Abstract
Background
Volumetric capnography allows for continuous monitoring of expired tidal volume and carbon dioxide. The slope of the alveolar plateau of the capnogram (SIII) could provide information regarding ventilation homogeneity. We aimed to assess the feasibility of measuring SIII during newborn resuscitation and determine if SIII decreased after surfactant indicating ventilation inhomogeneity improvement.
Methods
Respiratory function traces of preterm infants resuscitated at birth were analysed. Ten capnograms were constructed for each infant: five pre- and post-surfactant. If a plateau was present SIII was calculated by regression analysis.
Results
Thirty-six infants were included, median gestational age of 28.7 weeks and birth weight of 1055 g. Average time between pre- and post-surfactant was 3.2 min. Three hundred and sixty capnograms (180 pre and post) were evaluated. There was adequate slope in 134 (74.4%) capnograms pre and in 100 (55.6%) capnograms post-surfactant (p = 0.004). Normalised for tidal volume SIII pre-surfactant was 18.89 mmHg and post-surfactant was 24.86 mmHg (p = 0.006). An increase in SIII produced an up-slanting appearance to the plateau indicating regional obstruction.
Conclusion
It was feasible to evaluate the alveolar plateau pre-surfactant in preterm infants. Ventilation inhomogeneity increased post-surfactant likely due to airway obstruction caused by liquid surfactant present in the airways.
Impact
-
Volumetric capnography can be used to assess homogeneity of ventilation by SIII analysis.
-
Ventilation inhomogeneity increased immediately post-surfactant administration during the resuscitation of preterm infants, producing a characteristic up-slanting appearance to the alveolar plateau.
-
The best determinant of alveolar plateau presence in preterm infants was the expired tidal volume.
Similar content being viewed by others
Introduction
Capnography allows for continuous measurement of carbon dioxide (CO2) expired from the large conducting and smaller gas exchanging airways during ventilation and can be represented relative to time or volume.1 The latter enables breath by breath analysis of carbon dioxide elimination in relation to tidal volume and by construction of a capnogram waveform can allow calculation of the end-tidal CO2 and physiological dead space.2 Furthermore, volumetric capnography can provide clinicians with valuable knowledge regarding the homogeneity of alveolar ventilation, adequacy of gas exchange and ventilation–perfusion (V/Q) relationships, provided the shape of the capnogram is well-defined.3,4 Three phases of expiration can be determined with the third (or alveolar) phase producing a plateau as pure alveolar gas is exhaled.5 The gradient of the alveolar plateau, SIII, can be used as an index of alveolar ventilation inhomogeneity, with a steeper slope of the plateau phase indicating more severe ventilation inhomogeneity.6 Indeed, a strong correlation between V/Q ratio and SIII obtained from volumetric capnography has been demonstrated in an animal model of acute lung injury.7 Furthermore, the SIII results pre- and post-bronchodilator therapy in children with asthma showed a steeper alveolar plateau prior to treatment resulting from small airway obstruction.8
Spontaneously breathing infants with bronchopulmonary dysplasia have been shown to have an SIII steeper than their non-BPD preterm counterparts, suggestive of disease induced changes to the lung parenchyma adversely affecting V/Q matching.9 We have previously described a steeper SIII in invasively ventilated term or preterm infants who required higher levels of ventilatory support on the neonatal intensive care unit.10 The morphometric changes in alveoli and small airways as infants mature are thought to explain the mechanism behind the decrease in the slope of the alveolar plateau over time from infancy to adolescence, with one study demonstrating a smaller SIII as gestational age advances and tidal volumes increase.11 Constructing volumetric capnograms, however, can be methodologically difficult in the preterm population, in part due to their small tidal volumes, rapid breathing rates and shortened expiratory times.12
Exogenous surfactant is administered during the initial resuscitation of preterm infants at birth to prevent respiratory distress syndrome (RDS) and reduce ventilation–perfusion mismatch. Surfactant therapy can improve lung volume, oxygenation and atelectasis in newborn infants as demonstrated by a post-surfactant increase in functional residual capacity.13 Ventilation inhomogeneity can be assessed by moment analysis of the nitrogen washout curve according to an exponential lung model. Moment ratios, calculated from the percentage of total lung nitrogen volume and number of turnovers, are directly related to ventilation inhomogeneity. In a study of ventilated newborn infants (median gestational age 30 weeks) with RDS, homogeneity of ventilation assessed by the above techniques was determined pre- and post-surfactant. Post surfactant there was a significant drop in moment ratio (p < 0.05), with a single-compartment lung model fitting the washout data better post surfactant suggestive of improved homogeneity of ventilation (p < 0.01).14
Our aims were to describe the feasibility and methodology of analysing the alveolar plateau (SIII) in preterm infants during resuscitation and to report on the changes in ventilation inhomogeneity pre- and post-surfactant administration.
