Abstract
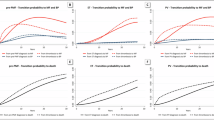
Thrombotic risk assessment is crucial in newly diagnosed essential thrombocythemia (ET) and polycythemia vera (PV) patients to guide cytoreductive therapy. We assessed whether thromboinflammation biomarkers would be good candidates to improve thrombosis risk stratification. We prospectively enrolled 394 newly diagnosed, cytoreductive therapy–naïve, ET and PV patients. We measured seven plasma biomarkers of neutrophil, monocyte, platelet, and endothelial activation, including NET markers, and evaluated their association with thrombosis risk scores at diagnosis. Multivariable analysis in the whole MPN cohort showed elevated calprotectin and tissue factor levels in high-risk versus low-risk patients using the conventional two-tiered score. This was also observed in ET patients only, but not in PV patients. Patients with a JAK2V617F allele burden >20% showed higher levels of three markers, including calprotectin, supporting its role in immunothrombosis. In PV patients, calprotectin correlated with the Venous Thrombosis Score (VETS), and five markers were elevated in those with prior venous thrombosis. Lastly, aspirin use was associated with lower H3Cit levels in patients with normal platelet counts, confirming its beneficial effect on NET formation. This is the largest study to date linking thromboinflammation markers to thrombotic risk in MPN patients and identifying potential biomarkers for future thrombosis risk scores.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
For original data, please contact chloe.james@inserm.fr.
References
Guy A, Poisson J, James C. Pathogenesis of cardiovascular events in BCR-ABL1-negative myeloproliferative neoplasms. Leukemia. 2021;35:935–55.
Stein BL, Martin K. From Budd-Chiari syndrome to acquired von Willebrand syndrome: thrombosis and bleeding complications in the myeloproliferative neoplasms. Hematology Am Soc Hematol Educ Program. 2019;2019:397–406.
Rungjirajittranon T, Owattanapanich W, Ungprasert P, Siritanaratkul N, Ruchutrakool T. A systematic review and meta-analysis of the prevalence of thrombosis and bleeding at diagnosis of Philadelphia-negative myeloproliferative neoplasms. BMC Cancer 2019;19:184.
Barbui T, Tefferi A, Vannucchi AM, Passamonti F, Silver RT, Hoffman R, et al. Philadelphia chromosome-negative classical myeloproliferative neoplasms: revised management recommendations from European LeukemiaNet. Leukemia. 2018;32:1057–69.
Barbui T, Finazzi G, Carobbio A, Thiele J, Passamonti F, Rumi E, et al. Development and validation of an International Prognostic Score of thrombosis in World Health Organization–essential thrombocythemia (IPSET-thrombosis). Blood. 2012;120:5128–33.
Barbui T, Vannucchi AM, Buxhofer-Ausch V, De Stefano V, Betti S, Rambaldi A, et al. Practice-relevant revision of IPSET-thrombosis based on 1019 patients with WHO-defined essential thrombocythemia. Blood Cancer J. 2015;5:e369.
Alvarez-Larrán A, Cuevas B, Velez P, Noya S, Caballero-Navarro G, Ferrer-Marín F, et al. Application of IPSET-thrombosis in 1366 patients prospectively followed from the Spanish registry of essential thrombocythemia. Hemasphere. 2023;7:e936.
Gu W, Zhang Y, Sun T, Ju M, Liu X, Xue F, et al. Prediction of thrombosis in polycythemia vera: Development and validation of a multiple factor-based prognostic score system. Res Pract Thrombosis Haemost. 2023;7:100132 mars.
Pasquer H, Daltro de Oliveira R, Vasseur L, Soret-Dulphy J, Maslah N, Zhao LP, et al. Distinct clinico-molecular arterial and venous thrombosis scores for myeloproliferative neoplasms risk stratification. Leukemia. 2024;38:326–39. févr.
Stark K, Massberg S. Interplay between inflammation and thrombosis in cardiovascular pathology. Nat Rev Cardiol. 2021;18:666–82. sept.
