTKi and BCL2i exposure [44, 45]. Interestingly, one patient treated with BGB-16673 developed a BTK Ala428Asp variant [46], however further data are required to understand the landscape of BTK variants occurring on these agents.
Resistance To Bcl2 Inhibitors
CLL cells show very high expression of the pro-survival molecule BCL2 and are critically reliant on this mechanism to avoid apoptotic cell death [47]. Small molecules that bind specifically to BCL2, relieving restraints on apoptosis in CLL cells, represent a major advancement in the treatment of CLL and have dramatically improved patient outcomes in the relapsed refractory [48, 49] and treatment naïve settings [50]. The most commonly used agent in this class is venetoclax and whilst newer agents are currently being clinically evaluated (including sonrotoclax [51] and lisaftoclax [52]), to date the majority of our understanding of BCL2i resistance comes from patients treated with venetoclax.
Similar to BTKi, true primary resistance to venetoclax-containing regimens is very rare in the first line setting and is even rarer in relapsed/refractory disease, and should raise consideration of the potential for Richter transformation. Indeed, the great majority of patients achieve significant cytoreduction unless treatment is ceased early due to toxicity [48, 50, 53,54,55,56]. Only in early monotherapy trials for previously heavily treated patients has failure to achieve at least a partial response been seen in more than 10% of patients [48, 56, 57]. Consequently, secondary resistance is the predominant form of resistance observed clinically.
Studies on resistance mechanisms to venetoclax are primarily based on the analysis of samples from patients treated with continuous venetoclax [58,59,60]. Presently, very little is known about clonal evolution during time-limited venetoclax therapy which achieves deep and durable remissions. Limited data on the success of retreating with venetoclax after initial time-limited therapy would also suggest that relapsing disease is not a priori resistant to venetoclax.
Studies based on samples from patients progressing on continuous venetoclax therapy have demonstrated that emergent resistance to BCL2 inhibition can arise through distinct genetic and epigenetic changes [58, 61,62,63,64]. The recurring mechanisms observed commonly across patients are outlined below. Similar to the BTKi context, a recurrent finding is that clinical resistance to venetoclax within an individual patient is often multifactorial with different mechanisms operating in CLL subpopulations collected from the same patient [59, 60, 62, 65]. Indeed, single cell multi-omics studies indicate that within single cells often two mechanisms may occur concurrently [60].
Mechanisms of resistance
BCL2 variants
Similar to variants arising in BTK on BTKi therapy, variants in BCL2 that affect drug binding are the canonical direct resistance mechanism observed in patients with CLL treated with continuous venetoclax (Table 2 and Fig. 2). BCL2 variants that have been observed to emerge in patients with CLL progressing on venetoclax in several independent clinical cohorts include Gly101Val [61], Asp103Tyr/Glu [62, 66, 67] and Phe104Leu/Ile/Cys [68], with experimental evidence supporting decreased drug binding but retention of pro-survival function. Analysis of crystal structures of the Gly101Val variant suggests that these mediate decreased venetoclax-BCL2 binding through a knock-on effect of Val101 to a three-dimensionally adjacent residue, Glu152 [68]. Other variants with less experimental/functional supporting data, but nevertheless occurring relatively specifically in the context of relapsed CLL treated with venetoclax, are Asp103Val, Arg107_Arg110dup, Ala113Gly, Arg129His and Val156Asp [62, 69,70,71]. Multiple variants can occur simultaneously within the same CLL patient. Notably, many of these variants occur either in, or adjacent to, the P4 pocket (critical for mediating venetoclax binding and selectivity over other BCL2 family molecules) (Fig. 3), or the BH3 binding groove more generally and are predicted to impair venetoclax-BCL2 binding [68].
Altered expression of proteins involved in apoptosis
Outside of drug-binding BCL2 variants, other direct resistance mechanisms to BCL2 inhibitor therapy involve perturbations of other proteins in the intrinsic apoptotic pathway. The most commonly observed abnormalities are increased expression of the alternative pro-survival BCL2 family molecules, MCL1, BCL-xL and BCL2A1 [58, 60, 61]. Higher expression of these proteins may occur by copy-number gain/amplification e.g. MCL1 [58, 60, 72] but most have epigenetic origins [60]. Recent work has also uncovered further complexity of cooperating genetic lesions in the apoptosis pathway, including loss of function PMAIP1 (NOXA) variants and loss-of-function BAX variants [60, 65, 69].
TP53 dysregulation
Loss or reduction in p53 function through TP53 aberrations (i.e. del(17p) and/or TP53 mutation) are associated with shorter duration of response with all CIT regimens and also with targeted therapies including venetoclax monotherapy [48, 73] and venetoclax-containing combination regimens. [50, 74, 75]. Intact p53 function is not required for achievement of complete remission [48, 56] and, indeed, complete remission rates are similar between TP53-wildtype and TP53-aberrant CLL [48, 75, 76]. However, aberrant p53 function in CLL is associated with inferior prognosis compared to intact p53 with venetoclax containing regimens [50, 74]. While venetoclax acts downstream of p53 in apoptosis initiation, when the mitochondrial permeabilization triggered by BH3 mimetics is sub-lethal, mitochondrial DNA release induces p53 activation, which in turn can generate a second wave of apoptotic stimulus through induction of PUMA and NOXA, which maximizes cell killing [77]. Although p53 function does not influence the susceptibility of mitochondria to apoptosis, absence of p53 function does reduce maximal BAX/BAK activation [78]. Consequently, in the absence of p53 function, there is a higher chance of escape, especially when venetoclax concentrations are submaximal [78]. Although follow-up is shorter, it appears that the time-limited combination of venetoclax and BTK inhibition, with or without an anti-CD20 does not obviate the long-term negative prognostic impact of TP53 aberrations in patients with treatment-I CLL [79].