Methods
Subjects
This was a retrospective analysis of respiratory function traces collected from a previous randomised controlled trial involving resuscitation of preterm infants (London Riverside NHS Research Ethics Committee: 16/LO/1718), with consent from the original study stating the data could be used to inform future research.
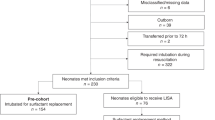
The traces of preterm infants less than 34 completed weeks of gestation were analysed if the infants required resuscitation with intubation and administration of endotracheal surfactant on the labour ward.
Protocol
Infants were resuscitated using a continuous flow, pressure-limiting device (Neopuff infant resuscitator, Fisher and Paykel Healthcare, New Zealand). Management post-delivery was performed according to the Neonatal Life Support protocol (Resuscitation Council, UK) and the European Consensus Guidelines on RDS.15 Initial peak inspiratory pressures (PIP) of 20–25 cm H2O with a positive end-expiratory pressure (PEEP) of 4–5 cm H2O were used and increased according to clinician discretion if inadequate chest rise, no response to positive pressure ventilation or poor oxygenation. The fraction of inspired oxygen (FiO2) was initially set at 0.21 and was increased as necessary to maintain oxygen saturations between 92 and 96%. If infants were not responding to positive pressure ventilation via face mask they were intubated with shouldered Cole’s endotracheal tubes (ETTs) and given surfactant. The surfactant liquid preparation (Curosurf, Chiesi Italy) was administered via the ETT at a dose of 200 mg/kg.
Respiratory function monitoring
Respiratory function monitoring was recorded via an NM3 respiratory profile monitor (Philips, Respironics) with customised Spectra software (Grove Medical, UK). The NM3 monitor has a combined flow, pressure, and mainstream carbon dioxide (CO2) sensor (Capnostat-5) with a dead space of 0.8 ml and a CO2 response time of less than 60 ms according to the manufacturer’s specifications. The NM3 Capnostat-5 device was placed into the ventilatory circuit between the Neopuff device and the ETT. During resuscitation the respiratory monitor displayed expired tidal volume, end-tidal CO2, peak inspiratory pressure and PEEP. Respiratory function monitoring traces analysed were those following intubation immediately pre- and post-surfactant administration once the ETT was reconnected to the Neopuff, prior to transferring the infant to the Neonatal Intensive Care Unit.
