Abstract
The United States neonatal and infant mortality rates have declined substantially over the last six decades. Despite these reductions, significant racial disparities in mortality and other important outcomes have persisted. While increased risk of preterm birth is a major contributor to these differences, racial inequities in risk-adjusted outcomes such as gestational age-specific and major congenital anomaly-associated mortality remain. Race-specific differences in inter- and intra-neonatal intensive care unit (NICU) practices associated with worse outcomes for infants of color suggest opportunities for reducing these disparate health outcomes during and after NICU hospitalization. Identifying NICU-based contributing factors and implementing factor-specific improvement strategies can lead to more equitable outcomes. In this review, we describe examples of racial inequities in risk-adjusted NICU outcomes and inter- and intra-NICU practices associated with worse outcomes for infants of color, provide an overview of current approaches to health equity in NICU care, and identify opportunities, sustainable strategies, and accountabilities for more equitable care and support of NICU patients and, quite importantly, their families.
Impact
-
Characterize racial inequities in risk-adjusted neonatal intensive care unit (NICU) outcomes and inter- and intra-NICU practices associated with worse outcomes for infants of color.
-
Provide an overview of current trends in and approaches to health equity in NICU care.
-
Discuss strategies for implementing and sustaining more equitable care and support for infants and families during NICU hospitalization.
Similar content being viewed by others
Background
Infant health outcomes are among a wide range of health conditions in the United States that are affected by racial and ethnic inequities. Like other social factors, these inequities are driven by structural, institutional, individual, and internalized forces.1,2 Because race and ethnicity are poor proxies for biology—they are social constructs—these disparities are not inevitable but could be addressed by targeted interventions.
Infant outcomes have substantially improved over the last century, but racial and ethnic inequities have persisted. Much of this persistence has resulted from differences in risk at birth (e.g., preterm birth rates) which have proven difficult to mitigate. Conversely, some success has been achieved in reducing disparate outcomes by focusing on high-risk newborns. Recent evidence and promising interventions suggest strategies—which can be effective, not only to improve overall infant outcomes but also to reduce racially and ethnically disparate outcomes—for infants assured access to high quality neonatal intensive care.
The terms “disparity” and “inequity” are often used interchangeably. While “disparity” is generally used to describe differences, “inequity” suggests differences that are unjust and preventable. The presence, prevalence, and persistence of racial and ethnic health inequities in a wide range of health conditions in the US are well documented.3 The Agency for Healthcare Research and Quality regularly assesses the performance of our healthcare system and identifies strengths and weaknesses, as well as quality of healthcare and disparities in access to healthcare. The 2019 National Healthcare Quality and Disparities Report noted that in 40% of 202 quality measures, Black, American Indian, and Alaska Native patients received worse care than that received by their White counterparts. Hispanic/LatinX individuals received worse care in one-third of the quality measures.4 Multiple forces including, but not limited to institutional (through laws and policies), structural (through the ordering of society), individual (through bias and discrimination), and internalized (acceptance of stigmatized messages about abilities and self-worth) may contribute to health inequities associated with race, ethnicity, gender, income, and other social drivers. Even historical actions such as the Tuskegee study and the case of Henrietta Lacks - both of which involved individuals who participated in research without their knowledge and consent - can lead to mistrust and poor health care utilization or access to clinical trials.5 Often, these forces lead to the inequitable distribution of the “social determinants of health,” a framework that has focused on how the lived experience and poor resource access among disadvantaged individuals impact health.6 Addressing these disparities leads to health equity, which the Centers for Disease Control and Prevention refers to as “the state in which everyone has a fair and just opportunity to attain their highest level of health.”
For centuries, the relationship between race and poor health status has been attributed to genetic differences.7 As reported by many, most recently the National Academy of Sciences, “[race and ethnicity] categories are not useful proxies for biology because there is no genetic, or biological, basis for race.” The Human Genome Project determined that humans were 99.9% identical to each other at the DNA level. It found that “genetic variation overlaps across racial and ethnic groups instead of creating distinct clusters.” The notion of genetic inferiority also supports hierarchical discrimination and racial injustices. Further, it conveys the impression that disparate poor health is inevitable, thereby unburdening policy makers. As a result, increasing efforts have focused directly on racism: discrimination, marginalization, and oppression of people of color through policies, ideas, and actions. Racism accentuates health risk by restricting access to and use of effective interventions.8 Addressing these disparities requires action that is “deliberate, evidence-based, and sometimes uncomfortable.9”
Disparities in infant outcome
Among the several measures that could be used to gauge the status of infant health in the United States, infant mortality is the most used. It includes the effects of several conditions present at birth - including prematurity, congenital anomalies, complications of pregnancy and delivery, respiratory distress, and congenital infection - as well as conditions, often environmental, remote from birth—including sudden unexplained infant death, acquired infections, and accidents. It reflects short and long-term morbidity and, over time, both evolving health risks and the access and utilization of effective treatments. The sociopolitical significance of infant mortality is highlighted by the oft-quoted sentiment that societies are judged by how they treat their most vulnerable.
