Abstract
Background
Current National Comprehensive Cancer Network guidelines define brachytherapy monotherapy as a suitable treatment for favorable intermediate risk (FIR) and unfavorable intermediate risk (UIR) prostate cancer. Our objective is to define the subgroup of patients suitable for brachytherapy monotherapy.
Methods
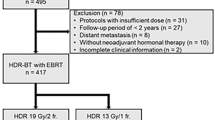
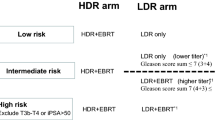
We conducted a single-institutional retrospective analysis of intermediate risk prostate cancer, treated with brachytherapy with or without androgen deprivation therapy (ADT) and/or external beam radiation therapy (EBRT). The primary endpoint was biochemical failure (BF), defined as prostate specific antigen (PSA) > 0.4 ng/mL. For monotherapy, multivariate Fine-Gray analysis was used to identify risk factors associated with BF. Univariate analysis was performed to evaluate whether ADT and/or EBRT were associated with BF for patients without and with such factors.
Results
Among 1622 patients, the median follow-up was 10.4 years. For monotherapy, PSA ≥ 10 ng/mL (adjusted sHR 3.01; 95% CI: 1.10–8.27; p = 0.032) and cT2b-c disease (adjusted sHR 4.52; 95% CI: 1.85–11.07; p = 0.001) were associated with BF. The 10-year incidences of BF after monotherapy for patients without and with these risk factors were 5.8% (3.8% FIR, 8.8% UIR) versus 17.2% (9.3% FIR, 23.9% UIR), respectively. For the cT1-T2a/PSA < 10 risk group, neither the addition of ADT (sHR 0.90; 95% CI: 0.38–2.1; p = 0.82) nor EBRT (sHR 0.65; 95% CI: 0.36-1.18; p = 0.16) was associated with biochemical failure. For the cT2b-T2c and/or PSA ≥ 10 subgroup, ADT (sHR: 0.33; 95% CI: 0.14–0.74; p = 0.007) but not EBRT (sHR 0.66; 95% CI: 0.34–1.31; p = 0.24) was associated with BF.
Conclusions
Brachytherapy monotherapy is suitable for all FIR, and UIR disease meeting cT1-T2a/PSA < 10 criteria.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to patient privacy concerns but reasonable data requests can be made to Dr. Grgur Mirić.
References
Michalski JM, Winter KA, Prestidge BR, Sanda MG, Amin M, Bice WS, et al. Effect of brachytherapy with external beam radiation therapy versus brachytherapy alone for intermediate-risk prostate cancer: NRG oncology RTOG 0232 randomized clinical trial. J Clin Oncol. 2023;41:4035–44.
King MT, Merrick GS, Galbreath RW, Fiano R, Butler WM, Wallner KE, et al. Prospective evaluation of supplemental external beam radiotherapy with palladium-103 prostate brachytherapy: long-term results of the 44/20/0 trials. Pract Radiat Oncol. 2025;15:e276-85.
NCCN Clinical Practice Guidelines in Oncology. Prostate Cancer. Versiion 2.2025. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
King MT, Keyes M, Frank SJ, Crook JM, Butler WM, Rossi PJ, et al. Low dose rate brachytherapy for primary treatment of localized prostate cancer: a systemic review and executive summary of an evidence-based consensus statement. Brachytherapy. 2021;20:1114–29.
Merrick GS, Butler WM. Modified uniform seed loading for prostate brachytherapy: rationale, design, and evaluation. Tech Urol. 2000;6:78–84.
Woo S, Han S, Kim TH, Suh CH, Westphalen AC, Hricak H, et al. Prognostic value of pretreatment MRI in patients with prostate cancer treated with radiation therapy: a systematic review and meta-analysis. Am J Roentgenol. 2019;214:597–604.
Rakauskas A, Peters M, Ball D, Kim NH, Ahmed HU, Winkler M, et al. The impact of local staging of prostate cancer determined on MRI or DRE at time of radical prostatectomy on progression-free survival: a Will Rogers phenomenon. Urol Oncol Semin Orig Investig https://www.sciencedirect.com/science/article/pii/S1078143922004057.
Baboudjian M, Gondran-Tellier B, Touzani A, Martini A, Diamand R, Roche JB, et al. Magnetic resonance imaging–based t-staging to predict biochemical recurrence after radical prostatectomy: a step towards the iTNM classification. Eur Urol Oncol. https://www.sciencedirect.com/science/article/pii/S2588931122001699.
Yang DD, Lee LK, Tsui JMG, Leeman JE, McClure HM, Sudhyadhom A, et al. AI-derived tumor volume from multiparametric mri and outcomes in localized prostate cancer. Radiology. 2024;313:e240041.
