Abstract
Background
Prostate cancer (PC) heterogeneity and treatment resistance remain major clinical challenges, with emerging evidence implicating the microbiome as a key modulator of disease pathogenesis. While microbial dysbiosis has been linked to PC diagnosis, progression, and therapeutic outcomes, the mechanisms underlying these associations are poorly understood. This review synthesizes current evidence on the diagnostic, prognostic, and therapeutic potential of the microbiome in PC.
Methods
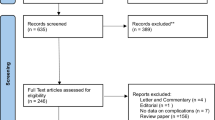
A systematic search of PubMed, Embase, and Cochrane Central Register of Controlled Trials (through April 2024) was conducted following PRISMA guidelines (PROSPERO: CRD42024534899). Controlled and observational studies investigating microbial roles in PC diagnosis (e.g., ISUP grading group), prognosis, or treatment response were included. Data extraction and quality assessment used the QUIPS tool. From 810 screened records, 42 studies met inclusion criteria.
Results
Distinct microbial profiles differentiated PC from controls, with Mycoplasma genitalium and Staphylococcus spp. enriched in prostate tumors (3.1- and 2.7-fold, respectively) and correlated with inflammation (IL-6: r = 0.38, p = 0.002). Urinary microbiota showed diagnostic potential (sensitivity: 58–82%), though sampling methods influenced variability. Prognostically, Betaproteobacteria gut enrichment predicted earlier castration-resistant progression (5.2 months; HR 1.8, 95% CI 1.3–2.5), while ADT-induced dysbiosis (e.g., Klebsiella overgrowth) accelerated resistance (2.1-fold risk). Therapies altered microbial ecology: radiotherapy depleted Bacteroides (linked to proctitis; OR 3.1), and immunotherapy responders harbored higher Akkermansia muciniphila. Microbial androgen synthesis and endotoxin production emerged as resistance mechanisms.
Conclusions
The microbiome influences PC detection, aggressiveness, and treatment efficacy through direct (tissue-resident) and indirect (gut-derived) mechanisms. Standardized profiling and microbiome-modulating strategies (e.g., probiotics during ADT) may personalize management. Prospective trials are needed to validate causality and translate microbial biomarkers into clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Vaccarella S, Li M, Bray F, Kvale R, Serraino D, Lorenzoni V, et al. Prostate cancer incidence and mortality in Europe and implications for screening activities: population based study. BMJ. 2024;386:e077738. https://doi.org/10.1136/bmj-2023-077738.
Hsing AW, Chokkalingam AP. Prostate cancer epidemiology. Front Biosci. 2006;11:1388–413. https://doi.org/10.2741/1891.
Rebello RJ, Oing C, Knudsen KE, Loeb S, Johnson DC, Reiter RE, et al. Prostate cancer. Nat Rev Dis Prim. 2021;7:1–27. https://doi.org/10.1038/s41572-020-00243-0.
Watson PA, Arora VK, Sawyers CL. Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat Rev Cancer. 2015;15:701–11. https://doi.org/10.1038/NRC4016.
Schwabe RF, Jobin C. The microbiome and cancer. Nat Rev Cancer. 2013;13:800–12. https://doi.org/10.1038/NRC3610.
Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets TV, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2018;359:97–103. https://doi.org/10.1126/SCIENCE.AAN4236.
De Marzo AM, Platz EA, Sutcliffe S, Xu J, Grönberg H, Drake CG, et al. Inflammation in prostate carcinogenesis. Nat Rev Cancer. 2007;7:256–69. https://doi.org/10.1038/NRC2090.
Tucci M, Bertaglia V, Vignani F, Buttigliero C, Fiori C, Porpiglia F, et al. Addition of docetaxel to androgen deprivation therapy for patients with hormone-sensitive metastatic prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016;69:563–73. https://doi.org/10.1016/J.EURURO.2015.09.013.
Pernigoni N, Zagato E, Calcinotto A, Troiani M, Mestre RP, Calì B, et al. Commensal bacteria promote endocrine resistance in prostate cancer through androgen biosynthesis. Science. 2021;374:216–24. https://doi.org/10.1126/SCIENCE.ABF8403/SUPPL_FILE/SCIENCE.ABF8403_SM.PDF.
Plottel CS, Blaser MJ. Microbiome and malignancy. Cell Host Microbe. 2011;10:324–35. https://doi.org/10.1016/J.CHOM.2011.10.003.
Wang I, Song L, Wang BY, Kalebasty AR, Uchio E, Zi X. Prostate cancer immunotherapy: a review of recent advancements with novel treatment methods and efficacy. Am J Clin Exp Urol. 2022;10:210.
Zitvogel L, Ma Y, Raoult D, Kroemer G, Gajewski TF. The microbiome in cancer immunotherapy: diagnostic tools and therapeutic strategies. Science. 2018;359:1366–70. https://doi.org/10.1126/SCIENCE.AAR6918.
