Abstract
Background
Traditional nomograms can inform the presence of extraprostatic extension (EPE) but not laterality, which remains important for surgical planning, and have not fully incorporated multiparametric MRI data. We evaluated predictors of side-specific EPE on surgical pathology including MRI characteristics and developed side-specific EPE risk calculators.
Methods
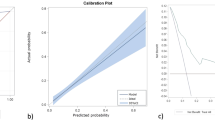
This was a retrospective cohort of patients evaluated with mpMRI prior to radical prostatectomy (RP) in our eleven hospital healthcare system from July 2018-November 2022. The dominant side was defined pre-operatively using a tiered system based on laterality of highest biopsy Gleason Grade Group (GG), highest PIRADS lesion, number of lesions, and cancer volume. Univariable and multivariable logistic regression were performed for overall EPE, dominant side EPE, and non-dominant side EPE. Internal validation with leave one out and calibration curves were completed.
Results
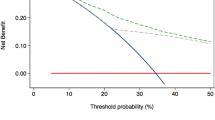
EPE was identified in 53% (317/601) of patients at RP. Side-specific factors (PIRADS, GG, abutment) were only associated with EPE on their respective side. Final variables in the model associated with EPE on the dominant and non-dominant sides included age, log PSA density (PSAD), side-specific PIRADS 5, side-specific GG3–5, and percentage positivity of systematic cores. AUCs for dominant and non-dominant side EPE were 0.77 (95% CI 0.73—0.80) and 0.79 (95% CI 0.74–0.84), respectively. MRI-identified abutment and prostate health index (PHI) did not improve model discrimination. Risk calculators available online at https://rossnm1.shinyapps.io/PredictionOfEPELaterality/.
Conclusions
PSA, side-specific PIRADS, side-specific GG, and percentage positivity of systematic cores were associated with side-specific EPE at RP and incorporated into a risk calculator to assist in surgical planning and nerve-sparing decisions at time of RP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data are available for bona fide researchers who request it from the authors.
Code availability
Code can be provided by contacting the corresponding author by reasonable request.
References
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378:1767–77.
Padhani AR, Petralia G, Sanguedolce F. Magnetic resonance imaging before prostate biopsy: time to talk. Eur Urol. 2016;69:1–3.
Siddiqui MR, Ansbro B, Shah PV, Aguiar JA, Li EV, Rich JM, et al. Real-world use of MRI for risk stratification prior to prostate biopsy. Prostate Cancer Prostatic Dis. 2023;26:353–9.
Jeong BC, Chalfin HJ, Lee SB, Feng Z, Epstein JI, Trock BJ, et al. The relationship between the extent of extraprostatic extension and survival following radical prostatectomy. Eur Urol. 2015;67:342–6.
Tosoian JJ, Chappidi M, Feng Z, Humphreys EB, Han M, Pavlovich CP, et al. Prediction of pathological stage based on clinical stage, serum prostate-specific antigen, and biopsy Gleason score: Partin Tables in the contemporary era. BJU Int. 2017;119:676–83.
Kattan MW, Eastham JA, Stapleton AM, Wheeler TM, Scardino PT. A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst. 1998;90:766–71.
Cooperberg MR, Freedland SJ, Pasta DJ, Elkin EP, Presti JC Jr, Amling CL, et al. Multiinstitutional validation of the UCSF cancer of the prostate risk assessment for prediction of recurrence after radical prostatectomy. Cancer. 2006;107:2384–91.
de Rooij M, Hamoen EH, Witjes JA, Barentsz JO, Rovers MM. Accuracy of magnetic resonance imaging for local staging of prostate cancer: a diagnostic meta-analysis. Eur Urol. 2016;70:233–45.
Soeterik TFW, van Melick HHE, Dijksman LM, Küsters-Vandevelde H, Stomps S, Schoots IG, et al. Development and external validation of a novel nomogram to predict side-specific extraprostatic extension in patients with prostate cancer undergoing radical prostatectomy. Eur Urol Oncol. 2022;5:328–37.
Martini A, Gupta A, Lewis SC. Development and internal validation of a side-specific, multparametric magnetic resonance imaging-based nomogram for the prediction of extracapsular extension of prostate cancer. BJU Int. 2018;122:1025–33.
Veerman H, Heymans MW, van der Poel HG. External validation of a prediction model for side-specific extraprostatic extension of prostate cancer at robot-assisted radical prostatectomy. Eur Urol Open Sci. 2022;37:50–2.
Godtman RA, Kollberg KS, Pihl CG, Månsson M, Hugosson J. The association between age, prostate cancer risk, and higher gleason score in a long-term screening program: results from the göteborg-1 prostate cancer screening trial. Eur Urol. 2022;82:311–7.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Eur Urol. 2015;67:1142–51.