Volumetric capnography indices
Data were extracted from the Spectra software into an Excel file with a sampling rate of 100 Hz. Ten volumetric capnograms were constructed for each infant: five pre and five post endotracheal surfactant administration. The flow signal was integrated over time to calculate the expired tidal volume. The anatomical dead space (VdANA) was calculated using the modified Bohr Enghoff (BE) equation (12): VdANA (ml) = Vte * (PEtCO2 − PemeanCO2)/PEtCO2, where Vte is the expired tidal volume (ml), PEtCO2 is the end-tidal CO2 (mmHg) and PemeanCO2 is the volume average mean expired CO2 (mmHg). The mean expired CO2 is calculated as an integrated function of CO2 from the end of inspiration to the end of expiration. Partial pressure concentrations of expired carbon dioxide were reported rather than fractional concentrations due to the methodological feasibility of the former, in that exhaled CO2 as detected by our NM3 monitor was reported in mmHg. The expiratory time (ms) was taken from the start of negative flow to where the flow equals zero. The value of anatomical dead space calculated also includes the contribution from the apparatus dead space, which includes the ETT and NM3 Capnostat-5. The BE equation method was used preferentially over the method described by Fletcher using Fowler’s equal triangles as the BE method has been shown to be feasible for dead space measurements regardless of both the shape of the volumetric capnogram and the presence or absence of an alveolar plateau.16,17
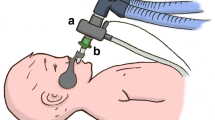
The volumetric capnogram was split into three phases: phase I, phase II and phase III (Fig. 1).5 Phase I represents the first part of expiration whereby gas was expired from the large conducting, non-gas exchanging airways. Phase II corresponds to the mid-part of expiration and contains a mixture of gas from the large airways with alveolar gas from distal airways. Phase III describes the final phase of expiration with pure alveolar gas being expired with a resulting alveolar plateau. The gradient (slope) of the phase III part of the capnogram is called SIII. The shape of each capnogram was evaluated and if an alveolar plateau was present SIII was calculated by fitting a regression line to this final phase, which relied on dynamic measurements taking each individual capnogram shape into account rather than calculating measurements at a fixed portion of the expired tidal volume, with a minimum of ten sample points required for SIII.18,19 The average values obtained from each of the five capnograms pre- and post-surfactant were calculated for each infant. Values of SIII were normalised to tidal volume to account for anthropometric differences.10,11 Furthermore, we present SIII values normalised to PemeanCO2 (ml−1) to account for differences in expired CO2. Feasibility of SIII analysis for each volumetric capnogram was assessed individually if an alveolar plateau was present allowing for SIII calculation. The feasibility was expressed as a percentage out of total number of capnograms analysed (Fig. 1). All evaluations were made by the same investigator who was blinded to the infant demographics at the time of analysis.
Sample size
In a previous study the mean difference in normalised SIII between preterm infants who developed BPD and those who did not matched for a postmenstrual age of 44 weeks at study was 10.6 l−1 with a standard deviation of 14.4.9 To detect a significant difference of 10.6 in the SIII of infants pre- and post-surfactant with 85% power at the 5% significance level a sample size of 35 infants was required.
Statistical analyses
The data were tested for normality using the Shapiro Wilk test and found to be non-normally distributed. Nonparametric tests were used with the Wilcoxon-matched pairs test to determine the change in capnography indices pre- and post-surfactant administration. The feasibility of SIII analysis was calculated as the percentage of the total that demonstrated presence of an alveolar plateau and allowed for SIII calculation. Differences between those capnograms that demonstrated an alveolar plateau and those that did not were assessed for statistical significance using the Mann–Whitney U test. The factors that were significantly different (p < 0.05) were inserted into a binary logistic regression model with the presence of alveolar plateau as the outcome variable. The performance of the characteristics that were significant in determining the presence of alveolar plateau was assessed by receiver operator characteristic (ROC) curve analysis and estimation of the corresponding area under the curve (AUC). Statistical analysis was performed using SPSS software version 26.0 (SPSS, New York).
Results
Thirty-six infants were studied. They had a median (interquartile range, IQR) gestational age (GA) at birth of 28.7 (26.1–30.8) weeks, a birth weight of 1055 (811–1357) g and a birth weight z-score of −0.49 (−1.12 to 0.03) (Table 1). Eighteen infants (50.0%) were male. Fifteen infants (41.7%) were born by vaginal delivery and 21 infants (58.3%) by caesarean section. Thirty-one infants (86.1%) were exposed to antenatal corticosteroids. Three infants (8.3%) died prior to discharge.
The median time between pre- and post-surfactant analysis was 3.2 (1.7–4.8) minutes. The median end-tidal CO2 level pre-surfactant was 43.2 (29.6–51.7) mmHg and 33.1 (27.0–44.0) mmHg post-surfactant (p = 0.044). The median expired tidal volume decreased immediately post-surfactant administration compared to pre-surfactant (6.6 versus 9.3 ml/kg; p < 0.001). The median anatomical dead space to tidal volume ratio (Vd/Vt) was higher in infants post-surfactant compared to pre-surfactant (0.58 versus 0.54; p = 0.012). There was no significant difference in the maximal peak inspiratory pressure (PIP) used pre- and post-surfactant (p = 0.383) (Table 2).