The reduction in infant mortality in this country represents one of the most dramatic declines in age-specific mortality ever recorded. In 1915, the first year in which US infant mortality data were available, the infant mortality rate (IMR) approached 100 deaths per 1000 live births.10 By 2023, the IMR was 5.61. Approximately two-thirds of these infants died in the neonatal period, the first 28 days of life; the US neonatal mortality rate (NMR) in 2023 was 3.65.11
Regretfully, significant racial and ethnic differences in infant mortality have persisted over this same period. In 1916, the IMR for Black infants (184.9 deaths per 1000 live births) was 87% higher than for their White counterparts. In 2023, the Black infant IMR was 10.93 deaths per 1000 live births, a dramatic improvement over 1916 but still 243% higher than the White IMR of 4.48 deaths per 1000 live births. Rates for American Indian/Alaska Native, Native Hawaiian, and Hispanic infants were also higher. The decline in infant mortality among newborns of color has therefore lagged behind the decline in White infant mortality over this period, and the same has been true for neonatal mortality12 [Figs. 1, 2]. In 2022, Black infant mortality exceeded White mortality in all five of the top five leading causes of infant death (congenital malformations, disorders related to short gestation and low birth weight, sudden infant death syndrome, unintentional injuries, and maternal complications) while Hispanic infant mortality exceeded White mortality in three of the top five.11
Two major factors contribute to disparate sub-population neonatal mortality rates: differences in risk at birth (e.g., gestational age distribution) and differences in risk-adjusted mortality once born (e.g., gestational age-specific mortality). The resulting mortality reduction strategies include either 1) reduction in preterm birth rates or provision of better care to the birth parent in hopes of improving the condition of the baby at birth, or 2) improvement in the care of the newborn. [Fig. 3] In the US, preterm birth rates (percentage born at less than 37 completed weeks of gestation) are higher for both Black (14.59%) and Hispanic (10.06%) birth individuals than White birth parents (9.44%).13 Preconception and antenatal care interventions aimed at preventing or delaying preterm birth have had frustrating and disparate effects on race and ethnic groups. A recent estimate suggested that more than two-thirds of IMR reduction was due to improvements in gestational age-specific survival that included improved survival for Black (69%) and Hispanic (86%) infants.14
Ultimately, the complete eradication of health inequity will require substantive societal efforts to address longstanding racial injustices that have resulted in substantial social and economic obstacles for minoritized communities. Whether through social determinants or through policies that have resulted in inadequate healthcare financing and resources, poor health in this population is the legacy of systemic racism and structural disadvantages. Excess preterm birth and other risk factors at birth among infants of color are sequelae of this legacy. Once born, care quality, including family support, is a critical and modifiable element in the causal pathway of outcome inequity. Strategies to ensure access to high quality neonatal intensive care for all babies should be effective, not only to improve overall infant outcomes but also to reduce racial and ethnic disparities in outcomes. A brief overview of the evolution of neonatal intensive care provides some insight into why NICUs have demonstrated more success in the former than in the latter objective.
