Abstract
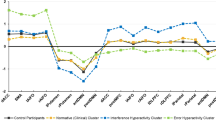
Improving diagnostic accuracy of obsessive-compulsive disorder (OCD) using models of brain imaging data is a key goal of the field, but this objective is challenging due to the limited size and phenotypic depth of clinical datasets. Leveraging the phenotypic diversity in large non-clinical datasets such as the UK Biobank (UKBB), offers a potential solution to this problem. Nevertheless, it remains unclear whether classification models trained on non-clinical populations will generalise to individuals with clinical OCD. This question is also relevant for the conceptualisation of OCD; specifically, whether the symptomology of OCD exists on a continuum from normal to pathological. Here, we examined a recently published “meta-matching” model trained on functional connectivity data from five large normative datasets (N = 45,507) to predict cognitive, health and demographic variables. Specifically, we tested whether this model could classify OCD status in three independent datasets (N = 345). We found that the model could identify out-of-sample OCD individuals. Notably, the most predictive functional connectivity features mapped onto known cortico-striatal abnormalities in OCD and correlated with genetic brain expression maps previously implicated in the disorder. Further, the meta-matching model relied upon estimates of cognitive functions, such as cognitive flexibility and inhibition, to successfully predict OCD. These findings suggest that variability in non-clinical brain and behavioural features can discriminate clinical OCD status. These results support a dimensional and transdiagnostic conceptualisation of the brain and behavioural basis of OCD, with implications for research approaches and treatment targets.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Code used to generate the results are available on GitHub (https://github.com/ljhearne/CBN_MetaMatch_public). The version of the meta-matching model used in the current work is available online (V2.0; https://github.com/ThomasYeoLab/Meta_matching_models). De-identified participant data for research purposes are available on request for data collected at the Brisbane [18] and Melbourne sites. De-identified participant data for research purposes are available on request for data collected at the Seoul site from the original authors [19].
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Arlingt VA. 2013. 2013.
Ahmari SE, Spellman T, Douglass NL, Kheirbek MA, Simpson HB, Deisseroth K, et al. Repeated cortico-striatal stimulation generates persistent OCD-like behavior. Science. 2013;340:1234–9.
Harrison BJ, Soriano-Mas C, Pujol J, Ortiz H, López-Solà M, Hernández-Ribas R, et al. Altered corticostriatal functional connectivity in obsessive-compulsive disorder. Arch Gen Psychiatry. 2009;66:1189–1200.
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: The orbitofronto-striatal model revisited. Neurosci Biobehav Rev. 2008;32:525–49.
Piantadosi SC, Chamberlain BL, Glausier JR, Lewis DA, Ahmari SE. Lower excitatory synaptic gene expression in orbitofrontal cortex and striatum in an initial study of subjects with obsessive compulsive disorder. Mol Psychiatry. 2021;26:986–98.
Shephard E, Stern ER, van den Heuvel OA, Costa DL, Batistuzzo MC, Godoy PB, et al. Toward a neurocircuit-based taxonomy to guide treatment of obsessive–compulsive disorder. Mol Psychiatry. 2021;26:4583–604.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive–compulsive disorder. Nat Rev Dis Primer. 2019;5:1–21.
Marek S, Tervo-Clemmens B, Calabro FJ, Montez DF, Kay BP, Hatoum AS, et al. Reproducible brain-wide association studies require thousands of individuals. Nature. 2022;603:654–60.
Poldrack RA, Huckins G, Varoquaux G Establishment of best practices for evidence for prediction: a review. JAMA Psychiatry. 2019. 27 November 2019. https://doi.org/10.1001/jamapsychiatry.2019.3671.
Chen P, An L, Wulan N, Zhang C, Zhang S, Ooi LQR, et al. Multilayer meta-matching: Translating phenotypic prediction models from multiple datasets to small data. Imaging Neurosci. 2024;2:1–22.