Guy A, Favre S, Labrouche-Colomer S, Deloison L, Gourdou-Latyszenok V, Renault MA, et al. High circulating levels of MPO-DNA are associated with thrombosis in patients with MPN. Leukemia. 2019;33:2544–8.
Guy A, Garcia G, Gourdou-Latyszenok V, Wolff-Trombini L, Josserand L, Kimmerlin Q, et al. Platelets and neutrophils cooperate to induce increased neutrophil extracellular trap formation in JAK2V617F myeloproliferative neoplasms. J Thrombosis Haemost. 2024;22:172–87.
Wolach O, Sellar RS, Martinod K, Cherpokova D, McConkey M, Chappell RJ, et al. Increased neutrophil extracellular trap formation promotes thrombosis in myeloproliferative neoplasms. Sci Transl Med [Internet]. 11 avr 2018 [cité 29 mars 2020];10. Disponible sur: https://stm.sciencemag.org/content/10/436/eaan8292.
Barbui T, De Stefano V, Alvarez-Larran A, Iurlo A, Masciulli A, Carobbio A, et al. Among classic myeloproliferative neoplasms, essential thrombocythemia is associated with the greatest risk of venous thromboembolism during COVID-19. Blood Cancer J. 2021;11:21.
Mauracher LM, Posch F, Martinod K, Grilz E, Däullary T, Hell L, et al. Citrullinated histone H3, a biomarker of neutrophil extracellular trap formation, predicts the risk of venous thromboembolism in cancer patients. J Thrombosis Haemost. 2018;16:508–18.
Benkhoff M, Alde K, Ehreiser V, Dahlmanns J, Metzen D, Haurand JM, et al. Thromboinflammation is associated with clinical outcome after ST-elevation myocardial infarction. Blood Adv. 2024;8:5581–9.
Veyrard P, Roblin X, Pansart C, Mao R, Nancey S, Killian M, et al. Serum calprotectin is useful to confirm inflammatory bowel disease activity but not to predict relapse. Clin Immunol Commun. 2022;2:33–8.
Colicchia M, Schrottmaier WC, Perrella G, Reyat JS, Begum J, Slater A, et al. S100A8/A9 drives the formation of procoagulant platelets through GPIbα. Blood. 2022;140:2626–43.
Silvin A, Chapuis N, Dunsmore G, Goubet AG, Dubuisson A, Derosa L, et al. Elevated calprotectin and abnormal myeloid cell subsets discriminate severe from mild COVID-19. Cell. 2020;182:1401–18.e18.
Zuo Y, Zuo M, Yalavarthi S, Gockman K, Madison JA, Shi H, et al. Neutrophil extracellular traps and thrombosis in COVID-19. J Thromb Thrombolysis. 2021;51:446–53.
Fuchs TA, Brill A, Duerschmied D, Schatzberg D, Monestier M, Myers DD, et al. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci. 2010;107:15880–5.
Barbui T, Barosi G, Birgegard G, Cervantes F, Finazzi G, Griesshammer M, et al. Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European LeukemiaNet. J Clin Oncol. 2011;29:761–70.
Thålin C, Daleskog M, Göransson SP, Schatzberg D, Lasselin J, Laska AC, et al. Validation of an enzyme-linked immunosorbent assay for the quantification of citrullinated histone H3 as a marker for neutrophil extracellular traps in human plasma. Immunol Res. 2017;65:706–12.
Thålin C, Aguilera K, Hall NW, Marunde MR, Burg JM, Rosell A, et al. Quantification of citrullinated histones: Development of an improved assay to reliably quantify nucleosomal H3Cit in human plasma. J Thrombosis Haemost. 2020;18:2732–43.
Jarlborg M, Courvoisier DS, Lamacchia C, Martinez Prat L, Mahler M, Bentow C, et al. Serum calprotectin: a promising biomarker in rheumatoid arthritis and axial spondyloarthritis. Arthritis Res Ther. 2020;22:105.