Neonatal intensive care units: looking back to inform the future
NICUs were established in the 1960s as deliveries shifted from homes to hospitals, and hospital staff recognized the survival benefits of thermoregulation, respiratory support, hygienic practices, and physiologic monitoring for newborn infants.15 Miniaturization of adult life-sustaining technologies (e.g., ventilators, medications, and laboratory testing); understanding of unique aspects of fetal-neonatal transitional physiology; collaboration among perinatal teams of physicians, nurses, and respiratory therapists (among others); and favorable reimbursement were associated with substantial reductions in neonatal and infant mortality and rapid expansion in the number of NICUs in the United States.12,16,17 Horbar et al. described recent (1997-2021) trends in improvements in overall neonatal outcomes.18 Using outcomes of more than 400,000 very preterm (24-28 weeks’ gestation) infants cared for in more than 800 hospitals during this period, they found that the unadjusted in-hospital mortality rate declined more than 30%, from 18.1% to 12.4%, during the entire period. Except for chronic lung disease rates, which rose from 33.4% to 43.3%, rates declined for other significant morbidities including late onset infection (34.2–13.4%), necrotizing enterocolitis (10.0–6.8%), severe intraventricular hemorrhage (11.8–10.7%), severe retinopathy of prematurity (14.8–9.3%), and death or morbidity (65.4–57.6%). Despite the findings, Horbar et al. emphasized that these improvements had “slowed, stalled, or reversed” in recent years.18
Despite improved survival of critically ill newborn infants associated with NICU capacity expansion and advancements in treatments for critically ill infants, racial disparities in health outcomes persisted.11 Pragmatic adaptation of life-sustaining technologies and interventions used for adults and older children contributed to improved overall survival but were less successful in reducing racial disparities. For example, while implementation of life-sustaining interventions reduced overall neonatal mortality for infants with congenital anomalies by 10% between 2003 and 2017, and although the prevalence of most major congenital anomalies is approximately equal across racial and ethnic groups,19,20,21 the infant mortality rate for Black infants with major birth defects was more than 30% higher than the rate observed among White infants during the same period.22 Surfactant replacement therapy provides a second example of an intervention that lowered overall mortality but did not reduce racial disparities in neonatal mortality. After the U.S. Food and Drug Administration’s (FDA) approval of surfactant replacement therapy for preterm infants in 1989,23 Hamvas et al. reported a population-based, before/after FDA approval study which confirmed reduction in overall neonatal mortality with surfactant replacement therapy availability but found that this reduction was exclusively attributable to reduction in White neonatal mortality.24 Their observation was replicated in an independent cohort study25. These examples highlight the importance of rigorous, evidence-based trials for testing adaptation or implementation of new interventions for neonatal intensive care that not only examine outcomes but also are sufficiently powered to detect impact on racial disparities in outcomes. It is imperative that NICUs make explicit efforts to identify inequities and monitor outcomes with an equity lens. Fortunately, in recent years the NICU community has benefitted greatly from a scientific literature that has focused increasingly on infant health equity - both its progress and its promise.
Recent evidence: disparate outcomes within and between NICUs
Recent investigations have revealed that Black and Hispanic infants are more likely to receive care in quality-challenged hospitals and to receive poorer care within hospitals. For example, Howell and her colleagues looked at outcomes for more than 7000 very preterm infants born in New York City hospitals from 2010 to 2014 and documented substantial variation in risk-adjusted neonatal mortality and significant morbidities (bronchopulmonary dysplasia, severe necrotizing enterocolitis, stage 3 or higher retinopathy of prematurity, and grade III/IV intraventricular hemorrhage) by hospital. The hospital of birth was highly associated with the infant’s outcome. Black and Hispanic infants were more likely than White infants to be born in hospitals with the highest risk-standardized rates of morbidity and mortality. Substantial differences in outcomes were seen within hospitals, but the differences in hospital of birth explained 40% of the Black-White disparity and 30% of the Hispanic-White disparity in outcomes.26 Substantial improvements could be attained if the lowest performing hospitals performed at average. Sofaer et al. subsequently performed a qualitative study of New York City hospitals to understand the factors that differentiated high and low performing hospitals. High performing hospitals had stronger commitments from hospital leadership to diversity, quality, and equity; had better access to specialist physicians and experienced nursing staff; included nurses in developing clinical policies and protocols; and acknowledged the influence of racism and bias on racial-ethnic disparities. Opportunities for improvement in both clusters included comprehensive family engagement strategies, care standardization, and the reporting of quality data by patient sociodemographic characteristics.27
Large clinical databases provide insight into the disparities in specific clinical processes and outcomes that might explain these differences in morbidity and mortality. In a large California cohort, the California Perinatal Quality Care Collaborative (CPQCC), Profit and colleagues utilized the Baby-MONITOR tool to examine nine care processes and modifiable outcomes: antenatal steroids, hypothermia, timely eye examination, breast milk at discharge, pneumothorax, healthcare acquired infection, chronic lung disease, growth velocity, and mortality. Here again, racial/ethnic differences in outcomes and key processes were observed both within and between NICUs.28 Horbar et al. used the database of the Vermont Oxford Network (VON), a nonprofit, voluntary community of practice dedicated to improving the quality, safety, and value of care for newborns, which enrolls approximately 90% of US newborns born at 22–29 weeks’ gestation to examine factors that contributed to inequitable care. In this study, which included 700 US NICUs, he demonstrated that Black infants tended to be more concentrated (segregated) in NICUs with lower Baby-MONITOR scores. An interesting observation was that Hispanic and Asian infants were more concentrated at higher quality NICUs.29