BAX clonal hematopoiesis
The CLL compartment in patients treated with BCL2i adapts through the acquisition of BCL2 variants and alternative pro-survival molecule expression as described above. However, it has been recently observed that patients treated with BCL2i therapy may have adaptive clonal hematopoiesis outside the primary tumor compartment [80]. Hypothesized to be the result of the selective pressure of BCL2i therapy throughout the hematopoietic compartment, this is primarily manifest as loss of function BAX variants which may be detected in remission in patients with CLL on BCL2i with single-cell sequencing showing presence within the myeloid and NK-cell compartments [81]. Moreover, a recent analysis of patients randomized between venetoclax-obinutuzumab and chlorambucil-obinutuzumab in the CLL14 trial has shown a significant enrichment of BAX clonal hematopoiesis in the venetoclax containing arm [82]. Interestingly, BAX variants have also recently been recognized as a rare driver in age-related clonal hematopoiesis [83]. Whilst the potential clinical significance of BAX-mutated clonal hematopoiesis is unknown currently, it is an important phenomenon to be aware of given it may be detected during genomic testing of patients with CLL.
Diagnostic considerations for the investigation of resistance mutations in patients treated with targeted therapy
A summary of recommendations and considerations in a clinical setting, including clinical trials and observational studies is shown in Table 3.
Methodological approaches
Multiple types of genomic alterations (sequence variants, copy-number variants (CNVs) and structural variants) may be associated with targeted therapy resistance. That said, the most frequent tested abnormalities are single nucleotide variants (SNVs) and small insertions/deletions (indels) in BTK, PLCG2 and BCL2. Given the large number of potential nucleotide changes and often low variant allele frequency (VAF) that may give rise to relevant resistance variants in these genes, next-generation sequencing (NGS) has rapidly become the most commonly used methodology for detecting these alterations.
Targeted NGS gene panels employed by diagnostic laboratories in hematological malignancy typically have sequencing depths that permit reliable detection of variants down to approximately 1–5% VAF. Allele specific methodologies (e.g. droplet digital PCR) are potentially useful for single and high-sensitivity variant detection (potentially <0.1% VAF detection limit). However, given their absolute specificity for a single mutation they cannot be relied upon as an approach for screening patients for all potential resistance variants.
In addition, given the frequent presence of multiple resistance variants spanning increasing parts of relevant genes, NGS targeting of the whole coding region (including splice sites) is the most clinically relevant approach currently. However, if panel size is a limiting factor then BTK exons 14, 15 and 16 (NM_000061); PLCG2 exons 19, 20, 24 and 30 (NM_002661) and BCL2 exon 2 (NM_000633) will cover the majority of variants described to date. It should be noted that BCL2 exon 2 has a high GC content and may pose challenges with primer design and suboptimal coverage in amplicon-based panels but tends to be less of an issue using capture-based panels.
NGS testing for variants in BTK, PLCG2 and BCL2 is ideally performed after target enrichment and usually as part of a broader panel of genes assessed. There are numerous enrichment technologies that may be used, including two-primer amplicon, single primer extension/amplicon and hybridization-based approaches. These enrichment strategies are frequently combined with unique molecular indexing and duplex identification to improve sensitivity and specificity.
Ultimately any of these technical approaches may be used, however the laboratory performing the assay should have a robust understanding of the analytical performance of their assay including, but not limited to, sensitivity, specificity, reproducibility, linearity and coefficient of variation.
Sample considerations
When assessing for resistance variants, the most appropriate sample to test depends on both the clinical context and pattern of disease involvement. In the non-transformed setting, the most commonly tested sample is DNA extracted from mononuclear cells from peripheral blood (PB) or bone marrow (BM) aspirate due to ease of availability. DNA extracted from lymph node biopsy (either fresh or formalin-fixed, paraffin-embedded) may be used in the context of an SLL phenotype when there is no involvement of the PB or BM, or where there is discordant behavior of a specific anatomical site warranting directed evaluation.
It should be noted that in one series approximately half of patients with concurrent sampling of PB and lymph node showed differences in clonal composition between the two compartments [84]. A case report and preliminary data in a larger cohort support the possibility of similar separation of clonal evolutions between compartments in patients treated with BTKi [85]. In the same vein, BTK and/or PLCG2 mutations are more often identified in patients with disease progressing with prominent leukemic disease than in patients progressing primarily with nodal disease [86].
Whilst there is no absolute threshold of disease burden that is required to perform testing, the ability to detect low-frequent variants will be compromised at lower disease burden within the sample tested. As an example, if the disease burden in the sample is 20% and the molecular method has an intrinsic sensitivity of 2% VAF, then variants will only be detected when they involve greater than 10-20% of the clonal compartment (depending on zygosity). Enrichment of tumor cells with either CD19+ selection or negative depletion (e.g. MACS) may be of value, and is recommended for samples with low tumor burden if detection of subclonal variants is deemed of clinical relevance for the patient. In the context of possible transformed disease, the molecular profile of the transformed compartment may be significantly different from the untransformed CLL compartment and therefore samples containing transformed disease should be tested if deemed clinically relevant.
Finally, cell-free DNA (cfDNA) extracted from patient plasma can be used as a source for testing [87, 88]. However, the current understanding of the clinical relevance of findings from this compartment is limited. In addition, the quantity of circulating tumor DNA that can be routinely extracted from plasma in patients with CLL is low and therefore lower input/more sensitive methodologies may be required to detect variants. Whilst it is theoretically possible, there is no current evidence that the spectrum of resistance variants present in cfDNA differs significantly from an appropriate sample of the tumor compartment.
Reporting of variants
For accurate clinical reporting of laboratory test results, it is crucial to provide essential details about the sample type and the methods used for DNA extraction, target amplification and sequencing. Specifically, when reporting results from NGS-based tests, comprehensive information on the sequencing technology should be included. This should specify the type of targeted NGS applied (amplicon-based or capture-based), gene/exon coverage, the sequencing instrument used, and the laboratories validated limit of detection (LOD).