Hultcrantz M, Björkholm M, Dickman PW, Landgren O, Derolf ÅR, Kristinsson SY, et al. Risk for arterial and venous thrombosis in patients with myeloproliferative neoplasms: a population-based cohort study. Ann Intern Med. 2018;168:317.
for the Study Alliance Leukemia (SAL), Kaifie A, Kirschner M, Wolf D, Maintz C, Hänel M, et al. Bleeding, thrombosis, and anticoagulation in myeloproliferative neoplasms (MPN): analysis from the German SAL-MPN-registry. J Hematol Oncol. 2016;9:18.
Zhang Y, Zhou Y, Wang Y, Teng G, Li D, Wang Y, et al. Thrombosis among 1537 patients with JAK2-mutated myeloproliferative neoplasms: risk factors and development of a predictive model. Cancer Med. 2020;9:2096–105.
Nienhold R, Ashcroft P, Zmajkovic J, Rai S, Rao TN, Drexler B, et al. MPN patients with low mutant JAK2 allele burden show late expansion restricted to erythroid and megakaryocytic lineages. Blood. 2020;136:2591–5.
Rumi E, Pietra D, Ferretti V, Klampfl T, Harutyunyan AS, Milosevic JD, et al. JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood. 2014;123:1544–51.
Gerds AT, Mesa R, Burke JM, Grunwald MR, Stein BL, Squier P, et al. Association between elevated white blood cell counts and thrombotic events in polycythemia vera: analysis from REVEAL. Blood. 2024;143:1646–55.
Etulain J, Martinod K, Wong SL, Cifuni SM, Schattner M, Wagner DD. P-selectin promotes neutrophil extracellular trap formation in mice. Blood. 2015;126:242–6.
Clark SR, Ma AC, Tavener SA, McDonald B, Goodarzi Z, Kelly MM, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med. 2007;13:463–9.
Dyer MR, Chen Q, Haldeman S, Yazdani H, Hoffman R, Loughran P, et al. Deep vein thrombosis in mice is regulated by platelet HMGB1 through release of neutrophil-extracellular traps and DNA. Sci Rep. 2018;8:2068.
Rocca B, Tosetto A, Petrucci G, Rossi E, Betti S, Soldati D, et al. Long-term pharmacodynamic and clinical effects of twice- versus once-daily low-dose aspirin in essential thrombocythemia: the ARES trial. Am J Hematol. 2024;99:1462–74.
Perrier-Cornet A, Ianotto J-C, Mingant F, Perrot M, Lippert E, Galinat H. Decreased turnover aspirin resistance by bidaily aspirin intake and efficient cytoreduction in myeloproliferative neoplasms. Platelets. 2018;29:723–8.
Valdes V, Nardi MA, Elbaum L, Berger JS. Reproducibility over time and effect of low-dose aspirin on soluble P-selectin and soluble CD40 ligand. J Thromb Thrombolysis. 2015;40:83–7.
Ferroni P, Martini F, Riondino S, La Farina F, Magnapera A, Ciatti F, et al. Soluble P-selectin as a marker of in vivo platelet activation. Clin Chim Acta. 2009;399:88–91.
Pasquer H, Kiladjian JJ, Benajiba L. Current myeloproliferative neoplasm scoring systems for clinical practice. Blood. 2025;145:257–76.
Craver BM, Ramanathan G, Hoang S, Chang X, Mendez Luque LF, Brooks S, et al. N-acetylcysteine inhibits thrombosis in a murine model of myeloproliferative neoplasm. Blood Adv. 2020;4:312–21.
Marin Oyarzún CP, Carestia A, Lev PR, Glembotsky AC, Castro Ríos MA, Moiraghi B, et al. Neutrophil extracellular trap formation and circulating nucleosomes in patients with chronic myeloproliferative neoplasms. Sci Rep. 2016;6:38738.
Schmidt S, Daniliants D, Hiller E, Gunsilius E, Wolf D, Feistritzer C. Increased levels of NETosis in myeloproliferative neoplasms are not linked to thrombotic events. Blood Adv. 2021;5:3515–27.