Three hundred and sixty volumetric capnograms were evaluated for adequate slope definition (180 pre- and 180 post-surfactant). The alveolar plateau was present and analysable in 134 (74.4%) capnograms pre-surfactant and in 100 (55.6%) capnograms immediately post-surfactant (p = 0.004). The median (IQR) SIII pre-surfactant was 1.58 (0.76–3.09) mmHg/ml and 2.44 (1.22–5.23) mmHg/ml post-surfactant (p = 0.005). The median (IQR) normalised for tidal volume SIII pre-surfactant was 18.89 (9.32–29.08) mmHg and post-surfactant was 24.86 (16.04–31.18) mmHg (p = 0.006). The median (IQR) normalised for PemeanCO2 SIII pre-surfactant was 0.08 (0.03–0.20) ml−1 and post-surfactant was 0.16 (0.06–0.43) ml−1 (p = 0.003). The expiratory time of capnograms with an alveolar plateau was 572 (437–675) ms pre-surfactant compared to 499 (410–591) ms post-surfactant (p = 0.051).
Of the 180 volumetric capnograms that were constructed pre-surfactant administration the alveolar plateau was present in more mature [median GA 28.9 (27.0–30.1) weeks] compared to less mature infants [median GA 27.9 (24.9–30.1) weeks; p = 0.013]. There was no significant difference in birth weight where an alveolar plateau was present [1.1 (0.84–1.36) kg] compared to where it was absent [0.87 (0.66–1.29) kg; p = 0.071). The median expiratory time in all 180 capnograms was 540 ms, with the expiratory time significantly longer in those capnograms demonstrating presence of an alveolar plateau [580 (450–730) ms] compared to those without [390 (295–550) ms; p < 0.001]. Expired tidal volumes were also greater if an alveolar plateau was present [10.6 (8.4–16.8) ml/kg] compared to when it was absent [5.3 (4.3–6.7) ml/kg; p < 0.001). The correlation between expiratory time and expired tidal volume was moderate (r = 0.48; p < 0.001). Binary logistic regression analysis with gestational age, expiratory time and expired tidal volume as covariates showed that all three covariates remained independently associated with the presence of an alveolar plateau (Table 3). ROC analysis demonstrated an AUC of 0.92 for expired tidal volume in determining the presence of an alveolar plateau. A tidal volume greater than or equal to 7.0 ml/kg had 92% sensitivity and 82% specificity in discriminating whether a capnogram had an alveolar plateau (Table 4).
Discussion
We have demonstrated the feasibility of using volumetric capnography during resuscitation of preterm infants and that the presence of an alveolar plateau is best determined by a larger expiratory tidal volume. Furthermore, we have described an increase in ventilation inhomogeneity immediately post-surfactant therapy.