Each variant detected during diagnostic workup should be described at both the gene and protein levels adhering to HGVS nomenclature. Variant allele frequency (VAF) should be reported for assays that have been validated to report quantitative measurements. The observed VAF of any given variant(s) should be interpreted in the context of the CCF of the sample. This can be estimated by multiplying the observed VAF of an individual variant (or sum of VAFs in the case of multiple variants) by two for BCL2, PLCG2 and BTK (for females) and dividing by the observed quantity of disease present in the sample (typically most accurately quantitated by flow cytometry). This correction will give an approximation of the resistant proportion of the disease compartment that is accounted for by these variants. As mentioned, a range of clonality may be observed for variants in BTK/PLCG2/BCL2 with some patients having very low levels of identifiable resistance variants, whereas others having an almost complete clonal dominance by one particular variant. These scenarios potentially have different implications for therapeutic decision making.
After assessment using population databases (e.g. gnomAD v4) to determine germline versus somatic origin of the variant (in the context of tumor-only sequencing), each detected variant should be curated taking into account the precise molecular and predicted protein consequence (including assessment for splicing effect). Relevant literature for each variant detected should include previous peer-reviewed descriptions of emergence in the context of targeted therapy; evidence from clinical studies reporting the particular variant; the specific agent to which it is proposed as a resistance variant; and evidence from germline literature where appropriate (e.g. BTK loss of function variants or PLCG2 gain of function variants). Generally, the evidence for a variant being a predictive biomarker of targeted therapy resistance should derive from randomized control trials to assess a clinical endpoint in patients with and without the variant biomarker. While this type of evidence may exist for more non-specific markers of therapy resistance (e.g. variants in TP53 for patients treated with chemoimmunotherapy), it does not generally exist for specific on-target resistance variants arising during targeted therapy (e.g. BTK, PLCG2 and BCL2). This should be acknowledged if diagnostic laboratories are using variant curation frameworks such as the Standards and Guidelines for the Interpretation and Reporting of Sequence Variants in Cancer from the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists [89].
Clinical Implications of on-target resistance mutations
Clinical utility of resistance variant detection in current clinical practice
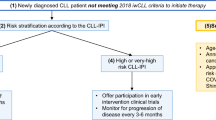
How to use resistance variant testing in current clinical practice remains incompletely defined and international guidelines on this topic are currently lacking. Despite this, in a rapidly changing therapeutic landscape, with new agents emerging within classes as well as entirely new classes entering the clinic, there is likely to be a need for rapid uptake and integration of new data obtained in clinical trials as well as in real-world settings.
Primary resistance to cBTKi and BCL2 inhibitors is extremely rare clinically and resistance variants in BTK and BCL2 have not been observed in CLL specimens prior to the relevant drug exposure [90]. Therefore, there is minimal value testing for BTK/PLCG2/BCL2 variants prior to commencement of therapy. Testing performed at time of suspected or confirmed clinical progression on or after targeted therapy is more commonly performed and the results of these tests can help interpret and confirm other clinicopathological observations. That notwithstanding, therapy providing ongoing clinical benefit should not be ceased if the patient has not had definitive clinical progression, since some patients may continue to derive benefit for prolonged periods after the first detection of a resistance variant [91]. However, the detection of such variants is predictive of a higher rate of subsequent disease progression and close monitoring is appropriate. The recognition of such variants can provide a window of opportunity to plan and prepare for the next line of therapy or consider available clinical trials.
An emerging area of clinical concern is potential cross resistance between cBTKi and ncBTKi. Both acalabrutinib and zanubrutinib have a significant incidence of resistance variants (Thr474Ile and Leu528Trp respectively) that have been identified as resistance variants also to pirtobrutinib. The presence of a high CCF cross-resistant BTK variant (particularly Thr474Ile or Leu528Trp) after cBTK therapy should prompt consideration of alternative therapies to pirtobrutinib, noting that venetoclax is active in this context [54, 92]. Going forward it will be important to determine how distinct mutations associated with progression on cBTKi impact outcomes of re-targeting BTK with either ncBTKis or BTK degraders.
The efficacy of re-treatment after time-limited venetoclax (in the front line or relapsed/refractory setting) is an area of active study. Whilst the incidence of BCL2 resistance variants is likely lower in the time-limited context [70], the presence of a high CCF/VAF BCL2 resistance variant could potentially be integrated into decision making regarding whether to pursue re-treatment or an alternative available therapy. Appropriately designed studies will be required to definitively provide answers to these questions; however, these data are unlikely to be imminently available for integration into care of patients in the clinic today.
The detection of variants with very low VAF/CCF in patients with clinical progression indicates that other resistance mechanisms may also be in play. The clinical significance of these variants, especially when considering re-treatment with the same drug class or cross-resistance between cBTKi and ncBTKi, is currently unknown.
Maximizing understanding of resistance from clinical studies
Identification of resistance mechanisms should be an important component of clinical trials of targeted therapies. In that regard, the comprehensive collection of clinical and laboratory characteristics within clinical trials provides an ideal setting to identify markers associated with the development of resistance and to differentiate between distinct resistance mechanisms. Ultimately, investigating resistance mechanisms in interventional clinical trials and real-world studies requires the systematic collection of appropriate samples with the following considerations:
-
Timepoints – samples should be collected (i) at baseline (before initiation of therapy) (ii) sequentially during the course of treatment and (iii) upon disease progression.
-
Sample type – DNA and RNA should be stored from peripheral blood (PB)/bone marrow aspirate (BM) at baseline and upon disease progression. Depending on resources, storing of DNA from timepoints throughout treatment should also be considered. As molecular MRD monitoring is increasingly incorporated in clinical trials, a practical approach may be to store an aliquot of DNA from each timepoint that MRD is measured. Whilst requiring significant resources to process and store, cryopreserved live tumor cells (stored as peripheral blood/bone marrow aspirate mononuclear cells) are highly valuable to functionally study resistance as well as single cell sequencing. Whilst DNA/RNA/cells form a core sample set, consideration of other sample types may also be relevant such as ctDNA (which may be stored as plasma) or nodal tissue.
