Abstract
Introduction
Standard surgical options for Benign Prostatic Hyperplasia [BPH], despite their excellent functional outcomes, are associated with multiple side effects and require general/spinal anesthesia and hospitalization. In this scenario, Transperineal Laser Ablation of the Prostate [TPLA] emerged as an ultra-minimally invasive ejaculation-sparing procedure, showing promising functional results, with a good safety profile. This systematic review aimed to provide an overview of the current role of TPLA in clinical practice, focusing on operative setting, safety, and efficacy.
Evidence acquisition
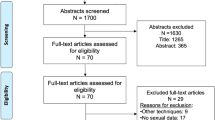
Literature search was performed on June 12th, 2024 using PubMed, Embase, and Cochrane Central databases, following the EAU Guidelines Office and the PRISMA statement recommendations. All studies reporting outcomes after TPLA procedures were included.
Evidence synthesis
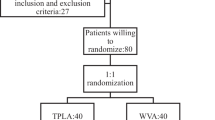
Seventeen studies were included in this systematic review, of which 2 RCTs compared TPLA with TURP, 12 prospective and 3 retrospective non-randomized studies (of which 1 comparing TPLA and Prostatic Artery Embolization [PAE]). All procedures were performed using the same EchoLaserTM system (SoracteLiteTM) (Elesta s.r.l., Calenzano (FI), Italy), however great heterogeneity exists considering inclusion criteria, peri- and post-operative management. Mainly low-grade complications (Clavien-Dindo [CD] Grade ≤ II) were reported, while no major adverse events (CD grade > III) occurred. In all studies TPLA led to a great improvement in urinary function, up to 5 years after the procedure, while not significantly impacting erectile and ejaculatory functions.
Conclusions
TPLA showed promising results both in the short- and mid-term, improving urinary function while preserving sexual function and keeping a good safety profile. Since the evidence available is still limited, larger prospective comparative studies are warranted to confirm the efficacy of TPLA and to adequately compare it to standard endoscopic techniques and other minimally invasive surgical treatments.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Sebastianelli A, Gacci M. Current status of the relationship between metabolic syndrome and lower urinary tract symptoms. Eur Urol Focus. 2018;4:25–7.
Gacci M, Sebastianelli A, Salvi M, De Nunzio C, Vignozzi L, Corona G, et al. Benign prostatic enlargement can be influenced by metabolic profile: results of a multicenter prospective study. BMC Urol. 2017;17:22.
Cornu JN, Gacci M, Hashim H, Herrmann TRW, Malde S, Netsch C, et al. EAU guidelines on non-neurogenic male lower urinary tract symptoms (LUTS). 2024;67:1099–109.
Gacci M, Sebastianelli A, Spatafora P, Corona G, Serni S, De Ridder D, et al. Best practice in the management of storage symptoms in male lower urinary tract symptoms: a review of the evidence base. Ther Adv Urol. 2018;10:79–92.
Gandhi J, Weissbart SJ, Smith NL, Kaplan SA, Dagur G, Zumbo A, et al. The impact and management of sexual dysfunction secondary to pharmacological therapy of benign prostatic hyperplasia. Transl Androl Urol. 2017;6:295–304.
La Vignera S, Aversa A, Cannarella R, Condorelli RA, Duca Y, Russo GI, et al. Pharmacological treatment of lower urinary tract symptoms in benign prostatic hyperplasia: consequences on sexual function and possible endocrine effects. Expert Opin Pharmacother. 2021;22:179–89.
Gacci M, Ficarra V, Sebastianelli A, Corona G, Serni S, Shariat SF, et al. Impact of medical treatments for male lower urinary tract symptoms due to benign prostatic hyperplasia on ejaculatory function: a systematic review and meta-analysis. J Sex Med. 2014;11:1554–66.
Ottaiano N, Shelton T, Sanekommu G, Benson CR. Surgical complications in the management of benign prostatic hyperplasia treatment. Curr Urol Rep. 2022;23:83–92.
Porto JG, Arbelaez MCS, Blachman-Braun R, Bhatia A, Bhatia S, Satyanarayana R, et al. Complications associated with minimally invasive surgical therapies (MIST) for surgical management of benign prostatic hyperplasia: a Manufacturer and User Facility Device Experience (MAUDE) database review. World J Urol. 2023;41:1975–82.
Cornu JN, Zantek P, Burtt G, Martin C, Martin A, Springate C, et al. Minimally invasive treatments for benign prostatic obstruction: a systematic review and network meta-analysis. Eur Urol. 2023;83:534–47.