The benefits of perinatal regionalization and risk-appropriate care- -infants with mild to complex critical illness or physiologic immaturity are born at or transferred to a facility with the personnel and resources appropriate for their needs and condition—are well documented.30 Despite these recognized benefits, infants with minoritized status in a 3-state study had reduced access to higher level and higher volume NICUs.31 Further, a recent 5-state study found that American Indian and Black individuals delivered at lower quality hospitals compared to their nearest delivery hospitals.32 Another recent examination of the CPQCC cohort described survival without major morbidity rates by race, ethnicity, and safety net hospital status. Outcomes had improved over the period 2008–2021 but had plateaued after 2018. Improvement was seen in all racial and ethnic groups, although Hispanic infants had the lowest rates of survival without major morbidity during the last three years of analysis. A significant finding was that safety net NICUs had significantly lower survival without major morbidity than their non-safety net counterparts and that Black and Hispanic infants were disproportionately hospitalized in these NICUs.33
There are substantial opportunities to reduce disparities in access to quality care and to effective interventions that will improve outcomes for all infants who require NICU care, but they may require different strategies. For example, in a systematic review of the literature, Sigurdson et al. documented the racial and ethnic disparities in quality of care for NICU infants in three health care quality measurement types: structure (nursing characteristics, risk-appropriate care settings, composite quality measures), process (breast milk use, high risk infant follow up referral, parental satisfaction, shared parent-provider decision-making, kangaroo care), and outcomes (intraventricular hemorrhage, necrotizing enterocolitis, overall morbidity and mortality).34
Advances in research and rigorous quality improvement programs have contributed to reduction in disparities in care. For example, in the VON cohort, over two periods spanning 17 years, Boghossian et al. have documented a decrease over time in racial and ethnic disparities in several care practices and outcomes for infants born at 22–29 weeks’ gestational age. In the first period, 2006–2017, compared with White infants, Black infants had a faster decline for mortality, hypothermia, necrotizing enterocolitis (NEC), and late onset sepsis (LOS), whereas Hispanic infants had a faster decline for mortality, respiratory distress syndrome, and pneumothorax. The improvements for several care practice measures and potentially modifiable outcomes reinforced the notion that quality improvement programs targeted at specific clinical practices have an important role, particularly in hospitals that serve minoritized patients.35 By the end of the second period, 2018-2022, there were no in-hospital mortality rate differences between Black and White infants, while Black newborns continued to experience higher rates of NEC and longer length of stay. Similarly, there were no mortality rate differences between Hispanic and White infants. Lower rates of respiratory complications among Black and Hispanic newborns, including chronic lung disease, compared with White newborns, have resulted in higher rates of survival without major complications for these groups.35,36 VON race/ethnicity mortality in 2021–2023 for infants 22–29 weeks is shown in Fig. 4.
Race, as well as other social determinants such as maternal educational attainment and insurance status, are associated with extreme preterm infant outcomes beyond in-hospital mortality and morbidity. A cohort study of infants born at 22–26 weeks’ gestation in NICHD Neonatal Research Network centers over a 12-year period demonstrated that among infants who survived to discharge, social determinants were also associated with higher rates of readmission, neurodevelopmental impairment, and post-discharge death.36 Referral to high-risk infant follow-up programs, recommended to help mitigate risks associated with extreme preterm delivery and improve long-term health and development, is highly variable. A large cohort study of infants discharged from 58 US hospitals found that fewer than half were seen in these programs with notable disparities in the participation of Black infants both within and between hospitals.37 These findings were like those of a population-based California cohort of very low birth weight infants where race and other sociodemographic factors were associated with non-participation in NICU follow up care.38 In another study examining resource and service use of the most vulnerable of these infants (born at 22-25 weeks’ gestation), lower resource utilization was associated with maternal and sociodemographic factors.39
To summarize, despite substantial improvements in care and outcomes, racial inequities both between and within NICUs remain. Minoritized infants are more concentrated in hospitals with poorer adjusted outcomes, including mortality and severe morbidity. Differentiating factors in these lower performing hospitals include structural, leadership, and cultural factors - all of which may be affected by limited resources. These infants also experience differences in care practices and modifiable outcomes within NICUs with disparate structural, process, and outcome quality measures. Despite these challenges, in recent years, several racially and ethnically disparate NICU care practices and outcomes have improved. Persistence of racial disparities in post-discharge outcomes, including neurodevelopmental impairment and post-discharge death, is likely affected by both disparate referral practices and deeply embedded social conditions.