Liu Q, Yang Y, Pan M, Yang F, Yu Y, Qian Z. Role of the gut microbiota in tumorigenesis and treatment. Theranostics. 2024;14:2304. https://doi.org/10.7150/THNO.91700.
Gilbert JA, Blaser MJ, Caporaso JG, Jansson JK, Lynch SV, Knight R. Current understanding of the human microbiome. Nature Med. 2018;24:392–400. https://doi.org/10.1038/nm.4517.
Knoll T, Omar MI, Maclennan S, Hernández V, Canfield S, Yuan Y, et al. Key steps in conducting systematic reviews for underpinning clinical practice guidelines: methodology of the European association of urology. Eur Urol. 2018;73:290–300. https://doi.org/10.1016/J.EURURO.2017.08.016.
Miyake M, Ohnishi K, Hori S, Nakano A, Nakano R, Yano H, et al. Mycoplasma genitalium Infection and chronic inflammation in human prostate cancer: detection using prostatectomy and needle biopsy specimens. Cells. 2019;8. https://doi.org/10.3390/cells8030212.
Cavarretta I, Ferrarese R, Cazzaniga W, Saita D, Lucianò R, Ceresola ER, et al. The microbiome of the prostate tumor microenvironment. Eur Urol. 2017;72:625–31. https://doi.org/10.1016/j.eururo.2017.03.029.
Ahn HK, Kim K, Park J, Kim KH. Urinary microbiome profile in men with genitourinary malignancies. Investig Clin Urol. 2022;63:569–76. https://doi.org/10.4111/icu.20220124.
Gonçalves MFM, Pina-Vaz T, Fernandes ÂR, Miranda IM, Silva CM, Rodrigues AG, et al. Microbiota of urine, glans and prostate biopsies in patients with prostate cancer reveals a dysbiosis in the genitourinary system. Cancers. 2023;15. https://doi.org/10.3390/cancers15051423.
Lee J, Wickes BL, Fu J, Brockman NE, Garg H, Jobin C, et al. Prevalence of genotoxic bacteria in men undergoing biopsy for prostate cancer. Prostate. 2023;83:663–9. https://doi.org/10.1002/pros.24500.
Kalinen S, Kallonen T, Gunell M, Ettala O, Jambor I, Knaapila J, et al. Differences in gut microbiota profiles and microbiota steroid hormone biosynthesis in men with and without prostate cancer. Eur Urol Open Sci. 2024;62:140–50. https://doi.org/10.1016/j.euros.2024.02.004.
Liu X, Dong Q. Associations between gut microbiota and three prostate diseases: a bidirectional two-sample Mendelian randomization study. Sci Rep. 2024;14. https://doi.org/10.1038/S41598-024-54293-5.
Feng Y, Jaratlerdsiri W, Patrick SM, Lyons RJ, Haynes AM, Collins CC, et al. Metagenomic analysis reveals a rich bacterial content in high-risk prostate tumors from African men. Prostate. 2019;79:1731–8. https://doi.org/10.1002/PROS.23897.
Salachan PV, Rasmussen M, Fredsøe J, Ulhøi B, Borre M, Sørensen KD. Microbiota of the prostate tumor environment investigated by whole-transcriptome profiling. Genome Med. 2022;14:9. https://doi.org/10.1186/s13073-022-01011-3.
Liu Y, Jiang H. Compositional differences of gut microbiome in matched hormone-sensitive and castration-resistant prostate cancer. Transl Androl Urol. 2020;9:1937–44. https://doi.org/10.21037/tau-20-566.
Terrisse S, Goubet AG, Ueda K, Thomas AM, Quiniou V, Thelemaque C, et al. Immune system and intestinal microbiota determine efficacy of androgen deprivation therapy against prostate cancer. J Immunother Cancer. 2022;10. https://doi.org/10.1136/JITC-2021-004191.
Kim JH, Seo H, Kim S, Ul-Haq A, Rahim MA, Jo S, et al. Biochemical recurrence in prostate cancer is associated with the composition of lactobacillus: microbiome analysis of prostatic tissue. Int J Mol Sci. 2023;24. https://doi.org/10.3390/ijms241310423.
Gioscio E, Rancati T, Avuzzi B, De Cecco L, Morlino S, Noris Chiorda B, et al. Modulations of gut microbiota following radiotherapy for prostate cancer. Radiother Oncol. 2020;152:S60–1. https://doi.org/10.1016/S0167-8140(21)00146-8.
Wang L. Changes in the gut microbial profile during long-term androgen deprivation therapy for prostate cancer. Prostate Cancer Prostatic Dis. 2023. https://doi.org/10.1038/s41391-023-00723-w.
Frugé AD, Ptacek T, Tsuruta Y, Morrow CD, Azrad M, Desmond RA, et al. Dietary changes impact the gut microbe composition in overweight and obese men with prostate cancer undergoing radical prostatectomy. J Acad Nutr Diet. 2018;118:714–23.e1. https://doi.org/10.1016/j.jand.2016.10.017.