Diamand R, Ploussard G, Roumiguié M, Oderda M, Benamran D, Fiard G, et al. External validation of a multiparametric magnetic resonance imaging-based nomogram for the prediction of extracapsular extension and seminal vesicle invasion in prostate cancer patients undergoing radical prostatectomy. Eur Urol. 2021;79:180–5.
Stephenson AJ, Scardino PT, Eastham JA, Bianco FJ Jr, Dotan ZA, Fearn PA, et al. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Natl Cancer Inst. 2006;98:715–7.
Freifeld Y, Diaz de Leon A, Xi Y. Diagnostic performance of prospectively assigned likert scale scores to determine extraprostatic extension and seminal vesicle invasion with multiparametric MRI of the prostate. AJR Am J Roentgenol. 2019;212:576–81.
Reisæter LA, Halvorsen OJ, Beisland C. Assessing extraprostatic extension with multiparametric MRI of the prostate: mehralivand extraprostatic extension grade or extraprostatic extension likert scale? Radio Imaging Cancer. 2020;2:e190071.
Mehralivand S, Shih JH, Harmon S. A grading system for the assessment of risk of extraprostatic extension of prostate cancer at multiparametric MRI. Radiology. 2019;290:709–19.
Valentin B, Schimmoller L, Ullrich T. Magnetic resonance imaging improves the prediction of tumor stage in localized prostate cancer. Abdom Radio. 2021;46:2751–9.
Bakir B, Onay A, Vural M. Can extraprostatic extension be predicted by tumor-capsule contact length in prostate cancer? relationship with international society of urological pathology grade groups. AJR Am J Roentgenol. 2020;214:588–96.
van den Berg I, Soeterik TFW, van der Hoeven E, Claassen B, Brink WM, Baas DJH, et al. The development and external validation of artificial intelligence-driven MRI-based models to improve prediction of lesion-specific extraprostatic extension in patients with prostate cancer. Cancers (Basel). 2023;15:5452.
Westphalen AC, McCulloch CE, Anaokar JM, Arora S, Barashi NS, Barentsz JO, et al. Variability of the positive predictive value of PI-RADS for prostate MRI across 26 centers: experience of the society of abdominal radiology prostate cancer disease-focused panel. Radiology. 2020;296:76–84.
Moroianu SL, Bhattacharya I, Seetharaman A. Computation detection of extraprostatic extension of prostate cancer on multiparametric MRI using deep learning. Cancers (Basel). 2022;14:2821.
Funding
HDP is supported by the Prostate Cancer Foundation Young Investigator Award.
Author information
Authors and Affiliations
Contributions
EVL contributed with conceptualization, methodology, formal analysis, investigation, data curation, writing of original draft and editing, and visualization. SK assisted with methodology, formal analysis, investigation, resources, visualization, and reviewing and editing of manuscript. JAA assisted with investigation, writing of original draft, and review and editing of the manuscript. MRS assisted with data curation and review and editing of manuscript. ZS contributed to investigation and review of manuscript. CN contributed to resources, data acquisition, and review and editing of manuscript. EMS provided conceptualization, review and editing of manuscript and supervision. AER contributed with conceptualization, review and editing of manuscript, supervision, project administration, and funding acquisition. HDP contributed with conceptualization, review and editing of manuscript, supervision, project administration, and funding acquisition.
Corresponding author
Ethics declarations
Competing interests
AER is engaged in consulting with American Society of Clinical Oncology (ASCO), Astellas, Bayer HealthCare Pharmaceuticals, Blue Earth Diagnostics, Janssen Biotech, Lantheus Medical Imaging, Myovant Sciences, NCCN, Pfizer, Tempus Health, and Veracyte. EMS is engaged in consulting with Astellas, Lantheus Medical Imaging, Pfizer. The other contributing authors have no conflicts of interest to declare.
Ethics approval and consent to participate
The study was reviewed under IRB STU00214996 issued by Northwestern University. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, E.V., Kumar, S., Aguiar, J.A. et al. Prostate MRI and clinicopathologic risk calculator to predict laterality of extraprostatic extension at radical prostatectomy. Prostate Cancer Prostatic Dis 28, 859–864 (2025). https://doi.org/10.1038/s41391-024-00928-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41391-024-00928-7
This article is cited by
-
Re: Prostate MRI and clinicopathologic risk calculator to predict laterality of extraprostatic extension at radical prostatectomy
Prostate Cancer and Prostatic Diseases (2025)
-
Integrating clinical and technological perspectives to enhance predictive modeling in prostate cancer surgery
Prostate Cancer and Prostatic Diseases (2025)