He T, An L, Chen P, Chen J, Feng J, Bzdok D, et al. Meta-matching as a simple framework to translate phenotypic predictive models from big to small data. Nat Neurosci. 2022;25:795–804.
Strom NI, Soda T, Mathews CA, Davis LK. A dimensional perspective on the genetics of obsessive-compulsive disorder. Transl Psychiatry. 2021;11:1–11.
Fullana MA, Vilagut G, Rojas-Farreras S, Mataix-Cols D, de Graaf R, Demyttenaere K, et al. Obsessive–compulsive symptom dimensions in the general population: Results from an epidemiological study in six European countries. J Affect Disord. 2010;124:291–9.
Robbins TW, Banca P, Belin D. From compulsivity to compulsion: the neural basis of compulsive disorders. Nat Rev Neurosci. 2024;25:313–33.
Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63.
Naze S, Hearne LJ, Roberts JA, Sanz-Leon P, Burgher B, Hall C, et al. Mechanisms of imbalanced frontostriatal functional connectivity in obsessive-compulsive disorder. Brain. 2023;146:1322–7.
Smit DJA, Cath D, Zilhão NR, Ip HF, Denys D, den Braber A, et al. Genetic meta-analysis of obsessive–compulsive disorder and self-report compulsive symptoms. Am J Med Genet B Neuropsychiatr Genet. 2020;183:208–16.
Cocchi L, Naze S, Robinson C, Webb L, Sonkusare S, Hearne LJ, et al. Effects of transcranial magnetic stimulation of the rostromedial prefrontal cortex in obsessive–compulsive disorder: a randomized clinical trial. Nat Ment Health. 2023;1:555–63.
Kim M, Kwak S, Yoon YB, Kwak YB, Kim T, Cho KIK, et al. Functional connectivity of the raphe nucleus as a predictor of the response to selective serotonin reuptake inhibitors in obsessive-compulsive disorder. Neuropsychopharmacology. 2019;44:2073–81.
Van Essen DC, Smith SM, Barch DM, Behrens TE, Yacoub E, Ugurbil K, et al. The WU-Minn human connectome project: an overview. Neuroimage. 2013;80:62–79.
Hearne LJ, Breakspear M, Harrison BJ, Hall CV, Savage HS, Robinson C, et al. Revisiting deficits in threat and safety appraisal in obsessive‐compulsive disorder. Hum Brain Mapp. 2023;44:6418–28.
Esteban O, Markiewicz CJ, Blair RW, Moodie CA, Isik AI, Erramuzpe A, et al. fMRIPrep: a robust preprocessing pipeline for functional MRI. Nat Methods. 2019;16:111–6.
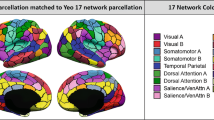
Schaefer A, Kong R, Gordon EM, Laumann TO, Zuo X-N, Holmes AJ, et al. Local-global parcellation of the human cerebral cortex from intrinsic functional connectivity MRI. Cereb Cortex N Y N 1991. 2018;28:3095–114.
Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–55.
Wang H-T, Meisler SL, Sharmarke H, Clarke N, Gensollen N, Markiewicz CJ, et al. Continuous evaluation of denoising strategies in resting-state fMRI connectivity using fMRIPrep and Nilearn. PLOS Comput Biol. 2024;20:e1011942.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLOS Med. 2015;12:e1001779.
Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, et al. The conception of the ABCD study: From substance use to a broad NIH collaboration. Dev Cogn Neurosci. 2018;32:4–7.
Alexander LM, Escalera J, Ai L, Andreotti C, Febre K, Mangone A, et al. An open resource for transdiagnostic research in pediatric mental health and learning disorders. Sci Data. 2017;4:170181.
Nooner KB, Colcombe S, Tobe R, Mennes M, Benedict M, Moreno A, et al. The NKI-rockland sample: a model for accelerating the pace of discovery science in psychiatry. Front Neurosci. 2012;6:152.