Gemma L, Pecoraro A, Sebastianelli A, Spatafora P, Sessa F, Nicoletti R, et al. Impact of minimally invasive surgical procedures for Male Lower Urinary Tract Symptoms due to benign prostatic hyperplasia on ejaculatory function: a systematic review. Prostate Cancer Prostatic Dis. 2024;27:404–21.
Busetto GM, Lombardo R, De Nunzio C, Santoro G, Tocci E, Schiavone N, et al. Ejaculation sparing of classic and minimally invasive surgical treatments of LUTS/BPH. Prostate Cancer Prostatic Dis. 2025;28:37–44.
Elterman DS, Zorn KC, Chughtai B, Bhojani N. Is it time to offer True Minimally Invasive Treatments (TMIST) for BPH? - A review of office-based therapies and introduction of a new technology category. Can J Urol. 2021;28:10580–3.
Checcucci E, Veccia A, De Cillis S, Piramide F, Volpi G, Amparore D, et al. New ultra-minimally invasive surgical treatment for benign prostatic hyperplasia: a systematic review and analysis of comparative outcomes. Eur Urol Open Sci. 2021;33:28–41.
Sessa F, Bisegna C, Polverino P, Gacci M, Siena G, Cocci A, et al. Transperineal laser ablation of the prostate (TPLA) for selected patients with lower urinary tract symptoms due to benign prostatic obstruction: a step-by-step guide. Urol Video J 2022;15:100167.
Sessa F, Polverino P, Siena G, Bisegna C, Lo Re M, Spatafora P, et al. Transperineal laser ablation of the prostate (TPLA) for lower urinary tract symptoms due to benign prostatic obstruction. J Clin Med. 2023;12:793.
Tzelves L, Nagasubramanian S, Pinitas A, Juliebø-Jones P, Madaan S, Sienna G, et al. Transperineal laser ablation as a new minimally invasive surgical therapy for benign prostatic hyperplasia: a systematic review of existing literature. Ther Adv Urol. 2023;15:17562872231198634.
Tafuri A, Panunzio A, De Carlo F, Luperto E, Di Cosmo F, Cavaliere A, et al. Transperineal laser ablation for benign prostatic enlargement: a systematic review and pooled analysis of pilot studies. J Clin Med. 2023;12:1860.
Knoll T, Omar MI, Maclennan S, Hernández V, Canfield S, Yuan Y, et al. Key steps in conducting systematic reviews for underpinning clinical practice guidelines: methodology of the European Association of Urology. Eur Urol. 2018;73:290–300.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Cai HJ, Fang JH, Kong FL, Xu CK, Chen CH, Wang W, et al. Ultrasound-guided transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a new minimally invasive interventional therapy. Acta radiol. 2022;63:553–8.
Patelli G, Ranieri A, Paganelli A, Mauri G, Pacella CM. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. Cardiovasc Intervent Radiol. 2017;40:1440–6.
Pacella CM, Patelli G, Iapicca G, Manenti G, Perretta T, Ryan CP, et al. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. Prostate Cancer Prostatic Dis. 2020;23:356–63.
de Rienzo G, Lorusso A, Minafra P, Zingarelli M, Papapicco G, Lucarelli G, et al. Transperineal interstitial laser ablation of the prostate, a novel option for minimally invasive treatment of benign prostatic obstruction. Eur Urol. 2021;80:95–103.
Frego N, Saita A, Casale P, Diana P, Contieri R, Avolio PP, et al. Feasibility, safety, and efficacy of ultrasound-guided transperineal laser ablation for the treatment of benign prostatic hyperplasia: a single institutional experience. World J Urol. 2021;39:3867–73.
Manenti G, Perretta T, Calcagni A, Ferrari D, Ryan CP, Fraioli F, et al. 3-T MRI and clinical validation of ultrasound-guided transperineal laser ablation of benign prostatic hyperplasia. Eur Radiol Exp. 2021;5:41.
Polverino P, Lore M, Saladino M, Pecoraro A, Moscardi L, Rivetti A, et al. Could transperineal interstitial laser ablation of the prostate be the right option for highly comorbid patients with lower urinary tract symptoms due to benign prostatic obstruction? A preliminary single-center experience focusing on functional and safety outcomes. Minerva Urol Nephrol. 2023;76:646–9.
Bertolo R, Iacovelli V, Cipriani C, Carilli M, Vittori M, Antonucci M, et al. Ejaculatory function following transperineal laser ablation vs <scp>TURP < /scp> for benign prostatic obstruction: a randomized trial. BJU Int. 2023;132:100–8.
Canat HL, Gurbuz C, Bozkurt M. Transurethral resection of the prostate (TURP) versus transperineal laser ablation (TPLA) due to benign prostatic hyperplasia (BPH): prospective and comparative study. Int Urol Nephrol. 2023;55:2747–52.
