Abstract
Early life trauma (ELT) exposure and posttraumatic stress disorder (PTSD) both affect neural structure, which predicts a variety of mental health concerns throughout the lifespan and may present differently between adolescents and adults. However, few studies have identified the relationship between ELT, PTSD, development, and brain structure using cortical thickness (CT). CT may reveal previously obscured alterations that are potentially clinically relevant and, furthermore, could identify specific structural correlates distinct to ELT from PTSD. Two hundred and fifty-three female adolescent and adult survivors of interpersonal violence and non-trauma-exposed demographically matched controls underwent structural MRI at two different sites. Images were processed and CT was estimated using FreeSurfer. Vertex-wise linear model tests were conducted across the cortical surface to investigate whether PTSD and ELT exposure uniquely affect CT, controlling for scanner site. Planned follow-up tests included second-level analyses of clinical symptoms for CT clusters that were significantly related to PTSD or ELT. CT in the middle cingulate cortex was inversely related to ELT in both age groups, such that individuals with more ELT demonstrated less CT in this region. Additionally, CT was significantly greater in the bilateral intraparietal sulcus and left angular gyrus in both adolescents and adults with PTSD. Furthermore, CT in these clusters was also significantly related to clinical symptom severity in the adult PTSD group. This study provides evidence for distinct CT correlates of ELT and PTSD that are present across adolescents and adults, suggesting consistent markers related to ELT and PTSD on gray matter structure in trauma-exposed individuals.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Hart H, Rubia K. Neuroimaging of child abuse: a critical review. Front Hum Neurosci. 2012;6:52.
Lim L, Radua J, Rubia K. Gray matter abnormalities in childhood maltreatment: a voxel-wise meta-analysis. Am J Psychiatry. 2014;171:854–63.
Kühn S, Gallinat J. Gray matter correlates of posttraumatic stress disorder: a quantitative meta-analysis. Biol Psychiatry. 2013;73:70–74.
Butler O, Adolf J, Gleich T, Willmund G, Zimmermann P, Lindenberger U, et al. Military deployment correlates with smaller prefrontal gray matter volume and psychological symptoms in a subclinical population. Transl Psychiatry. 2017;7:e1031.
Fischl B, Dale AM. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci USA. 2000;97:11050–5.
Wierenga LM, Langen M, Oranje B, Durston S. Unique developmental trajectories of cortical thickness and surface area. Neuroimage 2014;87:120–6.
Tamnes CK, Østby Y, Walhovd KB, Westlye LT, Due-Tønnessen P, Fjell AM. Neuroanatomical correlates of executive functions in children and adolescents: a magnetic resonance imaging (MRI) study of cortical thickness. Neuropsychologia 2010;48:2496–508.
Abdallah CG, Sanacora G, Duman RS, Krystal JH. Ketamine and rapid-acting antidepressants: a window into a new neurobiology for mood disorder therapeutics. Annu Rev Med. 2015;66:509–23.
Averill LA, Purohit P, Averill CL, Boesl MA, Krystal JH, Abdallah CG. Glutamate dysregulation and glutamatergic therapeutics for PTSD: evidence from human studies. Neurosci Lett. 2017;649:147–55.
Cisler JM, Herringa RJ. Posttraumatic stress disorder and the developing adolescent brain. Biol Psychiatry. 2020. https://doi.org/10.1016/j.biopsych.2020.06.001.
Kelly PA, Viding E, Wallace GL, Schaer M, De Brito SA, Robustelli B, et al. Cortical thickness, surface area, and gyrification abnormalities in children exposed to maltreatment: neural markers of vulnerability? Biol Psychiatry. 2013;74:845–52.
Whittle S, Dennison M, Vijayakumar N, Simmons JG, Yücel M, Lubman DI, et al. Childhood maltreatment and psychopathology affect brain development during adolescence. J Am Acad Child Adolesc Psychiatry. 2013;52:940–52.e1.
Corbo V, Salat DH, Amick MM, Leritz EC, Milberg WP, McGlinchey RE. Reduced cortical thickness in veterans exposed to early life trauma. Psychiatry Res Neuroimaging. 2014;223:53–60.
Heim CM, Mayberg HS, Mletzko T, Nemeroff CB, Pruessner JC. Decreased cortical representation of genital somatosensory field after childhood sexual abuse. Am J Psychiatry. 2013;170:616–23.
Averill LA, Abdallah CG, Pietrzak RH, Averill CL, Southwick SM, Krystal JH, et al. Combat exposure severity is associated with reduced cortical thickness in combat veterans: a preliminary report. Chronic Stress. 2017. https://doi.org/10.1177/2470547017724714.