Holmes AJ, Hollinshead MO, O’Keefe TM, Petrov VI, Fariello GR, Wald LL, et al. Brain Genomics Superstruct Project initial data release with structural, functional, and behavioral measures. Sci Data. 2015;2:150031.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–34.
Davis KAS, Coleman JRI, Adams M, Allen N, Breen G, Cullen B, et al. Mental health in UK Biobank – development, implementation and results from an online questionnaire completed by 157 366 participants: a reanalysis. BJPsych Open. 2020;6:e18.
Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, et al. Scikit-learn: Machine learning in Python. J Mach Learn Res. 2011;12:2825–30.
Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics. 2007;8:118–27.
Pomponio R, Erus G, Habes M, Doshi J, Srinivasan D, Mamourian E, et al. Harmonization of large MRI datasets for the analysis of brain imaging patterns throughout the lifespan. NeuroImage. 2020;208:116450.
Ooi LQR, Chen J, Zhang S, Kong R, Tam A, Li J, et al. Comparison of individualized behavioral predictions across anatomical, diffusion and functional connectivity MRI. NeuroImage. 2022;263:119636.
Haufe S, Meinecke F, Görgen K, Dähne S, Haynes J-D, Blankertz B, et al. On the interpretation of weight vectors of linear models in multivariate neuroimaging. NeuroImage. 2014;87:96–110.
Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:1125–65.
Strom NI, Gerring ZF, Galimberti M, Yu D, Halvorsen MW, Abdellaoui A, et al. Genome-wide analyses identify 30 loci associated with obsessive–compulsive disorder. Nat Genet. 2025:1–13.
Hawrylycz MJ, Lein ES, Guillozet-Bongaarts AL, Shen EH, Ng L, Miller JA, et al. An anatomically comprehensive atlas of the adult human brain transcriptome. Nature. 2012;489:391–9.
Markello RD, Arnatkeviciute A, Poline J-B, Fulcher BD, Fornito A, Misic B. Standardizing workflows in imaging transcriptomics with the abagen toolbox. Elife. 2021;10:e72129.
Dear R, Wagstyl K, Seidlitz J, Markello RD, Arnatkevičiūtė A, Anderson KM, et al. Cortical gene expression architecture links healthy neurodevelopment to the imaging, transcriptomics and genetics of autism and schizophrenia. Nat Neurosci. 2024;27:1075–86.
Hawrylycz M, Miller JA, Menon V, Feng D, Dolbeare T, Guillozet-Bongaarts AL, et al. Canonical genetic signatures of the adult human brain. Nat Neurosci. 2015;18:1832–44.
Burt JB, Helmer M, Shinn M, Anticevic A, Murray JD. Generative modeling of brain maps with spatial autocorrelation. NeuroImage. 2020;220:117038.
Nadeau C, Bengio Y. Inference for the generalization error. Mach Learn. 2003;52:239–81.
Bouckaert RR, Frank E Evaluating the Replicability of Significance Tests for Comparing Learning Algorithms. In: Dai H, Srikant R, Zhang C, editors. Adv. Knowl. Discov. Data Min., Berlin, Heidelberg: Springer; 2004. p. 3–12.
Chyzhyk D, Varoquaux G, Milham M, Thirion B. How to remove or control confounds in predictive models, with applications to brain biomarkers. GigaScience. 2022;11:giac014.
Smith SM, Nichols TE. Statistical challenges in “Big Data” human neuroimaging. Neuron. 2018;97:263–8.
Spisak T. Statistical quantification of confounding bias in machine learning models. GigaScience. 2022;11:giac082.
Robbins TW, Vaghi MM, Banca P. Obsessive-compulsive disorder: puzzles and prospects. Neuron. 2019;102:27–47.