Strategies to address racial disparities in NICU outcomes
Addressing challenges in inequitable racial and ethnic outcomes affected by differential care quality, and/or by access to or utilization of effective interventions requires different strategies. Although NICUs have limited opportunities to address the laws, policies, and history that disadvantage minoritized populations, they do have opportunities to mitigate the effects of persisting social conditions that differentially affect patients and families from these communities through strategies ranging from the implementation of programs supporting lower performing NICUs to processes facilitating intentional recruitment into follow up programs.
Strategies to improve NICU health equity are similar to those that improve clinical care and outcomes. Care innovations must continue to be aggressively pursued and studied through rigorous examination and trials sufficiently powered to detect their real or potential impact on racial disparities. For example, although not rigorously tested, improving continuity of support and communication between pregnancy and NICU providers who are caring for all high-risk pregnant people might improve infant outcomes through earlier identification of risk factors for the infant. Effective approaches to NICU clinical management should be standardized through evidence-based and regularly updated medical practice guidelines and policies that guide nursing and ancillary care team practices. Patient safety and quality improvement programs must assure that these practices are applied consistently to all NICU patients.
To address the variability in NICU care quality and better assure risk-appropriate care, challenges that are particularly prevalent in disadvantaged communities, the American Academy of Pediatrics (AAP) has provided helpful guidance with the policy statement, “Standards for Levels of Neonatal Care: II, III, and IV”.40 Despite universal state regulation of health care facilities, wide variation in the requirements for levels of neonatal care and in adherence to these specifications exists. The Standards were developed in response to the need to ensure high quality and equitable care. They address expectations for institutional commitment, scope of services, personnel, ancillary services, safety and quality programming, patient and family care resources and practices, and equipment required for each level of neonatal care [Table 1]. The Standards provide objective expectations and can be utilized by hospitals, states, and third-party evaluators (e.g., the AAP NICU Verification Program, third-party payers, and reputational surveys) to ensure that NICUs have the resources, personnel, assets, and processes to provide high quality, risk-appropriate care. Elevating quality in poorer-performing hospitals targets between-NICU variation. Within NICU differences largely reflect differences in use of evidence-based practices. Adhering to quality and performance standards--including structured, equity-focused, quality improvement and care standardization using evidence-based guidelines and policies—also targets within NICU variation. In addition to these technical (clinical) opportunities to improve care, within NICU potential improvements include essential relational (engaging and supporting families) care processes to mitigate stress, promote trust, and encourage care and feeding, as well as address the adverse interactions experienced by minoritized families.41 Family-centered care core components are included in the general program requirements of the national standards. Potential processes to improve family engagement might include ensuring linguistically concordant and culturally sensitive communication; identifying and addressing social determinants of health; and educating staff on topics such as infant health equity, implicit bias, and antiracism. Many NICUs have made more intentional efforts to improve staff diversity, responding to a body of research that has highlighted the benefits of minoritized patient-physician racial concordance on outcomes of care, including the NICU.42
Besides implementation of the AAP’s Standards, several strategies to reduce racial disparities in NICU-based outcomes have been suggested and supported through health equity programs of regional and national quality collaboratives. Building upon the work of Richard Rothstein (The Color of Law), Beck et al. describe the contributions of racism, segregation, and inequality to health outcome disparities across the life course43 (Table 2). Here, they discuss the opportunity to improve on the paradigm of NICU follow up, which has traditionally primarily focused on managing medical conditions and assessing neurodevelopment after NICU discharge. Rather, they propose the concept of “follow through,” an approach where health professionals assume greater responsibility for long term outcomes through comprehensive family engagement and improved coordination with community services. They specifically highlight the importance of promoting a culture of equity; identifying and mitigating family social risks; improving transitions to home and beyond; developing robust, equity-focused, quality improvement programs; and advocating for social justice at the local, state, and national levels. A collection of VON Potentially Better Practices (PBPs) to support these efforts is included and further described in a subsequent perspective.44 A recent survey demonstrated the ability of a wide range of NICUs to adopt several of the follow through PBPs.45
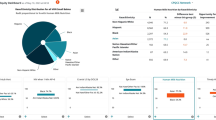
Montoya-Williams et al. cite concrete ways in which NICU-based health care professionals can contribute to antiracism and health equity8 (Fig. 5). Noting that the NICU is an ideal setting for implementation of antiracism, they suggest using several approaches with full partnership from Black and other minoritized families to address specific racial disparities, and incorporating antiracism into NICU-based research, academic and healthcare administration, and community engagement. Collaborating with families entails providing culturally and linguistically appropriate services. Specifically, they suggest integrating antiracism into medical education, developing programs that intentionally focus on improving access of Black women to prenatal care with maternal-fetal medicine specialists, improving access of Black families to NICU follow-up care and support, and instituting clinical, real-time dashboards that track delivery and outcomes by race, ethnicity, and preferred language of an infant’s family.