-
Analysis type - The laboratory analyses should be preplanned but also allow for exploratory adjustment in the course of the studies, and need to be adapted to the specific treatment regimens (types of agents and combinations) and study designs (i.e. single vs. multi-arm, dose-finding vs. standard-setting). Both candidate as well as unbiased approaches to resistance mechanisms should be considered. The candidate approach (e.g. targeted BTK/PLCG2 sequencing) is useful to characterize known resistance mechanisms occurring at low level as these approaches typically allow for greater sensitivity. In contrast, unbiased approaches (e.g. whole genome transcriptome sequencing) are valuable for discovery of new resistance mechanisms.
Summary
Given the high effectiveness and rapid uptake of targeted therapies in CLL, it is important for clinicians to understand the meaning of targeted therapy resistance for their patients. The increasing complexity of this area also highlights the critical role of the diagnostic laboratory in the accurate description, variant curation and effective communication of genomic results issued in the clinical setting (including clinical trials to allow appropriate comparisons and reproducible conclusions). Finally, ongoing research and a deepening of our understanding of resistance mechanisms to targeted therapy gives invaluable insights into disease biology and informs critical elements of clinical trial design and therapeutic drug development.
References
Burger JA, Tedeschi A, Barr PM, Robak T, Owen C, Ghia P, et al. Ibrutinib as Initial Therapy for Patients with Chronic Lymphocytic Leukemia. N Engl J Med. 2015;373:2425–37.
Shanafelt TD, Wang XV, Kay NE, Hanson CA, O’Brien S, Barrientos J, et al. Ibrutinib-Rituximab or Chemoimmunotherapy for Chronic Lymphocytic Leukemia. N Engl J Med. 2019;381:432–43.
Sharman JP, Egyed M, Jurczak W, Skarbnik A, Pagel JM, Flinn IW, et al. Acalabrutinib with or without obinutuzumab versus chlorambucil and obinutuzmab for treatment-naive chronic lymphocytic leukaemia (ELEVATE TN): a randomised, controlled, phase 3 trial. Lancet. 2020;395:1278–91.
Tam CS, Brown JR, Kahl BS, Ghia P, Giannopoulos K, Jurczak W, et al. Zanubrutinib versus bendamustine and rituximab in untreated chronic lymphocytic leukaemia and small lymphocytic lymphoma (SEQUOIA): a randomised, controlled, phase 3 trial. Lancet Oncol. 2022;23:1031–43.
Herman SE, Niemann CU, Farooqui M, Jones J, Mustafa RZ, Lipsky A, et al. Ibrutinib-induced lymphocytosis in patients with chronic lymphocytic leukemia: correlative analyses from a phase II study. Leukemia. 2014;28:2188–96.
Woyach JA, Smucker K, Smith LL, Lozanski A, Zhong Y, Ruppert AS, et al. Prolonged lymphocytosis during ibrutinib therapy is associated with distinct molecular characteristics and does not indicate a suboptimal response to therapy. Blood. 2014;123:1810–7.
Brown JR, Eichhorst B, Hillmen P, Jurczak W, Kazmierczak M, Lamanna N, et al. Zanubrutinib or Ibrutinib in Relapsed or Refractory Chronic Lymphocytic Leukemia. N Engl J Med. 2023;388:319–32.
Byrd JC, Brown JR, O’Brien S, Barrientos JC, Kay NE, Reddy NM, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371:213–23.
Byrd JC, Hillmen P, Ghia P, Kater AP, Chanan-Khan A, Furman RR, et al. Acalabrutinib Versus Ibrutinib in Previously Treated Chronic Lymphocytic Leukemia: Results of the First Randomized Phase III Trial. J Clin Oncol. 2021;39:3441–52.
Mato AR, Woyach JA, Brown JR, Ghia P, Patel K, Eyre TA, et al. Pirtobrutinib after a Covalent BTK Inhibitor in Chronic Lymphocytic Leukemia. N Engl J Med. 2023;389:33–44.
Shanafelt TD, Wang XV, Hanson CA, Paietta EM, O’Brien S, Barrientos J, et al. Long-term outcomes for ibrutinib-rituximab and chemoimmunotherapy in CLL: updated results of the E1912 trial. Blood. 2022;140:112–20.
Woyach JA, Furman RR, Liu TM, Ozer HG, Zapatka M, Ruppert AS, et al. Resistance mechanisms for the Bruton’s tyrosine kinase inhibitor ibrutinib. N Engl J Med. 2014;370:2286–94.
Voice AT, Tresadern G, Twidale RM, van Vlijmen H, Mulholland AJ. Mechanism of covalent binding of ibrutinib to Bruton’s tyrosine kinase revealed by QM/MM calculations. Chem Sci. 2021;12:5511–6.
Montoya S, Bourcier J, Noviski M, Lu H, Thompson MC, Chirino A, et al. Kinase-impaired BTK mutations are susceptible to clinical-stage BTK and IKZF1/3 degrader NX-2127. Science. 2024;383:eadi5798.
Hamasy A, Wang Q, Blomberg KE, Mohammad DK, Yu L, Vihinen M, et al. Substitution scanning identifies a novel, catalytically active ibrutinib-resistant BTK cysteine 481 to threonine (C481T) variant. Leukemia. 2017;31:177–85.
Dhami K, Chakraborty A, Gururaja TL, Cheung LW, Sun C, DeAnda F, et al. Kinase-deficient BTK mutants confer ibrutinib resistance through activation of the kinase HCK. Sci Signal. 2022;15:eabg5216.
Heidorn SJ, Milagre C, Whittaker S, Nourry A, Niculescu-Duvas I, Dhomen N, et al. Kinase-dead BRAF and oncogenic RAS cooperate to drive tumor progression through CRAF. Cell. 2010;140:209–21.