Wrocklage KM, Averill LA, Cobb Scott J, Averill CL, Schweinsburg B, Trejo M, et al. Cortical thickness reduction in combat exposed U.S. veterans with and without PTSD. Eur Neuropsychopharmacol. 2017;27:515–25.
Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61:4–12.
Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61:984.
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995;52:1048–60.
Breslau N, Davis GC, Andreski P, Peterson EL, Schultz LR. Sex differences in posttraumatic stress disorder. Arch Gen Psychiatry. 1997;54:1044–8.
Blanco C, Hoertel N, Wall MM, Franco S, Peyre H, Neria Y, et al. Toward understanding sex differences in the prevalence of posttraumatic stress disorder: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2018;79:0–0.
Busso DS, McLaughlin KA, Brueck S, Peverill M, Gold AL, Sheridan MA. Child abuse, neural structure, and adolescent psychopathology: a longitudinal study. J Am Acad Child Adolesc Psychiatry. 2017;56:321–28.e1.
Bing X, Ming-guo Q, Ye Z, Jing-na Z, Min L, Han C, et al. Alterations in the cortical thickness and the amplitude of low-frequency fluctuation in patients with post-traumatic stress disorder. Brain Res. 2013;1490:225–32.
Ross MC, Lenow JK, Kilts CD, Cisler JM. Altered neural encoding of prediction errors in assault-related posttraumatic stress disorder. J Psychiatr Res. 2018;103:83–90.
Sellnow K, Sartin-Tarm A, Ross MC, Weaver S, Cisler JM. Biotypes of functional brain engagement during emotion processing differentiate heterogeneity in internalizing symptoms and interpersonal violence histories among adolescent girls. J Psychiatr Res. 2020;121:197–206.
Cisler JM, Bush K, Scott Steele J, Lenow JK, Smitherman S, Kilts CD. Brain and behavioral evidence for altered social learning mechanisms among women with assault-related posttraumatic stress disorder. J Psychiatr Res. 2015;63:75–83.
Lenow J, Cisler J, Bush K. Altered trust learning mechanisms among female adolescent victims of interpersonal violence. J Interpers Violence. 2015. https://doi.org/10.1177/0886260515604411.
Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: data from a national sample. J Consult Clin Psychol. 2000;68:19–30.
Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J Clin Psychiatry. 2010;71:313–26.
Kaufman J, Birmhauer B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8.
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 2002.
Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Curr Psychiatry Rep. 2016;6:96–100.
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28:489–98.
Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL). Behav Res Ther. 1996;34:669–73.
Moshier SJ, Lee DJ, Bovin MJ, Gauthier G, Zax A, Rosen RC, et al. An empirical crosswalk for the PTSD checklist: translating DSM‐IV to DSM‐5 using a veteran sample. J Trauma Stress. 2019;32:799–805.
Bernstein DP, Fink L. Childhood trauma questionnaire: a retrospective self-report: manual. Harcourt Brace & Company; 1998.
Wardenaar KJ, van Veen T, Giltay EJ, de Beurs E, Penninx BWJH, Zitman FG. Development and validation of a 30-item short adaptation of the Mood and Anxiety Symptoms Questionnaire (MASQ). Psychiatry Res. 2010;179:101–6.
Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996.
Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991.
Watson D, Anna L, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–70.
Fischl B, Sereno MI, Tootell RBH, Dale AM. High-resolution intersubject averaging and a coordinate system for the cortical surface. Hum Brain Mapp. 1999;8:272–84.
Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res Int J. 1996;29:162–73.
Frøkjær JB, Bouwense SAW, Olesen SS, Lundager FH, Eskildsen SF, Goor Hvan, et al. Reduced Cortical thickness of brain areas involved in pain processing in patients with chronic pancreatitis. Clin Gastroenterol Hepatol. 2012;10:434–38.e1.
Shackman AJ, Salomons TV, Slagter HA, Fox AS, Winter JJ, Davidson RJ. The integration of negative affect, pain and cognitive control in the cingulate cortex. Nat Rev Neurosci. 2011;12:154–67.
Boccia M, D’Amico S, Bianchini F, Marano A, Giannini AM, Piccardi L. Different neural modifications underpin PTSD after different traumatic events: an fMRI meta-analytic study. Brain Imaging Behav. 2016;10:226–37.