Wang Y, Gao H, Kessinger CW, Schmaier A, Jaffer FA, Simon DI. Myeloid-related protein-14 regulates deep vein thrombosis. JCI Insight. 2017;2:e91356.
Marchetti M, Tartari CJ, Russo L, Panova-Noeva M, Leuzzi A, Rambaldi A, et al. Phospholipid-dependent procoagulant activity is highly expressed by circulating microparticles in patients with Essential Thrombocythemia. Am J Hematol. 2014;89:68–73.
Rayes J, Brill A. Hot under the clot: venous thrombogenesis is an inflammatory process. Blood. 2024;144:477–89.
Sacco M, Ranalli P, Lancellotti S, Petrucci G, Dragani A, Rocca B, et al. Increased von Willebrand factor levels in polycythemia vera and phenotypic differences with essential thrombocythemia. Res Pr Thromb Haemost. 2020;4:413–21.
De Grandis M, Cambot M, Wautier MP, Cassinat B, Chomienne C, Colin Y, et al. JAK2V617F activates Lu/BCAM-mediated red cell adhesion in polycythemia vera through an EpoR-independent Rap1/Akt pathway. Blood. 2013;121:658–65.
Poisson J, Tanguy M, Davy H, Camara F, Mdawar MBE, Kheloufi M, et al. Erythrocyte-derived microvesicles induce arterial spasms in JAK2V617F myeloproliferative neoplasm. J Clin Invest. 2020;130:2630–43.
Zhao B, Mei Y, Cao L, Zhang J, Sumagin R, Yang J, et al. Loss of pleckstrin-2 reverts lethality and vascular occlusions in JAK2V617F-positive myeloproliferative neoplasms [Internet]. American Society for Clinical Investigation; 2018 [cité 16 août 2020]. Disponible sur: https://www.jci.org/articles/view/94518/pdf.
Barbui T, Carobbio A, Finazzi G, Vannucchi AM, Barosi G, Antonioli E, et al. Inflammation and thrombosis in essential thrombocythemia and polycythemia vera: different role of C-reactive protein and pentraxin 3. Haematologica. 2011;96:315–8.
Liu W, Pircher J, Schuermans A, Ul Ain Q, Zhang Z, Honigberg MC, et al. Jak2 V617F clonal hematopoiesis promotes arterial thrombosis via platelet activation and cross talk. Blood. 2024;143:1539–50.
Falanga A, Marchetti M, Vignoli A, Balducci D, Russo L, Guerini V, et al. V617F JAK-2 mutation in patients with essential thrombocythemia: relation to platelet, granulocyte, and plasma hemostatic and inflammatory molecules. Exp Hematol. 2007;35:702–11.
Wang Y, Fang C, Gao H, Bilodeau ML, Zhang Z, Croce K, et al. Platelet-derived S100 family member myeloid-related protein-14 regulates thrombosis. J Clin Invest. 2014;124:2160–71.
Leimkühler NB, Gleitz HFE, Ronghui L, Snoeren IAM, Fuchs SNR, Nagai JS, et al. Heterogeneous bone-marrow stromal progenitors drive myelofibrosis via a druggable alarmin axis. Cell Stem Cell. 2021;28:637–52.e8.
Hogg N, Allen C, Edgeworth J. Monoclonal antibody 5.5 reacts with p8,14, a myeloid molecule associated with some vascular endothelium. Eur J Immunol. 1989;19:1053–61.
Pruenster M, Kurz ARM, Chung KJ, Cao-Ehlker X, Bieber S, Nussbaum CF, et al. Extracellular MRP8/14 is a regulator of β2 integrin-dependent neutrophil slow rolling and adhesion. Nat Commun. 2015;6:6915.
Zhong X, Xie F, Chen L, Liu Z, Wang Q. S100A8 and S100A9 promote endothelial cell activation through the RAGE‑mediated mammalian target of rapamycin complex 2 pathway. Mol Med Rep. 2020;22:5293–303.