Wang S, Mondal S, Zhao C, Berishaj M, Ghanakota P, Batlevi CL, et al. Noncovalent inhibitors reveal BTK gatekeeper and auto-inhibitory residues that control its transforming activity. JCI Insight. 2019;4:e127566.
Hantschel O, Rix U, Schmidt U, Burckstummer T, Kneidinger M, Schutze G, et al. The Btk tyrosine kinase is a major target of the Bcr-Abl inhibitor dasatinib. Proc Natl Acad Sci USA. 2007;104:13283–8.
Qiu S, Liu Y, Li Q. A mechanism for localized dynamics-driven activation in Bruton’s tyrosine kinase. R Soc Open Sci. 2021;8:210066.
Mian AA, Schull M, Zhao Z, Oancea C, Hundertmark A, Beissert T, et al. The gatekeeper mutation T315I confers resistance against small molecules by increasing or restoring the ABL-kinase activity accompanied by aberrant transphosphorylation of endogenous BCR, even in loss-of-function mutants of BCR/ABL. Leukemia. 2009;23:1614–21.
Yamamoto M, Kurosu T, Kakihana K, Mizuchi D, Miura O. The two major imatinib resistance mutations E255K and T315I enhance the activity of BCR/ABL fusion kinase. Biochem Biophys Res Commun. 2004;319:1272–5.
Woyach JA, Jones D, Jurczak W, Robak T, Illes A, Kater AP, et al. Mutational profile in previously treated patients with chronic lymphocytic leukemia progression on acalabrutinib or ibrutinib. Blood. 2024;144:1061–8.
Walliser C, Hermkes E, Schade A, Wiese S, Deinzer J, Zapatka M, et al. The Phospholipase Cgamma2 Mutants R665W and L845F Identified in Ibrutinib-resistant Chronic Lymphocytic Leukemia Patients Are Hypersensitive to the Rho GTPase Rac2 Protein. J Biol Chem. 2016;291:22136–48.
Baysac K, Sun G, Nakano H, Schmitz EG, Cruz AC, Fisher C, et al. PLCG2-associated immune dysregulation (PLAID) comprises broad and distinct clinical presentations related to functional classes of genetic variants. J Allergy Clin Immunol. 2024;153:230–42.
Bonfiglio S, Sutton LA, Ljungstrom V, Capasso A, Pandzic T, Westrom S, et al. BTK and PLCG2 remain unmutated in one-third of patients with CLL relapsing on ibrutinib. Blood Adv. 2023;7:2794–806.
Cosson A, Chapiro E, Bougacha N, Lambert J, Herbi L, Cung HA, et al. Gain in the short arm of chromosome 2 (2p+) induces gene overexpression and drug resistance in chronic lymphocytic leukemia: analysis of the central role of XPO1. Leukemia. 2017;31:1625–9.
Burger JA, Landau DA, Taylor-Weiner A, Bozic I, Zhang H, Sarosiek K, et al. Clonal evolution in patients with chronic lymphocytic leukaemia developing resistance to BTK inhibition. Nat Commun. 2016;7:11589.
Kapoor I, Li Y, Sharma A, Zhu H, Bodo J, Xu W, et al. Resistance to BTK inhibition by ibrutinib can be overcome by preventing FOXO3a nuclear export and PI3K/AKT activation in B-cell lymphoid malignancies. Cell Death Dis. 2019;10:924.
Seda V, Vojackova E, Ondrisova L, Kostalova L, Sharma S, Loja T, et al. FoxO1-GAB1 axis regulates homing capacity and tonic AKT activity in chronic lymphocytic leukemia. Blood. 2021;138:758–72.
Gounari M, Ntoufa S, Gerousi M, Vilia MG, Moysiadis T, Kotta K, et al. Dichotomous Toll-like receptor responses in chronic lymphocytic leukemia patients under ibrutinib treatment. Leukemia. 2019;33:1030–51.
Haselager MV, Kater AP, Eldering E. Proliferative signals in chronic lymphocytic leukemia; what are we missing?. Front Oncol. 2020;10:592205.
Fonte E, Apollonio B, Scarfo L, Ranghetti P, Fazi C, Ghia P, et al. In vitro sensitivity of CLL cells to fludarabine may be modulated by the stimulation of Toll-like receptors. Clin Cancer Res. 2013;19:367–79.
Boissard F, Fournie JJ, Quillet-Mary A, Ysebaert L, Poupot M. Nurse-like cells mediate ibrutinib resistance in chronic lymphocytic leukemia patients. Blood Cancer J. 2015;5:e355.
Fiorcari S, Maffei R, Audrito V, Martinelli S, Ten Hacken E, Zucchini P, et al. Ibrutinib modifies the function of monocyte/macrophage population in chronic lymphocytic leukemia. Oncotarget. 2016;7:65968–81.
Jayappa KD, Portell CA, Gordon VL, Capaldo BJ, Bekiranov S, Axelrod MJ, et al. Microenvironmental agonists generate de novo phenotypic resistance to combined ibrutinib plus venetoclax in CLL and MCL. Blood Adv. 2017;1:933–46.
Podoll T, Pearson PG, Kaptein A, Evarts J, de Bruin G, Emmelot-van Hoek M, et al. Identification and Characterization of ACP-5862, the major circulating active metabolite of acalabrutinib: both are potent and selective covalent bruton tyrosine kinase inhibitors. J Pharm Exp Ther. 2023;384:173–86.
Blombery P, Thompson ER, Lew TE, Tiong IS, Bennett R, Cheah CY, et al. Enrichment of BTK Leu528Trp mutations in patients with CLL on zanubrutinib: potential for pirtobrutinib cross-resistance. Blood Adv. 2022;6:5589–92.
Jackson RA, Britton RG, Jayne S, Lehmann S, Cowley CM, Trethewey CS, et al. BTK mutations in patients with chronic lymphocytic leukemia receiving tirabrutinib. Blood Adv. 2023;7:3378–81.