Glasser MF, Coalson TS, Robinson EC, Hacker CD, Harwell J, Yacoub E, et al. A multi-modal parcellation of human cerebral cortex. Nature. 2016;536:171–8.
Mahjani B, Bey K, Boberg J, Burton C. Genetics of obsessive-compulsive disorder. Psychol Med. 2021;51:2247–59.
Posthuma D. Revealing the complex genetic architecture of obsessive-compulsive disorder using meta-analysis. Mol Psychiatry. 2018;23:1181–8.
Mataix-Cols D, do Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. Am J Psychiatry. 2005;162:228–38.
Gillan CM, Fineberg NA, Robbins TW. A trans-diagnostic perspective on obsessive-compulsive disorder. Psychol Med. 2017;47:1528–48.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51.
Kebets V, Holmes AJ, Orban C, Tang S, Li J, Sun N, et al. Somatosensory-motor dysconnectivity spans multiple transdiagnostic dimensions of psychopathology. Biol Psychiatry. 2019;86:779–91.
Abramovitch A, Short T, Schweiger A. The C Factor: Cognitive dysfunction as a transdiagnostic dimension in psychopathology. Clin Psychol Rev. 2021;86:102007.
Wright L, Lipszyc J, Dupuis A, Thayapararajah SW, Schachar R. Response inhibition and psychopathology: A meta-analysis of go/no-go task performance. J Abnorm Psychol. 2014;123:429–39.
Gillan CM, Morein-Zamir S, Urcelay GP, Sule A, Voon V, Apergis-Schoute AM, et al. Enhanced avoidance habits in obsessive-compulsive disorder. Biol Psychiatry. 2014;75:631–8.
Rigoux L, Stephan KE, Petzschner FH. Beliefs, compulsive behavior and reduced confidence in control. PLOS Comput Biol. 2024;20:e1012207.
Chopra S, Dhamala E, Lawhead C, Ricard JA, Orchard ER, An L, et al. Generalizable and replicable brain-based predictions of cognitive functioning across common psychiatric illness. Sci Adv. 2024;10:eadn1862.
Abramovitch A, Abramowitz JS, Mittelman A. The neuropsychology of adult obsessive–compulsive disorder: a meta-analysis. Clin Psychol Rev. 2013;33:1163–71.
Banca P, Herrojo Ruiz M, Gonzalez-Zalba MF, Biria M, Marzuki AA, Piercy T, et al. Action sequence learning, habits, and automaticity in obsessive-compulsive disorder. eLife. 2024;12:RP87346.
Marzuki AA, Tomić I, Ip SHY, Gottwald J, Kanen JW, Kaser M, et al. Association of environmental uncertainty with altered decision-making and learning mechanisms in youths with obsessive-compulsive disorder. JAMA Netw Open. 2021;4:e2136195–e2136195.
Snyder HR, Kaiser RH, Warren SL, Heller W. Obsessive-compulsive disorder is associated with broad impairments in executive function: a meta-analysis. Clin Psychol Sci. 2015;3:301–30.
van den Heuvel OA, van Wingen G, Soriano-Mas C, Alonso P, Chamberlain SR, Nakamae T, et al. Brain circuitry of compulsivity. Eur Neuropsychopharmacol. 2016;26:810–27.
Figee M, Luigjes J, Smolders R, Valencia-Alfonso C-E, van Wingen G, de Kwaasteniet B, et al. Deep brain stimulation restores frontostriatal network activity in obsessive-compulsive disorder. Nat Neurosci. 2013;16:386–7.
Bruin WB, Abe Y, Alonso P, Anticevic A, Backhausen LL, Balachander S, et al. The functional connectome in obsessive-compulsive disorder: resting-state mega-analysis and machine learning classification for the ENIGMA-OCD consortium. Mol Psychiatry. 2023:1–13.
Bu X, Hu X, Zhang L, Li B, Zhou M, Lu L, et al. Investigating the predictive value of different resting-state functional MRI parameters in obsessive-compulsive disorder. Transl Psychiatry. 2019;9:17.