The increase in SIII and decrease in expired tidal volume that occurs immediately post-surfactant may be explained by the liquid surfactant preparation obstructing the small airways. Indeed complete airway obstruction post-surfactant administration in the delivery room has previously been described in a cohort of 16 infants, with similar changes in expired tidal volume to our current findings.20 The immediate increase in ventilation inhomogeneity could explain why some infants exhibit an acute deterioration following surfactant administration.21 The gradient of alveolar plateau post-surfactant demonstrated a ‘shark’s fin’ appearance to the shape of the capnogram similar to that observed in asthmatic patients presenting with small airway inflammation and obstruction prior to bronchodilator therapy.22,23
The feasibility in the current study of determining an alveolar plateau pre-surfactant was 74%; however, post-surfactant dropped to 56% secondary to the above-described obstructive findings. Previous descriptions of volumetric capnography derived calculations of dead space and SIII have been evaluated in one newborn animal model of ventilated surfactant-depleted lungs secondary to bronchoalveolar lavage (BAL). The number of capnograms without alveolar plateaus was significantly decreased following BAL, with no plateau phase in over three quarters of those with expiratory times of less than 200 ms, and with a feasibility rate of 50% in surfactant-depleted lungs increasing to as high as 90% in healthy lungs. The average expiratory time in our cohort pre-surfactant was longer at 540 ms and may explain our higher percentage of feasibility.17
Expiratory tidal volume and expiratory time were better determinants of alveolar plateau presence in our study than birth weight. Indeed a study performed in spontaneously breathing infants has described how capnography wave patterns are not affected by body weight per se but rather by maturity.24 By normalising the SIII to tidal volume we allowed ventilation inhomogeneity to be interrogated independently of significant changes in slope with expired tidal volume. That the best determinant of a presence of an alveolar plateau was the expiratory tidal volume, was an unexpected finding. A computer-simulated model has reported changes in ventilation inhomogeneity calculated by lung clearance index to be influenced by lung volume and dead space to tidal volume ratio, with reduced indices often misinterpreted as more homogeneous distribution of ventilation, suggesting ventilation homogeneity indices need to be considered in the context of tidal volumes and peak inspiratory pressures.25 We suggest the change in expiratory tidal volume and anatomical dead space to tidal volume ratio pre- and post-treatment in the current study was due to the surfactant preparation partially blocking exhalation of expiratory gas and not due to changes in ventilatory pressures influencing tidal volume delivery. It needs to be highlighted that values of SIII should be interpreted with caution when significant changes in tidal volume occur. The presence of an alveolar plateau could indeed indicate that delivery of tidal volume to the alveoli is large enough to overcome the dead space and allow for adequate alveolar ventilation and clearance of carbon dioxide.
The values of normalised for tidal volume SIII pre-surfactant (median 18.9 mmHg) in our study are higher than reported in the literature. Using the same method of analysis, we have previously demonstrated normalised for tidal volume values of SIII pre-extubation of 16.5 mmHg in preterm and 13.5 mmHg in term infants, measured at 30 and 40 weeks corrected gestational age, respectively.10 The higher values in the current study of infants, measured at a less mature gestational age of 28 weeks, may relate to the morphometric changes to alveolar lung growth that occur during maturation with a corresponding decrease in the slope of phase III.11 We further speculate that atelectasis and greater V/Q mismatch immediately post birth, prior to surfactant, might explain the larger values of SIII, with improvement in respiratory disease and hence lower SIII in those infants studied at a later chronological time point. Contrary to this potential explanation however is a study of preterm infants with bronchopulmonary dysplasia measured at 44 weeks corrected gestational age, in which such infants had normalised for fraction of expired CO2 SIII values of 26.8 l−1 compared to term controls of 14.8 l−1. Suggesting that after the initial convalescent phase of disease, evolution of parenchymal lung changes with progressive V/Q mismatch may indeed increase indices of ventilation inhomogeneity.9 That study, however, was performed in spontaneously breathing infants and as such employed different equipment (face mask) and methodology of SIII calculation, hence, may not be fully comparable to our study. Furthermore, we acknowledge comparison of SIII between different studies may be difficult to evaluate given different rates of exhaled carbon dioxide; we have, therefore, presented SIII normalised to PemeanCO2 to account for this.
Our study has strengths and some limitations. This is the first study to evaluate the shape of the volumetric capnogram and to describe SIII during the resuscitation immediately post birth in preterm infants. Despite often a lack of alveolar plateau in critically ill neonates, attributable to small tidal volumes and V/Q mismatch in respiratory disease, even in plateau absence some clinical information from the capnogram can still be useful with end-tidal carbon dioxide being used to non-invasively estimate arterial carbon dioxide.26 Our findings may be used to inform clinicians regarding the effect of surfactant on ventilatory parameters immediately post administration; indeed, slower administration may be required to avoid partial airway obstruction. Volumetric capnography may further be useful in adjustment of ventilatory parameters post-surfactant administration until ventilation inhomogeneity improves.