Jebaraj BMC, Muller A, Dheenadayalan RP, Endres S, Roessner PM, Seyfried F, et al. Evaluation of vecabrutinib as a model for noncovalent BTK/ITK inhibition for treatment of chronic lymphocytic leukemia. Blood. 2022;139:859–75.
Wang E, Mi X, Thompson MC, Montoya S, Notti RQ, Afaghani J, et al. Mechanisms of Resistance to Noncovalent Bruton’s Tyrosine Kinase Inhibitors. N Engl J Med. 2022;386:735–43.
Brown JR, Desikan SP, Nguyen B, Won H, Tantawy SI, McNeely S, et al. Genomic Evolution and Resistance during Pirtobrutinib Therapy in Covalent BTK-Inhibitor (cBTKi) Pre-Treated Chronic Lymphocytic Leukemia Patients: Updated Analysis from the BRUIN Study. Blood. 2023;142:326 -.
Casan JML, Seymour JF. Degraders upgraded: the rise of PROTACs in hematological malignancies. Blood. 2024;143:1218–30.
Searle E, Forconi F, Linton K, Danilov A, McKay P, Lewis D, et al. Initial Findings from a First-in-Human Phase 1a/b Trial of NX-5948, a Selective Bruton’s Tyrosine Kinase (BTK) Degrader, in Patients with Relapsed/Refractory B Cell Malignancies. Blood. 2023;142:4473.
Seymour JF, Cheah CY, Parrondo R, Thompson MC, Stevens DA, Lasica M, et al. First Results from a Phase 1, First-in-Human Study of the Bruton’s Tyrosine Kinase (BTK) Degrader Bgb-16673 in Patients (Pts) with Relapsed or Refractory (R/R) B-Cell Malignancies (BGB-16673-101). Blood. 2023;142:4401.
Wong RL, Choi MY, Wang HY, Kipps TJ. Mutation in Bruton Tyrosine Kinase (BTK) A428D confers resistance To BTK-degrader therapy in chronic lymphocytic leukemia. Leukemia. 2024;38:1818–21.
Del Gaizo Moore V, Brown JR, Certo M, Love TM, Novina CD, Letai A. Chronic lymphocytic leukemia requires BCL2 to sequester prodeath BIM, explaining sensitivity to BCL2 antagonist ABT-737. J Clin Invest. 2007;117:112–21.
Roberts AW, Davids MS, Pagel JM, Kahl BS, Puvvada SD, Gerecitano JF, et al. Targeting BCL2 with venetoclax in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374:311–22.
Seymour JF, Kipps TJ, Eichhorst B, Hillmen P, D’Rozario J, Assouline S, et al. Venetoclax-rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378:1107–20.
Fischer K, Al-Sawaf O, Bahlo J, Fink AM, Tandon M, Dixon M, et al. Venetoclax and obinutuzumab in patients with CLL and coexisting conditions. N Engl J Med. 2019;380:2225–36.
Guo Y, Xue H, Hu N, Liu Y, Sun H, Yu D, et al. Discovery of the Clinical Candidate Sonrotoclax (BGB-11417), a Highly Potent and Selective Inhibitor for Both WT and G101V Mutant Bcl-2. J Med Chem. 2024;67:7836–58.
Ailawadhi S, Chen Z, Huang B, Paulus A, Collins MC, Fu LT, et al. Novel BCL-2 Inhibitor lisaftoclax in relapsed or refractory chronic lymphocytic leukemia and other hematologic malignancies: first-in-human open-label trial. Clin Cancer Res. 2023;29:2385–93.
Jain N, Keating M, Thompson P, Ferrajoli A, Burger J, Borthakur G, et al. Ibrutinib and Venetoclax for First-Line Treatment of CLL. N Engl J Med. 2019;380:2095–103.
Jones JA, Mato AR, Wierda WG, Davids MS, Choi M, Cheson BD, et al. Venetoclax for chronic lymphocytic leukaemia progressing after ibrutinib: an interim analysis of a multicentre, open-label, phase 2 trial. Lancet Oncol. 2018;19:65–75.
Kater AP, Seymour JF, Hillmen P, Eichhorst B, Langerak AW, Owen C, et al. Fixed duration of venetoclax-rituximab in relapsed/refractory chronic lymphocytic leukemia eradicates minimal residual disease and prolongs survival: Post-Treatment Follow-Up of the MURANO Phase III Study. J Clin Oncol. 2019;37:269–77.
Stilgenbauer S, Eichhorst B, Schetelig J, Coutre S, Seymour JF, Munir T, et al. Venetoclax in relapsed or refractory chronic lymphocytic leukaemia with 17p deletion: a multicentre, open-label, phase 2 study. Lancet Oncol. 2016;17:768–78.
Kater AP, Arslan O, Demirkan F, Herishanu Y, Ferhanoglu B, Diaz MG, et al. Activity of venetoclax in patients with relapsed or refractory chronic lymphocytic leukaemia: analysis of the VENICE-1 multicentre, open-label, single-arm, phase 3b trial. Lancet Oncol. 2024;25:463–73.
Guieze R, Liu VM, Rosebrock D, Jourdain AA, Hernandez-Sanchez M, Martinez Zurita A, et al. Mitochondrial Reprogramming Underlies Resistance to BCL-2 Inhibition in Lymphoid Malignancies. Cancer Cell. 2019;36:369–84.e13.
Khalsa JK, Cha J, Utro F, Naeem A, Murali I, Kuang Y, et al. Genetic events associated with venetoclax resistance in CLL identified by whole-exome sequencing of patient samples. Blood. 2023;142:421–33.
Thijssen R, Tian L, Anderson MA, Flensburg C, Jarratt A, Garnham AL, et al. Single-cell multiomics reveal the scale of multilayered adaptations enabling CLL relapse during venetoclax therapy. Blood. 2022;140:2127–41.
Blombery P, Anderson MA, Gong JN, Thijssen R, Birkinshaw RW, Thompson ER, et al. Acquisition of the Recurrent Gly101Val Mutation in BCL2 Confers Resistance to Venetoclax in Patients with Progressive Chronic Lymphocytic Leukemia. Cancer Discov. 2019;9:342–53.