NICU-based strategies for improving infant outcomes and reducing racial disparities8.
Several professional organizations in pediatrics and obstetrics have increasingly focused on health equity and have developed knowledge bases and tools to support this work. These include the American Academy of Pediatrics, the Academic Pediatric Association, the American College of Obstetrics and Gynecology, and the Society for Maternal-Fetal Medicine. The American Pediatric Society informs equity-focused policies, advocacy, and academic research by offering scholarly sessions at the Pediatric Academic Society meeting and other platforms. The mission of the American Board of Pediatrics is to certify pediatricians who meet standards of excellence and are committed to continuous learning and improvement. Although not a membership organization, it has supported health equity through workforce data support, knowledge and skill assessment content, and in its wide range of health care improvement offerings. A younger organization, the Neonatal Justice Collaborative, which utilizes action-oriented research, advocacy, medical education, and quality improvement to advance health equity, antiracism, and social justice, is one of the most active in this space. The focus of other organizations can be leveraged to gain support for equity work to the benefit of the NICU and other hospital services. The Joint Commission, an agency tasked with evaluating the safety and quality of health care organizations, issued new requirements to reduce health care disparities in 2023. These requirements focus on leadership, health-related social needs assessment, and sociodemographic quality and safety. Even reputational surveys, such as the US News and World Report rankings, have begun to compile rankings of hospitals serving disadvantaged communities.
Finally, all equity strategies require sound data to support quality and performance improvement efforts and accountability to act on the data results. In addition to internal reporting, race-specific NICU outcomes can be incorporated into hospital-wide quality improvement metrics, monitored regularly, and shared with families, staff, and providers. Improvement in these metrics might also be considered in the evaluation of hospital leadership performance. In addition to data acquired internally, data from local, regional, and national sources help to raise awareness, identify disparate outcomes and modifiable targets, provide benchmarks, and drive interventions. The field of health equity science provides this focus, and “builds evidence to guide programs, surveillance, policy, communications, and future scientific study focused on eliminating inequities.46” It is foundational for explorations of racial, ethnic and other social inequities such as rurality, where health literacy, poor access to primary and specialty care, and increased travel distances to care facilities may influence access and utilization.47
Conclusion
There are many opportunities to improve health equity in NICUs. Unit-based physician and patient care services leadership share responsibility with hospitals’ boards of directors, accrediting and reputational organizations, professional organizations, and third-party payers for ensuring that equity-focused PBPs43 (Table 2) are undertaken, promoted, measured, monitored, and advanced in their units. Fundamental to improving health equity nationally is elevating care quality in poorly performing units and ensuring that safe, effective care practices are applied consistently to all patients and families. Both the assurance of risk-appropriate care in regionalized systems and unit compliance with comprehensive standards are essential. NICU care must be supported by adherence to evidence-based guidelines; robust, equity-focused quality improvement; comprehensive family engagement, including culturally and linguistically appropriate services; follow through practices, including identifying and mitigating health-related social needs; and coordination with community services for transition to home and beyond. Sufficient resources are required to ensure high level NICU care. Hospital and network administration and governance, as well as state and federal health entities, share accountability for infant health equity.
