Abstract
Background
There is extensive evidence that Holder pasteurization (HoP) (30 min at 62.5 °C) has harmful effects on the bioactivities of human milk (HM). We previously demonstrated that lowering HoP temperature is sufficient to inactivate Cytomegalovirus (HCMV). Here, we analyzed the effect of lowering time/temperature on the antiviral activity against HCMV and IgA levels of HM.
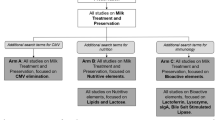
Methods
Eighty HM samples from five mothers were pasteurized in a range of temperature (62.5–56 °C) and time (40–10 min) in a conventional setting of Human Milk Bank. Unpasteurized HM from each mother was used as control. The samples were assayed against HCMV-AD169 strain in cell cultures and IgA levels were determined by ELISA.
Results
All HM samples exhibited anti-HCMV activity, to a different extent. An improvement of antiviral activity was observed in samples treated at 60, 58 and 56 °C compared to those at 62.5 °C, with ID50 values near those of unpasteurized milk. Similarly, better retention in IgA levels was observed by reducing the temperature of treatment.
Conclusions
We demonstrated that a 2.5 °C reduction of heat treatment significantly preserved the IgA content and fully restored the anti-HCMV activity of HM, supporting this variant of HoP as a valid alternative to preserve HM bioactivities.
Impact
-
This work questions the standard HoP and opens the debate on whether the pasteurization temperature commonly used in Human Milk Banks should be lowered to better preserve the biological components of the milk.
-
A reduction of HoP temperature at 60 °C determined a significant preservation of anti-HCMV activity and IgA content of donor HM, compared to standard HoP.
-
This alternative HoP is highly feasible compared to other substitute pasteurization techniques, since it would employ the same pasteurizer equipment found in most Human Milk Banks.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
All data generated or analyzed during this study are included in this published article.
References
Thome, U. H. & Boquien, C.-Y. Human milk: an ideal food for nutrition of preterm newborn. DOHAD (Developmental Origin of Health and Adult Diseases) Context and Nutritional Programming. Front. Pediatr. 6, 295 (2018).
Lönnerdal, B. Bioactive proteins in human milk—potential benefits for preterm infants. Clin. Perinatol. 44, 179–191 (2017).
Abrams, S. A., Landers, S., Noble, L. M. & Poindexter, B. B. Donor human milk for the high-risk infant: preparation, safety, and usage options in the United States. Pediatrics 139, e20163440 (2017).
Li, Y. et al. Pasteurization procedures for donor human milk affect body growth, intestinal structure, and resistance against bacterial infections in preterm pigs. J. Nutr. 147, 1121–1130 (2017).
Quigley, M. & McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 2014, CD002971 (2014).
Breastfeeding, S. O. et al. Breastfeeding and the use of human milk. Pediatrics 129, e827–e841 (2012).
Weaver, G. et al. Recommendations for the establishment and operation of Human Milk Banks in Europe: a consensus statement from the European Milk Bank Association (EMBA). Front. Pediatr. 7, 53 (2019).
Gayà, A. & Calvo, J. Improving pasteurization to preserve the biological components of donated human milk. Front. Pediatr. 6, 288 (2018).
Pitino, M. A., O’connor, D. L., McGeer, A. J. & Unger, S. The impact of thermal pasteurization on viral load and detectable live viruses in human milk and other matrices: a rapid review. Appl. Physiol. Nutr. Metab. 46, 10–26 (2021).
Paulaviciene, I. J. et al. The effect of prolonged freezing and Holder pasteurization on the macronutrient and bioactive protein compositions of human milk. Breastfeed Med. 15, 583–588 (2020).
García-Lara, N. R. et al. Effect of Holder pasteurization and frozen storage on macronutrients and energy content of breast milk. J. Pediatr. Gastroenterol. Nutr. 57, 377–382 (2013).
Peila, C. et al. The effect of Holder pasteurization on nutrients and biologically-active components in donor human milk: a review. Nutrients 8, 477 (2016).
Picaud, J. C. & Buffin, R. Human milk-treatment and quality of banked human milk. Clin. Perinatol. 44, 95–119 (2017).
Moro, G. E. et al. Processing of donor human milk: Update and recommendations from the European Milk Bank Association (EMBA). Front. Pediatr. 7, 49 (2019).
Aceti, A. et al. Effect of alternative pasteurization techniques on human milk’s bioactive proteins. J. Pediatr. Gastroenterol. Nutr. 70, 508–512 (2020).