Blombery P, Thompson ER, Nguyen T, Birkinshaw RW, Gong JN, Chen X, et al. Multiple BCL2 mutations cooccurring with Gly101Val emerge in chronic lymphocytic leukemia progression on venetoclax. Blood. 2020;135:773–7.
Chong SJF, Zhu F, Dashevsky O, Mizuno R, Lai JX, Hackett L, et al. Hyperphosphorylation of BCL-2 family proteins underlies functional resistance to venetoclax in lymphoid malignancies. J Clin Invest. 2023;133:e170169.
Herling CD, Abedpour N, Weiss J, Schmitt A, Jachimowicz RD, Merkel O, et al. Clonal dynamics towards the development of venetoclax resistance in chronic lymphocytic leukemia. Nat Commun. 2018;9:727.
Thompson ER, Nguyen T, Kankanige Y, Markham JF, Anderson MA, Handunnetti SM, et al. Single-cell sequencing demonstrates complex resistance landscape in CLL and MCL treated with BTK and BCL2 inhibitors. Blood Adv. 2022;6:503–8.
Liu J, Li S, Wang Q, Feng Y, Xing H, Yang X, et al. Sonrotoclax overcomes BCL2 G101V mutation-induced venetoclax resistance in preclinical models of hematologic malignancy. Blood. 2024;143:1825–36.
Tausch E, Close W, Dolnik A, Bloehdorn J, Chyla B, Bullinger L, et al. Venetoclax resistance and acquired BCL2 mutations in chronic lymphocytic leukemia. Haematologica. 2019;104:e434–e7.
Birkinshaw RW, Gong JN, Luo CS, Lio D, White CA, Anderson MA, et al. Structures of BCL-2 in complex with venetoclax reveal the molecular basis of resistance mutations. Nat Commun. 2019;10:2385.
Popovic R, Dunbar F, Lu C, Robinson K, Quarless D, Warder SE, et al. Identification of recurrent genomic alterations in the apoptotic machinery in chronic lymphocytic leukemia patients treated with venetoclax monotherapy. Am J Hematol. 2022;97:E47–E51.
Kotmayer L, Laszlo T, Mikala G, Kiss R, Levay L, Hegyi LL, et al. Landscape of BCL2 Resistance mutations in a real-world cohort of patients with relapsed/refractory chronic lymphocytic leukemia treated with venetoclax. Int J Mol Sci. 2023;24:5802.
Lucas F, Larkin K, Gregory CT, Orwick S, Doong TJ, Lozanski A, et al. Novel BCL2 mutations in venetoclax-resistant, ibrutinib-resistant CLL patients with BTK/PLCG2 mutations. Blood. 2020;135:2192–5.
Thomalla D, Beckmann L, Grimm C, Oliverio M, Meder L, Herling CD, et al. Deregulation and epigenetic modification of BCL2-family genes cause resistance to venetoclax in hematologic malignancies. Blood. 2022;140:2113–26.
Roberts AW, Ma S, Kipps TJ, Coutre SE, Davids MS, Eichhorst B, et al. Efficacy of venetoclax in relapsed chronic lymphocytic leukemia is influenced by disease and response variables. Blood. 2019;134:111–22.
Kater AP, Wu JQ, Kipps T, Eichhorst B, Hillmen P, D’Rozario J, et al. Venetoclax Plus Rituximab in Relapsed Chronic Lymphocytic Leukemia: 4-Year Results and Evaluation of Impact of Genomic Complexity and Gene Mutations From the MURANO Phase III Study. J Clin Oncol. 2020;38:4042–54.
Tausch E, Schneider C, Robrecht S, Zhang C, Dolnik A, Bloehdorn J, et al. Prognostic and predictive impact of genetic markers in patients with CLL treated with obinutuzumab and venetoclax. Blood. 2020;135:2402–12.
Anderson MA, Deng J, Seymour JF, Tam C, Kim SY, Fein J, et al. The BCL2 selective inhibitor venetoclax induces rapid onset apoptosis of CLL cells in patients via a TP53-independent mechanism. Blood. 2016;127:3215–24.
Diepstraten ST, Yuan Y, La Marca JE, Young S, Chang C, Whelan L, et al. Putting the STING back into BH3-mimetic drugs for TP53-mutant blood cancers. Cancer Cell. 2024;42:850–68.e9.
Thijssen R, Diepstraten ST, Moujalled D, Chew E, Flensburg C, Shi MX, et al. Intact TP-53 function is essential for sustaining durable responses to BH3-mimetic drugs in leukemias. Blood. 2021;137:2721–35.
Allan JN, Flinn IW, Siddiqi T, Ghia P, Tam CS, Kipps TJ, et al. Outcomes in Patients with High-Risk Features after Fixed-Duration Ibrutinib plus Venetoclax: Phase II CAPTIVATE Study in First-Line Chronic Lymphocytic Leukemia. Clin Cancer Res. 2023;29:2593–601.
Blombery P, Lew TE, Dengler MA, Thompson ER, Lin VS, Chen X, et al. Clonal hematopoiesis, myeloid disorders and BAX-mutated myelopoiesis in patients receiving venetoclax for CLL. Blood. 2022;139:1198–207.
Tiong IS, Nguyen T, Teh C, Chua CC, Ftouni S, Lew TE, et al. BAX Mutated Clonal Hematopoiesis Arises Following Treatment with the BCL2 Inhibitor Class of Therapeutics across a Range of Hematological and Non-Hematological Neoplasms. Blood. 2023;142:2688.
Al-Sawaf O, Locher BN, Christen F, Robrecht S, Zhang C, Fink AM, et al. Clonal Hematopoiesis in Patients with Chronic Lymphocytic Leukemia Treated with Fixed-Duration Venetoclax-Obinutuzumab or Chlorambucil-Obinutuzumab: Insights from the Randomized CLL14 Trial. Blood. 2024;144:4613.