In the face of threats to reduce or eliminate health insurance, severely constrain biomedical and health services research funding, and limit public health oversight, all of us must redouble our efforts to ensure that all NICU patients and families receive the best care that we have available to provide the sickest and most vulnerable patients among us.
“There can be no keener revelation of a society’s soul than the way in which it treats its children.” Nelson Mandela –
References
Bailey, Z. D. et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet 389, 1453–1463 (2017).
Jones, C. P. Levels of racism: a theoretic framework and a gardener’s tale. Am. J. Public Health 90, 1212–1215 (2000).
Collaborators, G. U. H. D. Cause-specific mortality by county, race, and ethnicity in the USA, 2000-19: a systematic analysis of health disparities. Lancet 402, 1065–1082 (2023).
Bonnett, D. 2019 National Healthcare Quality and Disparities Report, https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html (2019).
Center, P. R. Trust and Mistrust in Americans’ View of Scientific Experts. (2019).
Yearby, R. Structural racism and health disparities: reconfiguring the social determinants of health framework to include the root cause. J. Law Med. Ethics 48, 518–526 (2020).
Borrell, L. N. et al. Race and genetic ancestry in medicine–a time for reckoning with racism. N. Engl. J. Med. 384, 474–480 (2021).
Montoya-Williams, D., Fraiman, Y. S., Pena, M. M., Burris, H. H. & Pursley, D. M. Antiracism in the field of neonatology: a foundation and concrete approaches. Neoreviews 23, e1–e12 (2022).
Wang, S. X. Y. & Chi, K. Answering the call–sustaining equity efforts in the face of regression. N. Engl. J. Med. 392, 944–945 (2025).
Families, C. O. P. A. E.-O.-L. C. F. C. A. T. When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families (Institute of Medicine, Washington, 2003).
Ely, D. M. & Driscoll, A. K. In Vital Statistics Rapid Release Reports (2024).
Singh, G. K. & Yu, S. M. Infant mortality in the United States, 1915-2017: large social inequalities have persisted for over a century. Int J. MCH AIDS 8, 19–31 (2019).
Martin, J. A., Hamilton, B. E. & Osterman, M. J. K. Births in the United States, 2022. NCHS Data Brief, 1-8 (2023).
Callaghan, W. M., MacDorman, M. F., Shapiro-Mendoza, C. K. & Barfield, W. D. Explaining the recent decrease in US infant mortality rate, 2007-2013. Am. J. Obstet. Gynecol. 216, e71-73–e71-78 (2017).
Kingsmore, S. F. & Cole, F. S. The role of genome sequencing in neonatal intensive care units. Annu Rev. Genomics Hum. Genet 23, 427–448 (2022).
Pineda, R. et al. Nicus in the US: levels of acuity, number of beds, and relationships to population factors. J. Perinatol. 43, 796–805 (2023).
Davis, R., Stuchlik, P. M. & Goodman, D. C. The relationship between regional growth in neonatal intensive care capacity and perinatal risk. Med. Care 61, 729–736 (2023).
Horbar, J. D. et al. Trends in mortality and morbidities for infants born 24 to 28 weeks in the US: 1997-2021. Pediatrics 153 (2024).
Egbe, A., Lee, S., Ho, D. & Uppu, S. Effect of race on the prevalence of congenital malformations among newborns in the United States. Ethn. Dis. 25, 226–231 (2015).
Egbe, A. et al. Congenital malformations in the newborn population: a population study and analysis of the effect of sex and prematurity. Pediatr. Neonatol. 56, 25–30 (2015).
Gilboa, S. M. et al. Congenital heart defects in the united states: estimating the magnitude of the affected population in 2010. Circulation 134, 101–109 (2016).
Almli, L. M. et al. Infant mortality attributable to birth defects–United States, 2003-2017. MMWR Morb. Mortal. Wkly Rep. 69, 25–29 (2020).
Raj, J. U., Bland, R. D., Bhattacharya, J., Rabinovitch, M. & Matthay, M. A. Life-saving effect of pulmonary surfactant in premature babies. J. Clin. Investig. 134 (2024).
Hamvas, A. et al. The influence of the wider use of surfactant therapy on neonatal mortality among blacks and whites. N. Engl. J. Med. 334, 1635–1640 (1996).
Frisbie, W. P., Song, S. E., Powers, D. A. & Street, J. A. The increasing racial disparity in infant mortality: respiratory distress syndrome and other causes. Demography 41, 773–800 (2004).