Giribaldi, M. et al. A preliminary assessment of HTST processing on donkey milk. Vet. Sci. 4, 50 (2017).
Escuder-Vieco, D., Espinosa-Martos, I., Rodríguez, J. M., Fernández, L. & Pallás-Alonso, C. R. Effect of HTST and Holder pasteurization on the concentration of immunoglobulins, growth factors, and hormones in donor human milk. Front. Immunol. 9, 2222 (2018).
Wesolowska, A. et al. New achievements in high-pressure processing to preserve human milk bioactivity. Front. Pediatr. 6, 323 (2018).
Kontopodi, E. et al. Effects of high-pressure processing, UV-C irradiation and thermoultrasonication on donor human milk safety and quality. Front. Pediatr. 10, 305 (2022).
Christen, L., Lai, C. T., Hartmann, B., Hartmann, P. E. & Geddes, D. T. Ultraviolet-C irradiation: a novel pasteurization method for donor human milk. PLoS One 8, e68120 (2013).
Leite, J. A. S. et al. The effect of microwave-assisted heating on bioactive and immunological compounds in donor human milk. LWT 161, 113306 (2022).
Martysiak-Żurowska, D., Malinowska-Pańczyk, E., Orzołek, M., Kusznierewicz, B. & Kiełbratowska, B. Effect of microwave and convection heating on selected nutrients of human milk. Food Chem. 369, 130958 (2022).
Gayà, A. et al. Analysis of thermal sensitivity of human Cytomegalovirus assayed in the conventional conditions of a human milk bank. Front. Pediatr. 9, 640638 (2021).
Czank, C., Prime, D. K., Hartmann, B., Simmer, K. & Hartmann, P. E. Retention of the immunological proteins of pasteurized human milk in relation to pasteurizer design and practice. Pediatr. Res. 66, 374–379 (2009).
Leydold, S. M. et al. Chikungunya virus and the safety of plasma products. Transfusion 52, 2122–2130 (2012).
Donalisio, M. et al. Anti-cytomegalovirus activity in human milk and colostrum from mothers of preterm infants. J. Pediatr. Gastroenterol. Nutr. 67, 654–659 (2018).
Kabani, N. & Ross, S. A. Congenital Cytomegalovirus infection. J. Infect. Dis. 221, S9–S14 (2020).
Manicklal, S., Emery, V. C., Lazzarotto, T., Boppana, S. B. & Gupta, R. K. The “silent” global burden of congenital Cytomegalovirus. Clin. Microbiol. Rev. 26, 86–102 (2013).
Hamprecht, K. & Goelz, R. Postnatal Cytomegalovirus infection through human milk in preterm infants: transmission, clinical presentation, and prevention. Clin. Perinatol. 44, 121–130 (2017).
Trombetta, C. M., Viviani, S., Montomoli, E. & Marchi, S. Seroprevalence of antibodies to cytomegalovirus in pregnant women in the Apulia region (Italy). J. Prev. Med. Hyg. 62, E372–E376 (2021).
Francese, R. et al. Human milk glycosaminoglycans inhibit cytomegalovirus and respiratory syncytial virus infectivity by impairing cell binding. Pediatr. Res. 1–8. https://doi.org/10.1038/s41390-022-02091-y (2022).
Cagno, V. et al. In vitro evaluation of the antiviral properties of Shilajit and investigation of its mechanisms of action. J. Ethnopharmacol. 166, 129–134 (2015).
Civra, A. et al. Human colostrum and derived extracellular vesicles prevent infection by human rotavirus and respiratory syncytial virus in vitro. J. Hum. Lact. 37, 122–134 (2021).
Francese, R. et al. Anti-Zika virus and anti-Usutu virus activity of human milk and its components. PLoS Negl. Trop. Dis. 14, 1–24 (2020).
Conzelmann, C. et al. Storage-dependent generation of potent anti-ZIKV activity in human breast milk. Viruses 11, 591 (2019).
Donalisio, M. et al. High temperature-short time pasteurization has a lower impact on the antiviral properties of human milk than Holder pasteurization. Front. Pediatr. 6, 304 (2018).
Rio-Aige, K. et al. The breast milk immunoglobulinome. Nutrients 13, 1810 (2021).
Young, B. E., Murphy, K., Borman, L. L., Heinrich, R. & Krebs, N. F. Milk Bank pooling practices impact concentrations and variability of bioactive components of donor human milk. Front. Nutr. 7, 1–6 (2020).
Donalisio, M. et al. Extracellular vesicles in human preterm colostrum inhibit infection by human Cytomegalovirus in vitro. Microorganisms 8, 1087 (2020).