Advances in technology have enabled development of mainstream and sidestream capnography devices with low apparatus dead space (<0.8 ml), low sampling rates and fast response times (<60 ms), making them more suited to the neonatal population;12,27,28 indeed, we used such a mainstream device in our current study. The use of Cole’s shouldered ETTs in minimising leak,29 together with the low dead space measuring apparatus30 allowed for calculation and construction of volumetric capnograms which was crucial to the methodology employed. The steeper alveolar plateau and increase in SIII secondary to small airway obstruction inhibited accurate interpretation of the capnogram shape in some infants post-surfactant and we were therefore only able to comment on the feasibility of SIII analysis in pre-surfactant volumetric capnograms reducing the numbers for analysis; however, 36 infants and 180 capnograms met our sample size calculation. Determining the PEtCO2 value when the alveolar plateau is poorly defined and short may not be representative of the alveolar CO2, we, therefore, determined the PEtCO2 at the end of expiration defined by the end of expiratory flow. Values of arterial carbon dioxide are not routinely collected on the labour ward and so we could not comment on the alveolar dead space which may influence ventilation inhomogeneity. In choosing not to analyse the data by automation using a fixed portion of phase III, our results may be affected by subjectivity; however, this study was the first to describe alveolar plateau analysis during resuscitation of premature infants. Future studies could incorporate automated analysis which would improve the potential for real time utilisation.
In conclusion, evaluation of the alveolar plateau was feasible in pre-surfactant volumetric capnograms and expired tidal volume was the major determinant of an alveolar plateau presence. Ventilation inhomogeneity as assessed by SIII increased immediately post-surfactant administration likely due to airway obstruction caused by the liquid surfactant in the small airways.
References
Verscheure, S., Massion, P. B., Verschuren, F., Damas, P. & Magder, S. Volumetric capnography: lessons from the past and current clinical applications. Crit. Care 20, 184 (2016).
Suarez-Sipmann, F., Bohm, S. H. & Tusman, G. Volumetric capnography: the time has come. Curr. Opin. Crit. Care 20, 333–339 (2014).
Balogh, A. L. et al. Capnogram slope and ventilation dead space parameters: comparison of mainstream and sidestream techniques. Br. J. Anaesth. 117, 109–117 (2016).
Tolnai, J. et al. Volumetric but not time capnography detects ventilation/perfusion mismatch in injured rabbit lung. Front. Physiol. 9, 1805 (2018).
Fletcher, R. Airway deadspace, end-tidal CO2, and Christian Bohr. Acta Anaesthesiol. Scand. 28, 408–411 (1984).
Stromberg, N. O. & Gustafsson, P. M. Ventilation inhomogeneity assessed by nitrogen washout and ventilation-perfusion mismatch by capnography in stable and induced airway obstruction. Pediatr. Pulmonol. 29, 94–102 (2000).
Tusman, G., Suarez-Sipmann, F., Bohm, S. H., Borges, J. B. & Hedenstierna, G. Capnography reflects ventilation/perfusion distribution in a model of acute lung injury. Acta Anaesthesiol. Scand. 55, 597–606 (2011).
Cracco, O., Degrugilliers, L., Rames, C., Becourt, A. & Bayat, S. Change in capnogram waveform is associated with bronchodilator response and asthma control in children. Pediatr. Pulmonol. 54, 698–705 (2019).
Fouzas, S. et al. Volumetric capnography in infants with bronchopulmonary dysplasia. J. Pediatr. 164, 283–288 (2014).
Dassios, T., Dixon, P., Williams, E. & Greenough, A. Volumetric capnography slopes in ventilated term and preterm infants. Physiol. Meas. 41, 055001 (2020).
Ream, R. S. et al. Volumetric capnography in children. Influence of growth on the alveolar plateau slope. Anesthesiology 82, 64–73 (1995).
Schmalisch, G. Current methodological and technical limitations of time and volumetric capnography in newborns. Biomed. Eng. Online 15, 104 (2016).
Cotton, R. B. et al. The physiologic effects of surfactant treatment on gas exchange in newborn premature infants with hyaline membrane disease. Pediatr. Res. 34, 495–501 (1993).
Sandberg, K. L., Lindstrom, D. P., Sjoqvist, B. A., Parker, R. A. & Cotton, R. B. Surfactant replacement therapy improves ventilation inhomogeneity in infants with respiratory distress syndrome. Pediatr. Pulm. 24, 337–343 (1997).