Joshi A, Schmidt LE, Burnap SA, Lu R, Chan MV, Armstrong PC, et al. Neutrophil-derived protein S100A8/A9 alters the platelet proteome in acute myocardial infarction and is associated with changes in platelet reactivity. Arterioscler Thromb Vasc Biol. 2022;42:49–62.
Kovačić M, Mitrović-Ajtić O, Beleslin-Čokić B, Djikić D, Subotički T, Diklić M, et al. TLR4 and RAGE conversely mediate pro-inflammatory S100A8/9-mediated inhibition of proliferation-linked signaling in myeloproliferative neoplasms. Cell Oncol (Dordr). 2018;41:541–53.
Wang JC, Shi G, Chen C, Wong C, Gotlieb V, Joseph G, et al. TLR2 Derangements likely play a significant role in the inflammatory response and thrombosis in patients with Ph(−) classical myeloproliferative neoplasm. Mediators Inflamm. 2024;2024:1827127.
Baumeister J, Maié T, Chatain N, Gan L, Weinbergerova B, de Toledo MAS, et al. Early and late stage MPN patients show distinct gene expression profiles in CD34+ cells. Ann Hematol. 2021;100:2943–56.
Fiskus W, Masarova L, Mill CP, Birdwell C, Das K, Hou H, et al. Preclinical efficacy of tasquinimod-based combinations in advanced myeloproliferative neoplasms (MPN) in blastic phase. Blood Adv. 19 août 2025; bloodadvances.2025016898.
Samuelson BT, Vesely SK, Chai-Adisaksopha C, Scott BL, Crowther M, Garcia D. The impact of ruxolitinib on thrombosis in patients with polycythemia vera and myelofibrosis: a meta-analysis. Blood Coagul Fibrinolysis. 2016;27:648–52.
Masciulli A, Ferrari A, Carobbio A, Ghirardi A, Barbui T. Ruxolitinib for the prevention of thrombosis in polycythemia vera: a systematic review and meta-analysis. Blood Adv. 2020;4:380–6.
Acknowledgements
We thank the French group of MPN (France Intergroupe Syndrome Myéloproliferatifs, FIM) as the clinico-biological cohort FIMBANK team for the support in the conception and elaboration of the study, Fanny Robbesyn for the help in the coordination of the study, Valentin Landrieu for the help in calprotectin dosage realization, Audrey Bidet and the Center de Ressources Biologiques (CRB)- Cancer from Bordeaux hospital, all the CRBs involved in the preparation of samples.
Funding
This work was supported by grants from the association Force Hemato (“Appel à Projets Force Hemato”) and from the “Groupement Interrégional de Recherche Clinique et d’Innovation Sud-ouest Outre-Mer Hospitalier (GIRCI-SOHO)” (“Incitation à la recherche en cancérologie APIK 2018”). This work is a deliverable of the FIMBANK network, which was founded by the French ‘Institut National du Cancer’ (INCa BCB 2013 & 2020).
Author information
Authors and Affiliations
Consortia
Contributions
Contribution: CJ, AG and RT designed the study; MD, AC, RT, AG performed statistical analyses; GG, SLC, OM, MLB performed samples analysis; FB, J-C I, EL, LR, ST, BS, SG, GE, AP, A S-L, GD, CM, J-F V, LL, DR, MW, F-E N, FL, NC, LD, FG, J S-D, EC, FV, J-J K provided patients care and contributed to patients inclusion; LS, D L-P, VU coordinated data management of the FIMBANK biobank; AG and CJ wrote the manuscript; all authors provided data and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained from all study participants. The study was conducted in accordance with the principles of the Declaration of Helsinki. Approval was obtained from the Comité de Protection des Personnes (reference number: 19/060-3). All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guy, A., Mansier, O., Decilap, M. et al. Thromboinflammation is associated with high thrombotic risk in patients with newly diagnosed myeloproliferative neoplasms. Leukemia 40, 360–372 (2026). https://doi.org/10.1038/s41375-025-02836-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02836-8