Gidrewicz, D. A. & Fenton, T. R. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 14, 216 (2014).
Wedekind, S. I. S. & Shenker, N. S. Antiviral properties of human milk. Microorganisms 9, 715 (2021).
Kothari, A. et al. Preservation of anti-cytomegalovirus activity in human milk following high-pressure processing compared to Holder pasteurization. Front. Nutr. 9, 1–7 (2022).
Dussault, N. et al. Comparison of the effect of Holder pasteurization and high-pressure processing on human milk bacterial load and bioactive factors preservation. J. Pediatr. Gastroenterol. Nutr. 72, 756–762 (2021).
Müller, K. et al. Holder pasteurization: comparison of water-bath and dry-tempering devices. Front. Pediatr. 10, 1122 (2022).
Irazusta, A. et al. High-pressure homogenization and high hydrostatic pressure processing of human milk: preservation of immunological components for human milk banks. J. Dairy Sci. 103, 5978–5991 (2020).
Adhisivam, B. et al. Effect of Holder pasteurization on macronutrients and immunoglobulin profile of pooled donor human milk. J. Matern. Fetal Neonatal Med. 32, 3016–3019. https://doi.org/10.1080/14767058.2018.1455089 (2019).
Escuder-Vieco, D. et al. High-temperature short-time and Holder pasteurization of donor milk: impact on milk composition. Life 11, 114 (2021).
Kontopodi, E. et al. High-temperature short-time preserves human milk’s bioactive proteins and their function better than pasteurization techniques with long processing times. Front. Pediatr. 9, 798609 (2022).
Klotz, D. et al. High-temperature short-time treatment of human milk for bacterial count reduction. Front. Pediatr. 6, 359 (2018).
Capriati, T. et al. A modified Holder pasteurization method for donor human milk: preliminary. Data. Nutr. 11, 1139 (2019).
Jandová, M. et al. Bacillus cereus as a major cause of discarded pasteurized human banked milk: a single human milk bank experience. Foods 10, 1–15 (2021).
Jandová, M. et al. Quantitative risk assessment of Bacillus cereus growth during the warming of thawed pasteurized human banked milk using a predictive mathematical model. Foods 11, 1037 (2022).
Lewin, A., Delage, G., Bernier, F. & Germain, M. Banked human milk and quantitative risk assessment of Bacillus cereus infection in premature infants: a simulation study. Can. J. Infect. Dis. Med. Microbiol. 2019, Article ID 6348281 (2019).
Lewin, A. et al. Bacillus cereus infection in neonates and the absence of evidence for the role of banked human milk: case reports and literature review. Infect. Control. Hosp. Epidemiol. 40, 787–793 (2019).
Hoque, S. A. et al. Transient heating of expressed breast milk up to 65°C inactivates HIV-1 in milk: a simple, rapid, and cost-effective method to prevent postnatal transmission. J. Med. Virol. 85, 187–193 (2013).
Kenji Yamato, H. et al. Inactivation of lymphocyte-transforming activity of human T-cell leukemia virus type I by heat. J. Cancer Res. 77, 13–15 (1986).
Donalisio, M. et al. Inactivation of high-risk human papillomaviruses by Holder pasteurization: implications for donor human milk banking. J. Perinat. Med. 42, 1–8 (2014).
Acknowledgements
The authors acknowledge Marian Forteza from Illustrate Science (www.illustrate-science.com) for the design of Fig. 2a. The authors also want to express their gratitude to the mothers who selflessly donated samples of their milk for the realization of this study.
Funding
This work was supported by a grant (CDIi20/08) from Comissió de Docencia I Investigació de la Fundació Banc de Sang I Teixits de les Illes Balears. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
M.D., A.G.: substantial contributions to conception and design. I.A., J.C., M.R., S.G. M.L.: acquisition of data. I.A., J.C., M.R.: analysis and interpretation of data. I.A., J.C.: drafting the article. M.D., A.G., D.L.: revising the article critically for important intellectual content. All authors: final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was revised and approved by the Ethics Committee of Balearic Islands (CEIC IB; IB 5024/22 PI). Each milk donor signed a written consent form for the use of donated milk for research purposes, where the mother’s and infant’s data protection were assured.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arduino, I., Calvo, J., Rittà, M. et al. Impact of time-temperature combinations on the anti-Cytomegalovirus activity and biological components of human milk. Pediatr Res 94, 956–964 (2023). https://doi.org/10.1038/s41390-023-02606-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-023-02606-1