Destefanis P, Sibona M, Vitiello F, Vercelli E, Micai L, Montefusco G, et al. Trans - Perineal laser ablation of the prostate in high surgical risk patients affected by severe lower urinary tract symptoms related to benign prostatic obstruction. Prostate Cancer Prostatic Dis. 2023;27:693–9.
Laganà A, Di Lascio G, Di Blasi A, Licari LC, Tufano A, Flammia RS, et al. Ultrasound-guided SoracteLiteTM transperineal laser ablation (TPLA) of the prostate for the treatment of symptomatic benign prostatic hyperplasia (BPH): a prospective single-center experience. World J Urol. 2023;41:1157–62.
Minafra P, Derienzo G, Gerbasi S, Cindolo L, Battaglia M, Ditonno P. Three years outcomes of transperineal laser ablation of the prostate. Minerva Urol Nephrol. 2023;75:471–8.
Patelli G, Altieri VM, Ierardi AM, Carnevale A, Chizzoli E, Baronchelli F, et al. Transperineal laser ablation of the prostate for symptomatic benign prostatic hyperplasia: long-term follow-up in 40 patients. J Vas Interv Radiol. 2024;35:1187–93.
van Kollenburg R, van Riel L, Bloemen P, de Reijke T, Beerlage H, de Bruin D, et al. Transperineal laser ablation as treatment for benign prostatic obstruction: safety, feasibility and functional outcomes—A pilot study. BJUI Compass. 2024;5:52–9.
Lo Re M, Polverino P, Rivetti A, Pecoraro A, Saladino M, Pezzoli M, et al. Transperineal laser ablation (TPLA) of the prostate for benign prostatic obstruction: the first 100 patients cohort of a prospective, single-center study. World J Urol. 2024;42:402.
Bianco FJ, Luna E, Lopez-Prieto A, González P, Gheiler EL, Kaufman AM, et al. Office-based transperineal laser ablation for benign prostatic hyperplasia under local anesthesia: 2-year results from a dose range confirmatory trial. JU Open Plus. 2024;2:e00008.
Cai H, Zhu C, Fang J. Ultrasound-guided perineal laser ablation versus prostatic arterial embolization for benign prostatic hyperplasia: two similar short-term efficacies. Acta radiol. 2023;64:2033–9.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The clavien-dindo classification of surgical complications. Ann Surg. 2009;250:187–96.
Baerlocher MO, Nikolic B, Sze DY. Adverse event classification: clarification and validation of the society of interventional radiology specialty–specific system. J Vas Interv Radiol. 2023;34:1–3.
Cocci A, Pezzoli M, Bianco F, Blefari F, Bove P, Cornud F, et al. Transperineal laser ablation of the prostate as a treatment for benign prostatic hyperplasia and prostate cancer: the results of a Delphi consensus project. Asian J Urol. 2024;11:271–9.
Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015;67:1066–96.
Lambertini L, Sandulli A, Coco S, Paganelli D, Cadenar A, Dell’Oglio P, et al. Complication rate across the minimally invasive surgical treatments (MISTs): where do we stand? A systematic review of the literature. Prostate Cancer Prostatic Dis. 2024 Oct 22. https://doi.org/10.1038/s41391-024-00900-5. Epub ahead of print. PMID: 39438691.
Author information
Authors and Affiliations
Contributions
AA, MLR, RN, and PP were responsible for interpreting data, editing and revising the tables, and writing the paper. EC, FS, and BG were responsible for collecting and reviewing journal articles, editing summary tables, and editing the manuscript. AA and AC were responsible for data analysis. MG was responsible for designing the review protocol, coordinating the group, and supervising the project. FS, AR, RC, AS, and SS provided feedback on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
As this is a systematic review, institutional review board or patient consent was not required. As for all systematic reviews, the patients presented in this systematic review have been previously reported.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alberti, A., Lo Re, M., Nicoletti, R. et al. Transperineal laser ablation in the management of benign prostatic hyperplasia: an updated systematic review and pooled analysis. Prostate Cancer Prostatic Dis (2025). https://doi.org/10.1038/s41391-025-00952-1
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41391-025-00952-1
This article is cited by
-
Outcomes and safety of trans perineal laser ablation of the prostate: a systematic review
World Journal of Urology (2025)
-
Commentary on “Ultrasound-guided Transperineal Prostate Thermal Ablation (TPTA) for Benign Prostatic Hyperplasia: Feasibility of an Outpatient Procedure using Radiofrequency Ablation”
CardioVascular and Interventional Radiology (2025)
-
Minimally invasive surgical techniques (MISTs) for benign prostatic hyperplasia: results from a Delphi consensus project to shed light on controversial topics
World Journal of Urology (2025)