Howell, E. A. et al. Differences in morbidity and mortality rates in black, white, and hispanic very preterm infants among New York City Hospitals. JAMA Pediatr. 172, 269–277 (2018).
Sofaer, S. et al. Characteristics of high versus low-performing hospitals for very preterm infant morbidity and mortality. J. Pediatr. X 10, 100094 (2023).
Profit, J. et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics 140 (2017).
Horbar, J. D. et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 173, 455–461 (2019).
Lasswell, S. M., Barfield, W. D., Rochat, R. W. & Blackmon, L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA 304, 992–1000 (2010).
Yannekis, G., Passarella, M. & Lorch, S. Differential effects of delivery hospital on mortality and morbidity in minority premature and low birth weight neonates. J. Perinatol. 40, 404–411 (2020).
Boghossian, N. S. et al. Racial and ethnic inequalities in actual vs nearest delivery hospitals. JAMA Netw. Open 8, e251404 (2025).
Liu, J. et al. Disparities in survival without major morbidity among very low birth weight infants in California. Pediatrics 154 (2024).
Sigurdson, K., Morton, C., Mitchell, B. & Profit, J. Disparities in NICU quality of care: a qualitative study of family and clinician accounts. J. Perinatol. 38, 600–607 (2018).
Boghossian, N. S., Geraci, M., Edwards, E. M. & Horbar, J. D. Racial and ethnic differences in outcomes of neonates born at less than 30 weeks’ gestation, 2018-2022. JAMA Netw. Open 7, e2451707 (2024).
Brumbaugh, J. E. et al. Early-life outcomes in relation to social determinants of health for children born extremely preterm. J. Pediatr. 259, 113443 (2023).
Fraiman, Y. S. et al. Racial inequity in high-risk infant follow-up among extremely low birth weight infants. Pediatrics 151, e2022057865 (2023).
Hintz, S. R. et al. Factors associated with successful first high-risk infant clinic visit for very low birth weight infants in California. J. Pediatr. 210, 91–98.e91 (2019).
Pai, V. V. et al. Resource and service use after discharge among infants 22-25 weeks estimated gestational age at the first high-risk infant follow-up visit in California. J. Pediatr. 274, 114172 (2024).
Stark, A. R. et al. Standards for levels of neonatal care: II, III, and IV. Pediatrics 151, e2023061957 (2023).
Ravi, D., Iacob, A. & Profit, J. Unequal care: racial/ethnic disparities in neonatal intensive care delivery. Semin Perinatol. 45, 151411 (2021).
Greenwood, B. N., Hardeman, R. R., Huang, L. & Sojourner, A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc. Natl. Acad. Sci. USA 117, 21194–21200 (2020).
Beck, A. F. et al. The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatr. Res 87, 227–234 (2020).
Horbar, J. D., Edwards, E. M. & Ogbolu, Y. Our responsibility to follow through for NICU infants and their families. Pediatrics 146, e20200360 (2020).
Edwards, E. M., Ehret, D. E. Y. & Horbar, J. D. Potentially better practices for follow through in neonatal intensive care units. Pediatrics 154, e2023065530 (2024).
National Center for Chronic Disease Prevntion and Health Promotion (NCCDPHP), C. f. D. C. a. P. Health Equity Science: Research and Evaluation, https://www.cdc.gov/health-equity-chronic-disease/hcp/health-equity-science/index.html (2024).
Khan, S. S. & Yancy, C. W. Rural America-Expanding the Lens of Health Disparities: Endorsing the Need for Health Equity Research. JAMA Cardiol (2025).
Acknowledgements
The authors wish to thank NICU providers, staff, and families for their ongoing commitment to improving outcomes for all high-risk infants. Unpublished VON data used with permission.
Funding
Pursley was supported by the Department of Pediatrics, Harvard Medical School, and Department of Neonatology, Beth Israel Deaconess Medical Center, Boston, MA.
Author information
Authors and Affiliations
Contributions
Pursley and Cole both contributed to conception and design of this manuscript, drafting and revising the review critically for important intellectual content, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
Cole has no potential/perceived conflicts of interest to report. Pursley is a member of the Board of Directors of Vermont-Oxford Network and the chair of the Advisory Board of the American Academy of Pediatrics NICU Verification Program.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pursley, D.M., Cole, F.S. Improving infant health equity: what have we learned, what do we do. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04589-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04589-7