Abstract
Study design
Survey.
Objectives
To investigate the needs and priorities of people with spinal cord injury for managing neurogenic bladder and bowel function and to determine their willingness to adopt neuromodulation interventions for these functions.
Methods
Anonymous online survey. It was advertised by word-of-mouth by community influencers and social media, and by advertisement in newsletters of advocacy groups.
Results
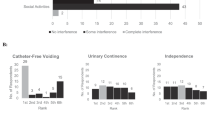
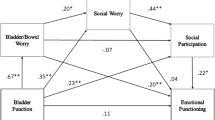
Responses from 370 individuals (27% female, 73% male) were included. Bladder emptying without catheters was the top priority for restoring bladder function, and maintaining fecal continence was the top priority for restoring bowel function. The biggest concerns regarding external stimulation systems were wearing a device with wires connecting to electrodes on the skin and having to don and doff the system daily as needed. The biggest concerns for implanted systems were the chances of experiencing problems with the implant that required a revision surgery or surgical removal of the whole system. Respondents were willing to accept an external (61%) or implanted (41%) device to achieve improved bladder or bowel function.
Conclusions
Bladder and bowel dysfunction remain important unmet challenges for individuals living with SCI who answered our survey. These individuals are willing to accept some potential risks of nerve stimulation approaches given potential benefits. Additional consumer input is critical for guiding both research and translation to clinical use and personalized medicine.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
French JS, Anderson-Erisman KD, Sutter M. What do spinal cord injury consumers want? A review of spinal cord injury consumer priorities and neuroprosthesis from the 2008 neural interfaces conference. Neuromodulation J Int Neuromodulation Soc. 2010;13:229–31.
Bragge P, Piccenna L, Middleton JW, et al. Developing a spinal cord injury research strategy using a structured process of evidence review and stakeholder dialogue. Part I: rapid review of SCI prioritisation literature. Spinal Cord. 2015;53:714–20.
Braaf S, Lennox A, Nunn A, Gabbe B. Social activity and relationship changes experienced by people with bowel and bladder dysfunction following spinal cord injury. Spinal Cord. 2017;55:679–86.
Park SE, Elliott S, Noonan VK, et al. Impact of bladder, bowel and sexual dysfunction on health status of people with thoracolumbar spinal cord injuries living in the community. J Spinal Cord Med. 2017;40:548–59.
Ren J, Chew DJ, Biers S, Thiruchelvam N. Electrical nerve stimulation to promote micturition in spinal cord injury patients: a review of current attempts. Neurourol Urodyn. 2016;35:365–70.
Brindley GS. The first 500 patients with sacral anterior root stimulator implants: general description. Paraplegia. 1994;32:795–805.
Martens FMJ, Heesakkers JPFA. Clinical results of a brindley procedure: sacral anterior root stimulation in combination with a rhizotomy of the dorsal roots. Adv Urol. 2011;2011:709708.
Creasey GH. Electrical stimulation of sacral roots for micturition after spinal cord injury. Urol Clin North Am. 1993;20:505–15.
Wheeler JS, Walter JS, Sibley P. Management of incontinent SCI patients with penile stimulation: preliminary results. J Am Paraplegia Soc. 1994;17:55–9.
Lee Y-H, Creasey GH. Self-controlled dorsal penile nerve stimulation to inhibit bladder hyperreflexia in incomplete spinal cord injury: a case report. Arch Phys Med Rehabil. 2002;83:273–7.
Opisso E, Borau A, Rijkhoff NJM. Subject-controlled stimulation of dorsal genital nerve to treat neurogenic detrusor overactivity at home. Neurourol Urodyn. 2013;32:1004–9.
Bourbeau DJ, Gustafson KJ, Brose SW. At-home genital nerve stimulation for individuals with SCI and neurogenic detrusor overactivity: a pilot feasibility study. J Spinal Cord Med. 2019;42:360–70.
Bhadra N, Bhadra N, Kilgore K, Gustafson KJ. High frequency electrical conduction block of the pudendal nerve. J Neural Eng. 2006;3:180–7.
Craggs M, McFarlane J. Neuromodulation of the lower urinary tract. Exp Physiol. 1999;84:149–60.