Bernstein N, Spencer Chapman M, Nyamondo K, Chen Z, Williams N, Mitchell E, et al. Analysis of somatic mutations in whole blood from 200,618 individuals identifies pervasive positive selection and novel drivers of clonal hematopoiesis. Nat Genet. 2024;56:1147–55.
Sun C, Chen YC, Martinez Zurita A, Baptista MJ, Pittaluga S, Liu D, et al. The immune microenvironment shapes transcriptional and genetic heterogeneity in chronic lymphocytic leukemia. Blood Adv. 2023;7:145–58.
Kiss R, Alpar D, Gango A, Nagy N, Eyupoglu E, Aczel D, et al. Spatial clonal evolution leading to ibrutinib resistance and disease progression in chronic lymphocytic leukemia. Haematologica. 2019;104:e38–e41.
Woyach JA, Ghia P, Byrd JC, Ahn IE, Moreno C, O’Brien SM, et al. B-cell receptor pathway mutations are infrequent in patients with chronic lymphocytic leukemia on continuous ibrutinib therapy. Clin Cancer Res. 2023;29:3065–73.
Yeh P, Hunter T, Sinha D, Ftouni S, Wallach E, Jiang D, et al. Circulating tumour DNA reflects treatment response and clonal evolution in chronic lymphocytic leukaemia. Nat Commun. 2017;8:14756.
Furstenau M, Weiss J, Giza A, Franzen F, Robrecht S, Fink AM, et al. Circulating Tumor DNA-Based MRD Assessment in Patients with CLL Treated with Obinutuzumab, Acalabrutinib, and Venetoclax. Clin Cancer Res. 2022;28:4203–11.
Li MM, Datto M, Duncavage EJ, Kulkarni S, Lindeman NI, Roy S, et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017;19:4–23.
Knisbacher BA, Lin Z, Hahn CK, Nadeu F, Duran-Ferrer M, Stevenson KE, et al. Molecular map of chronic lymphocytic leukemia and its impact on outcome. Nat Genet. 2022;54:1664–74.
Woyach JA, Ruppert AS, Guinn D, Lehman A, Blachly JS, Lozanski A, et al. BTK(C481S)-Mediated resistance to ibrutinib in chronic lymphocytic leukemia. J Clin Oncol. 2017;35:1437–43.
Lew TE, Bennett R, Lin VS, Whitechurch A, Handunnetti SM, Marlton P, et al. Venetoclax-rituximab is active in patients with BTKi-exposed CLL, but durable treatment-free remissions are uncommon. Blood Adv. 2024;8:1439–43.
Acknowledgements
The authors would like to gratefully acknowledge fundings sources including The Wilson Center for Blood Cancer Genomics (PB), the Snowdome Foundation (PB), RR: Supported by the Swedish Cancer Society (RR), the Swedish Research Council and Radiumhemmets Forskningsfonder (RR), Associazione Italiana per la Ricerca sul Cancro (AIRC) Foundation (GG) and the intramural research program of the NHLBI, NIH (AW), Leukemia & Lymphoma Society (JAW), Associazione Italiana per la Ricerca sul Cancro (AIRC) Foundation Milan (GL, PG).
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Consortia
Contributions
PB, TC, MG, RR, GG, SP, AWR, RWR, DR, LS, JFS, SS, AW, JAW, JRB, PG, and KS wrote the manuscript, critically evaluated the content, and approved the submitted version. PB, TC and KS edited the text. KS coordinated the manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
PB - Consultancy/advisory role and honoraria from AbbVie, Adaptive Biotechnologies, AstraZeneca and Roche Diagnostics; speakers bureau participation for AstraZeneca and Janssen. TC - Honoraria from AbbVie, AstraZeneca and BeiGene. GG - Advisory Boards/Speaker’s Bureau and honoraria from AbbVie, AstraZeneca, BeiGene, Hikma, Incyte, Johnson & Johnson, Lilly. LS - Honoraria from AbbVie, AstraZeneca, BeiGene, Johnson&Johnson, Lilly, Merck. SS - Advisory board/Research support/Travel support/Speaker fees from AbbVie, Amgen, AstraZeneca, BeiGene, BMS, Galapagos, Gilead, GSK, Hoffmann-La Roche, Janssen, Lilly, Novartis, Sunesis. AR - Inventor on a patent related to venetoclax; Employee of Walter and Eliza Hall Institute which received venetoclax-related milestone and royalty income, which is shared with employees; AbbVie, research funding for previous research; Janssen: research funding for research. RB - Employee of Walter and Eliza Hall Institute which received venetoclax-related milestone and royalty income, which is shared with employees. AW - Research support from Pharmacyclics LLC, an AbbVie Company, Acerta Pharma, a member of the AstraMI-Zeneca group, Merck, Nurix, Verastem and Genmab. RR - Honoraria from AbbVie, AstraZeneca, Illumina, Janssen, Lilly and Roche. JAW - Consultancy for AbbVie, AstraZeneca, Beigene, Genentech, J&J, Loxo/Lilly, Merck, and Newave. PG - Honoraria from AbbVie, AstraZeneca, BeiGene, BMS, Galapagos, Genmab, Johnson & Johnson, Lilly/LoxoOncology, MSD, Roche; research funding from AbbVie, AstraZeneca, BMS, Johnson & Johnson, Lilly/LoxoOncology, MSD. KS - Research support from AbbVie, AstraZeneca, Janssen, Novartis, Roche; honoraria from AbbVie, AstraZeneca, Bristol Myers Squibb, Lilly and Janssen.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Blombery, P., Chatzikonstantinou, T., Gerousi, M. et al. Resistance to targeted therapies in chronic lymphocytic leukemia: Current status and perspectives for clinical and diagnostic practice. Leukemia 39, 2049–2060 (2025). https://doi.org/10.1038/s41375-025-02662-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02662-y