Buckner RL, Andrews-Hanna JR, Schacter DL. The Brain’s default network. Ann N Y Acad Sci. 2008;1124:1–38.
Coles ME, Heimberg RG, Frost RO, Steketee G. Not just right experiences and obsessive–compulsive features:: Experimental and self-monitoring perspectives. Behav Res Ther. 2005;43:153–67.
Ahmari SE, Risbrough VB, Geyer MA, Simpson HB. Impaired sensorimotor gating in unmedicated adults with obsessive–compulsive disorder. Neuropsychopharmacology. 2012;37:1216–23.
Kawabe H, Sakisaka T, Yasumi M, Shingai T, Izumi G, Nagano F, et al. A novel rabconnectin‐3‐binding protein that directly binds a GDP/GTP exchange protein for Rab3A small G protein implicated in Ca2+‐dependent exocytosis of neurotransmitter. Genes Cells. 2003;8:537–46.
Zhuo B, Zhu L, Yao C, Wang X, Li S, Wang R, et al. ADCK1 is a potential therapeutic target of osteosarcoma. Cell Death Dis. 2022;13:954.
Koppe G, Meyer-Lindenberg A, Durstewitz D. Deep learning for small and big data in psychiatry. Neuropsychopharmacology. 2021;46:176–90.
Weiss K, Khoshgoftaar TM, Wang D. A survey of transfer learning. J Big Data. 2016;3:1–40.
Acknowledgements
This work was supported by the Australian NHMRC (GN2001283 and GNT2027597, L.C). A.Z. and L.J.H were supported by research fellowships from the NHMRC (APP1118153, APP1194070, respectively). PBF is supported by a National Health and Medical Research Council of Australia Investigator grant (1193596). BTTY is supported by the NUS Yong Loo Lin School of Medicine (NUHSRO/2020/124/TMR/LOA), the Singapore National Medical Research Council (NMRC) LCG (OFLCG19May-0035), NMRC CTG-IIT (CTGIIT23jan-0001), NMRC OF-IRG (OFIRG24jan-0006; OFIRG24jul-0049), NMRC STaR (STaR20nov-0003), Singapore Ministry of Health (MOH) Centre Grant (CG21APR1009), the United States National Institutes of Health (R01MH133334 & 2R01MH120080) and the Singapore National Research Foundation (NRF) Investigatorship (NRFI10-2024-0014).
Author information
Authors and Affiliations
Contributions
LJH and LC conceptualised the research. LW, PBF, OWM, YET, MB, CVH, MK, JSK, & LC contributed to data collection and/or data curation. BTTY developed methodology used in the analysis. LJH performed the analysis and wrote the first draft. All authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
L.C., L.J.H, and A.Z. are involved in a clinical neuromodulation centre (Queensland Neurostimulation Centre [QNC] as trading for Australian Brain Foundation) that offers neuroimaging-guided neurotherapeutics. LJH, AZ, and LC are not paid by QNC. This centre had no role in this study. L.C. serves as a co-inventor on a patent application by the National University of Singapore that covers neuroimaging-based personalised TMS. LC, LJH, and AZ are also involved in the development of imaging-based personalized TMS for depression with ANT Neuro. The provisional patent and ANT Neuro products are not directly related to this work. In the last 3 years PBF has received equipment for research from Neurosoft and Nexstim. He has served on a scientific advisory board for Magstim and received speaker fees from Otsuka. He has also acted as a founder and board member for TMS Clinics Australia and Resonance Therapeutics. BTTY holds shares and is a co-founder of B1neuro. The content in this manuscript is unrelated to the activities of B1neuro.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hearne, L.J., Yeo, B.T.T., Webb, L. et al. Distinct cognitive and functional connectivity features from healthy cohorts can identify clinical obsessive-compulsive disorder. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-03416-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41380-025-03416-z