Wheeler TL, Bowel and Bladder Workshop Participants, de Groat W, Eisner K, Emmanuel A, French J, et al. Translating promising strategies for bowel and bladder management in spinal cord injury. Exp Neurol. 2018;306:169–76.
Anderson KD. Consideration of user priorities when developing neural prosthetics. J Neural Eng. 2009;6:055003.
Myer ENB, Petrikovets A, Slocum PD, et al. Risk factors for explantation due to infection after sacral neuromodulation: a multicenter retrospective case-control study. Am J Obstet Gynecol. 2018;219:78.e1–e9.
Weber PB, Kapur R, Gwinn RP, Zimmerman RS, Courtney TA, Morrell MJ. Infection and erosion rates in trials of a cranially implanted neurostimulator do not increase with subsequent neurostimulator placements. Stereotact Funct Neurosurg. 2017;95:325–9.
Wexner SD, Hull T, Edden Y, et al. Infection rates in a large investigational trial of sacral nerve stimulation for fecal incontinence. J Gastrointest Surg J Soc Surg Aliment Tract. 2010;14:1081–9.
National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. J Spinal Cord Med. 2014;37:355–6.
Wyndaele J-J. The management of neurogenic lower urinary tract dysfunction after spinal cord injury. Nat Rev Urol. 2016;13:705–14.
Inskip JA, Lucci V-EM, McGrath MS, Willms R, Claydon VE. A community perspective on bowel management and quality of life after spinal cord injury: the influence of autonomic dysreflexia. J Neurotrauma. 2018;35:1091–105.
Adriaansen JJ, van Asbeck FW, van Kuppevelt D, Snoek GJ, Post MW. Outcomes of neurogenic bowel management in individuals living with a spinal cord injury for at least 10 years. Arch Phys Med Rehabil. 2015;96:905–12.
Burns AS, St-Germain D, Connolly M, et al. Phenomenological study of neurogenic bowel from the perspective of individuals living with spinal cord injury. Arch Phys Med Rehabil. 2015;96:49–55.
Nafees B, Lloyd AJ, Ballinger RS, Emmanuel A. Managing neurogenic bowel dysfunction: what do patients prefer? A discrete choice experiment of patient preferences for transanal irrigation and standard bowel management. Patient Prefer Adherence. 2016;10:195–204.
Sanders PMH, Ijzerman MJ, Roach MJ, Gustafson KJ. Patient preferences for next generation neural prostheses to restore bladder function. Spinal Cord. 2011;49:113–9.
Harvey LA, Dijkers MP. Surveys can provide valuable data but careful consideration needs to be given to the methods used to sample the population of interest. Spinal Cord. 2020;58:257–8.
Funding
This work was supported in part by the U.S. Department of Veterans Affairs Rehabilitation Research and Development Service RX001962. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Author information
Authors and Affiliations
Contributions
DB, GC, BF, JF, TJ, AK, AR, BGS, KBT, TW, and JW contributed equally to survey design and implementation. DB, AB, WD, RK, and JS contributed to data analyses and reporting. All co-authors contributed to results interpretation and manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
KBT and BGS are co-authors and they work for Dignify Therapeutics Inc. and for Radiometer, respectively. These roles may present real or perceived conflict of interest.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bourbeau, D., Bolon, A., Creasey, G. et al. Needs, priorities, and attitudes of individuals with spinal cord injury toward nerve stimulation devices for bladder and bowel function: a survey. Spinal Cord 58, 1216–1226 (2020). https://doi.org/10.1038/s41393-020-00545-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-00545-w
This article is cited by
-
The effect of high frequency sacral nerve stimulation on lower urinary tract function in awake, healthy animals
Scientific Reports (2025)
-
Diet-microbiome interactions promote enteric nervous system resilience following spinal cord injury
npj Biofilms and Microbiomes (2024)
-
Priorities, needs and willingness of use of nerve stimulation devices for bladder and bowel function in people with spinal cord injury (SCI): an Australian survey
Spinal Cord Series and Cases (2024)
-
Model-free based adaptive BackStepping-Super Twisting-RBF neural network control with α-variable for 10 DOF lower limb exoskeleton
International Journal of Intelligent Robotics and Applications (2024)
-
The Fifth Bioelectronic Medicine Summit: today’s tools, tomorrow’s therapies
Bioelectronic Medicine (2023)