Lim L, Hart H, Mehta M, Worker A, Simmons A, Mirza K, et al. Grey matter volume and thickness abnormalities in young people with a history of childhood abuse. Psychol Med. 2018;48:1034–46.
Lu LH, Dapretto M, O’Hare ED, Kan E, McCourt ST, Thompson PM, et al. Relationships between brain activation and brain structure in normally developing children. Cereb Cortex. 2009;19:2595–604.
Dickerson BC, Fenstermacher E, Salat DH, Wolk DA, Maguire RP, Desikan R, et al. Detection of cortical thickness correlates of cognitive performance: reliability across MRI scan sessions, scanners, and field strengths. Neuroimage 2008;39:10–18.
Peters S, Van Duijvenvoorde ACK, Koolschijn PCMP, Crone EA. Longitudinal development of frontoparietal activity during feedback learning: contributions of age, performance, working memory and cortical thickness. Dev Cogn Neurosci. 2016;19:211–22.
Seghier ML. The angular gyrus: multiple functions and multiple subdivisions. Neuroscientist. 2013;19:43–61.
Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H, et al. Cognitive reappraisal of emotion: a meta-analysis of human neuroimaging studies. Cereb Cortex. 2014;24:2981–90.
Zhang Y, Padmanabhan A, Gross JJ, Menon V. Development of human emotion circuits investigated using a big-data analytic approach: stability, reliability, and robustness. J Neurosci. 2019;39:7155–72.
Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164:1476–88.
Augsburger M, Galatzer-Levy IR. Utilization of machine learning to test the impact of cognitive processing and emotion recognition on the development of PTSD following trauma exposure. BMC Psychiatry. 2020;20:325.
Scott JC, Matt GE, Wrocklage KM, Crnich C, Jordan J, Southwick SM, et al. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. 2015;141:105–40.
Reynolds S, Carrey N, Jaworska N, Langevin LM, Yang X-R, MacMaster FP. Cortical thickness in youth with major depressive disorder. BMC Psychiatry. 2014;14:83.
Foland‐Ross LC, Sacchet MD, Prasad G, Gilbert B, Thompson PM, Gotlib IH. Cortical thickness predicts the first onset of major depression in adolescence. Int J Dev Neurosci. 2015;46:125–31.
Hegarty CE, Foland-Ross LC, Narr KL, Townsend JD, Bookheimer SY, Thompson PM, et al. Anterior cingulate activation relates to local cortical thickness. Neuroreport 2012;23:420–4.
Squeglia LM, McKenna BS, Jacobus J, Castro N, Sorg SF, Tapert SF. BOLD response to working memory not related to cortical thickness during early adolescence. Brain Res. 2013;1537:59–68.
Author information
Authors and Affiliations
Contributions
All authors contributed meaningfully to the preparation of this manuscript. The first author MCR led the conception and design of the work; led the processing, analysis, and interpretation of the data for the manuscript; drafted and critically revised the work for publication; provided final approval for the version to be published; and is in agreement to be accountable for all aspects of the manuscript. ASS-T contributed to the acquisition and processing of the data for the manuscript and provided critical revisions for important intellectual content. AML and KMC participated in the conception and design of the work and provided critical revisions for intellectual content. JMC provided a substantial contribution in study design and conception, data acquisition and interpretation, providing critical revisions for intellectual content, and provided final approval of the version to be published.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ross, M.C., Sartin-Tarm, A.S., Letkiewicz, A.M. et al. Distinct cortical thickness correlates of early life trauma exposure and posttraumatic stress disorder are shared among adolescent and adult females with interpersonal violence exposure. Neuropsychopharmacol. 46, 741–749 (2021). https://doi.org/10.1038/s41386-020-00918-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-020-00918-y
This article is cited by
-
Relationship between cortical thickness and serotonin 1A receptor binding in bipolar disorder
Translational Psychiatry (2025)
-
Developmental origins of mental health and disorders (DOMHaD): an approach to understanding, preventing and treating psychiatric disorders
Nature Mental Health (2025)
-
Sex-specific associations between self-reported physical activity and PTSD among survivors of sexual violence
Journal of Behavioral Medicine (2024)
-
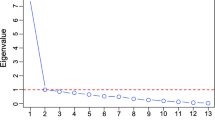
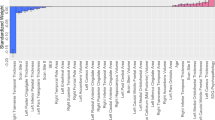
Examining the association between posttraumatic stress disorder and disruptions in cortical networks identified using data-driven methods
Neuropsychopharmacology (2024)
-
Study on the changes of Structural Covariance Network in post-traumatic stress disorder
Brain Imaging and Behavior (2022)