Sweet, D. G. et al. European Consensus Guidelines on the management of respiratory distress syndrome—2019 Update. Neonatology 115, 432–450 (2019).
Wenzel, U., Wauer, R. R. & Schmalisch, G. Comparison of different methods for dead space measurements in ventilated newborns using CO2-volume plot. Intensive Care Med. 25, 705–713 (1999).
Proquitte, H., Krause, S., Rudiger, M., Wauer, R. R. & Schmalisch, G. Current limitations of volumetric capnography in surfactant-depleted small lungs. Pediatr. Crit. Care Med. 5, 75–80 (2004).
Gravenstein, J. S. Capnography. 2nd edn. (Cambridge University Press, 2011).
Schwardt, J. D., Neufeld, G. R., Baumgardner, J. E. & Scherer, P. W. Noninvasive recovery of acinar anatomic information from CO2 expirograms. Ann. Biomed. Eng. 22, 293–306 (1994).
Schmolzer, G. M., Kamlin, C. O., Dawson, J. A., Morley, C. J. & Davis, P. G. Tidal volume delivery during surfactant administration in the delivery room. Intensive Care Med. 37, 1833–1839 (2011).
Tarawneh, A., Kaczmarek, J., Bottino, M. N. & Sant’anna, G. M. Severe airway obstruction during surfactant administration using a standardized protocol: a prospective, observational study. J. Perinatol. 32, 270–275 (2012).
Nik Hisamuddin, N. A. et al. Correlations between capnographic waveforms and peak flow meter measurement in emergency department management of asthma. Int. J. Emerg. Med. 2, 83–89 (2009).
You, B., Peslin, R., Duvivier, C., Vu, V. D. & Grilliat, J. P. Expiratory capnography in asthma: evaluation of various shape indices. Eur. Respir. J. 7, 318–323 (1994).
Tirosh, E., Bilker, A., Bader, D. & Cohen, A. Capnography in spontaneously breathing preterm and term infants. Clin. Physiol. 21, 150–154 (2001).
Schmalisch, G., Proquitte, H., Roehr, C. C. & Wauer, R. R. The effect of changing ventilator settings on indices of ventilation inhomogeneity in small ventilated lungs. BMC Pulm. Med. 6, 20 (2006).
McEvedy, B. A., McLeod, M. E., Kirpalani, H., Volgyesi, G. A. & Lerman, J. End-tidal carbon dioxide measurements in critically ill neonates: a comparison of side-stream and mainstream capnometers. Can. J. Anaesth. 37, 322–326 (1990).
Williams, E., Dassios, T. & Greenough, A. Assessment of sidestream end-tidal capnography in ventilated infants on the neonatal unit. Pediatr. Pulmonol. 55, 1468–1473 (2020).
Hagerty, J. J., Kleinman, M. E., Lyons, A. C. & Krauss, B. Accuracy of a new low-flux sidestream capnography technology in newborns. Pediatr. Res. 47, 360a–360aa (2007).
Hird, M., Greenough, A. & Gamsu, H. Gas trapping during high frequency positive pressure ventilation using conventional ventilators. Early Hum. Dev. 22, 51–56 (1990).
Frey, U., Stocks, J., Coates, A., Sly, P. & Bates, J. Specifications for equipment used for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/American Thoracic Society. Eur. Respir. J. 16, 731–740 (2000).
Acknowledgements
E.E.W. and K.A.H. were funded by the Charles Wolfson Charitable Trust. E.E.W. is supported by a non-conditional educational grant from SLE. This research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
E.E.W., T.D., K.A.H. and A.G. made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafted the article and revised it critically for important intellectual content; and all authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
This was a retrospective analysis of respiratory function traces collected from a previous randomised control trial involving resuscitation of preterm infants (London Riverside NHS Research Ethics Committee: 16/LO/1718), with consent from the original study stating the data could be used to inform future research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Williams, E.E., Dassios, T., Hunt, K.A. et al. Volumetric capnography pre- and post-surfactant during initial resuscitation of premature infants. Pediatr Res 91, 1551–1556 (2022). https://doi.org/10.1038/s41390-021-01578-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01578-4