Gosselaar C, Kranse R, Roobol MJ, Roemeling S, Schröder FH. The interobserver variability of digital rectal examination in a large randomized trial for the screening of prostate cancer. Prostate. 2008;68:985–93.
Gandaglia G, Ploussard G, Valerio M, Mattei A, Fiori C, Roumiguié M, et al. The key combined value of multiparametric magnetic resonance imaging, and magnetic resonance imaging–targeted and concomitant systematic biopsies for the prediction of adverse pathological features in prostate cancer patients undergoing radical prostatectomy. Eur Urol. 2020;77:733–41.
Davis BJ, Pisansky TM, Wilson TM, Rothenberg HJ, Pacelli A, Hillman DW, et al. The radial distance of extraprostatic extension of prostate carcinoma. Cancer. 1999;85:2630–7.
Merrick GS, Butler WM, Dorsey AT, Lief JH, Benson ML. Seed fixity in the prostate/periprostatic region following brachytherapy. Int J Radiat Oncol Biol Phys. 2000;46:215–20.
Ho AY, Burri RJ, Jennings GT, Stone NN, Cesaretti JA, Stock RG. Is seminal vesicle implantation with permanent sources possible? A dose–volume histogram analysis in patients undergoing combined 103Pd implantation and external beam radiation for T3c prostate cancer. Brachytherapy. 2007;6:38–43.
Raman S, Keyes M, Oh J, Rousseau E, Krauze A, Wilson D, et al. Patterns of prostate cancer recurrence after brachytherapy determined by prostate-specific membrane antigen–positron emission tomography and computed tomography imaging. Int J Radiat Oncol. 2022;112:1126–34.
Morris WJ, Tyldesley S, Rodda S, Halperin R, Pai H, McKenzie M, et al. Androgen suppression combined with elective nodal and dose escalated radiation therapy (the ASCENDE-RT Trial): an analysis of survival endpoints for a randomized trial comparing a low-dose-rate brachytherapy boost to a dose-escalated external beam boost for high- and intermediate-risk prostate cancer. Int J Radiat Oncol. 2017;98:275–85.
Kishan AU, Dang A, Katz AJ, Mantz CA, Collins SP, Aghdam N, et al. Long-term outcomes of stereotactic body radiotherapy for low-risk and intermediate-risk prostate cancer. JAMA Netw Open. 2019;2:e188006.
Kennedy TAC, Ong WL, Quon H, Cheung P, Chu W, Chung H, et al. Stereotactic radiation therapy for localized prostate cancer: 10-year outcomes from three prospective trials. Int J Radiat Oncol. 2025;121:325–30.
Chang CM, McIntosh AG, Shapiro DD, Davis JW, Ward JF, Gregg JR. Does a screening digital rectal exam provide actionable clinical utility in patients with an elevated PSA and positive MRI?. BJUI Compass. 2021;2:188–93.
Zumsteg ZS, Spratt DE, Pei I, Zhang Z, Yamada Y, Kollmeier M, et al. A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur Urol. 2013;64:895–902.
Hoffman KE, Penson DF, Zhao Z, Huang LC, Conwill R, Laviana AA, et al. Patient-reported outcomes through 5 years for active surveillance, surgery, brachytherapy, or external beam radiation with or without androgen deprivation therapy for localized prostate cancer. JAMA. 2020;323:149–63.
Crook JM, Tang C, Thames H, Blanchard P, Sanders J, Ciezki J, et al. A biochemical definition of cure after brachytherapy for prostate cancer. Radiother Oncol. 2020;149:64–9.
Author information
Authors and Affiliations
Contributions
MK, GM, and PO conceived and designed the study. GM, RF, RG, and KW acquired data. MK, GM, and PO wrote the manuscript. MK, GM, PO, RF, RG, KW, and SM reviewed the manuscript for intellectual content.
Corresponding author
Ethics declarations
Competing interests
Martin King has received research funding from Palette Life Sciences, Bayer Healthcare, and AstraZeneca, outside of the submitted work. Grgur Mirić has served as a consultant for Theragenics, outside of the submitted work. Robert Galbreath has received a grant from Theragenics for statistical analysis of the submitted work. Peter Orio has received research funding, consulting fees, and stock for Palette Life Sciences, outside of the submitted work.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. Institutional-board approval has been obtained from the Bethany Ethical Research and Animal Care Committee (reference number S24-16). In addition, all patients signed an IRB-approved informed consent form at the time of treatment, which included consent for their clinical data to be used in future research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
King, M., Mirić, G., Galbreath, R. et al. Brachytherapy monotherapy for favorable and select unfavorable intermediate risk prostate cancer. Prostate Cancer Prostatic Dis (2025). https://doi.org/10.1038/s41391-025-01021-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41391-025-01021-3