Gilbert SM, Kuo Yfang, Shahinian VB. Prevalent and incident use of androgen deprivation therapy among men with prostate cancer in the United States. Urol Oncol. 2009;29:647. https://doi.org/10.1016/J.UROLONC.2009.09.004.
Kure A, Tsukimi T, Ishii C, Aw W, Obana N, Nakato G, et al. Gut environment changes due to androgen deprivation therapy in patients with prostate cancer. Prostate Cancer Prostatic Dis. 2023;26:323–30. https://doi.org/10.1038/s41391-022-00536-3.
Li JKM, Wang LL, Wong CYP, Chiu PKF, Teoh JYC, Kwok HSW, et al. A cross-sectional study on gut microbiota in prostate cancer patients with prostatectomy or androgen deprivation therapy. Prostate Cancer Prostatic Dis. 2021;24:1063–72. https://doi.org/10.1038/s41391-021-00360-1.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359:91–7. https://doi.org/10.1126/SCIENCE.AAN3706.
Maślak E, Miśta W, Złoch M, Błońska D, Pomastowski P, Monedeiro F, et al. A new approach to imaging and rapid microbiome identification for prostate cancer patients undergoing radiotherapy. Biomedicines. 2022;10. https://doi.org/10.3390/biomedicines10081806.
Peiffer LB, White JR, Jones CB, Slottke RE, Ernst SE, Moran AE, et al. Composition of gastrointestinal microbiota in association with treatment response in individuals with metastatic castrate resistant prostate cancer progressing on enzalutamide and initiating treatment with anti-PD-1 (pembrolizumab). Neoplasia. 2022;32:100822. https://doi.org/10.1016/j.neo.2022.100822.
Sfanos KS, Markowski MC, Peiffer LB, Ernst SE, White JR, Pienta KJ, et al. Compositional differences in gastrointestinal microbiota in prostate cancer patients treated with androgen axis-targeted therapies. Prostate Cancer Prostatic Dis. 2018;21:539–48. https://doi.org/10.1038/s41391-018-0061-x.
Liss M, Shah D, Leach R, Rourke E, Basler J, White J. Intestinal microbiome analysis identifies bacteria and biosynthesis pathways associated with prostate cancer. J Urol. 2018;199:e1112.
Wang L, Zheng YB, Yin S, Li KP, Wang JH, Bao EH, et al. Causal relationship between gut microbiota and prostate cancer contributes to the gut-prostate axis: insights from a Mendelian randomization study. Discov. Oncol. 2024;15. https://doi.org/10.1007/S12672-024-00925-1.
O’Toole PW, Jeffery IB. Gut microbiota and aging. Science. 2015;350:1214–5. https://doi.org/10.1126/SCIENCE.AAC8469.
Fransen F, van Beek AA, Borghuis T, Aidy SE, Hugenholtz F, van der Gaast-de Jongh C, Savelkoul HFJ. Aged gut microbiota contributes to systemical inflammaging after transfer to germ-free mice. Front Immunol. 2017;8:293898 https://doi.org/10.3389/FIMMU.2017.01385/BIBTEX.
Thevaranjan N, Puchta A, Schulz C, Naidoo A, Szamosi JC, Verschoor CP, et al. Age-associated microbial dysbiosis promotes intestinal permeability, systemic inflammation, and macrophage dysfunction. Cell Host Microbe. 2017;21:455–66.e4. https://doi.org/10.1016/J.CHOM.2017.03.002.
Rivera-Izquierdo M, de Rojas JP, Martínez-Ruiz V, Pérez-Gómez B, Sánchez MJ, Khan KS, et al. Obesity as a risk factor for prostate cancer mortality: a systematic review and dose-response meta-analysis of 280,199 patients. Cancers. 2021;13. https://doi.org/10.3390/CANCERS13164169.
Mingdong W, Xiang G, Yongjun Q, Mingshuai W, Hao P. Causal associations between gut microbiota and urological tumors: a two-sample mendelian randomization study. BMC Cancer. 2023;23. https://doi.org/10.1186/s12885-023-11383-3.
Xie Q, Hu B. Effects of gut microbiota on prostatic cancer: a two-sample Mendelian randomization study. Front Microbiol. 2023;14. https://doi.org/10.3389/fmicb.2023.1250369.
Author information
Authors and Affiliations
Contributions
AD and DG performed the systematic review, extracted and analyzed the data, and drafted the manuscript. Both authors contributed equally as first authors. MCM conceived and designed the study, supervised the project, provided critical revisions, and approved the final version of the manuscript. JPA, FQF, and CC contributed to the writing and critical revision of the manuscript. LL provided expertise on microbiota, and contributed to the interpretation of the findings.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Distante, A., Garino, D., Cerrato, C. et al. The role of the human microbiome in prostate cancer: a systematic review from diagnosis to treatment. Prostate Cancer Prostatic Dis (2025). https://doi.org/10.1038/s41391-025-01028-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41391-025-01028-w