Abstract
Study design
Prospective observational cohort study.
Objectives
First, describe pressure injury (PI) and associated risk factors in individuals with spinal cord injury/disorder (SCI/D) during first rehabilitation. Second, evaluate a prediction model for hospital acquired PI (HAPI) development.
Setting
Acute care and rehabilitation clinic specialized in SCI/D.
Methods
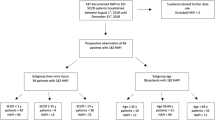
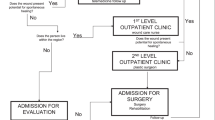
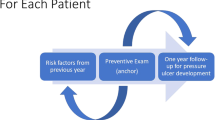
Patients ≥18 years of age with SCI/D were included during first rehabilitation between 08/2018 and 12/2019. We performed a systematic literature search to identify risk factors for PI development. Patients were classified according to HAPI developed. Between group differences of patients’ characteristics and risk factors were analyzed using descriptive statistics. Logistic predictive models were performed to estimate HAPI development and receiver operator characteristic (ROC) curve was used to test the model.
Results
In total, 94 patients were included, 48 (51.1%) developed at least one HAPI and in total 93 were observed, mainly stage I and stage II HAPI according to the European Pressure Ulcer Advisory Panel. We found nine significantly associated risk factors: completeness of SCI/D, pneumonia, sedative medications, autonomic dysreflexia, Braden ≤12 points, SCIPUS ≥9 points, lower admission SCIM and lower admission FIM-cognition, longer length of stay (LOS) (p ≤ 0.0005). In a predictive model, none of the risk factors was associated with HAPI development (AUC = 0.5).
Conclusion
HAPIs in patients with SCI/D during first rehabilitation are a frequent and complex condition and associated with several risk factors. No predictive model exists but with the identified risk factors of this study, larger studies can create a tailored and flexible HAPI risk prediction model.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
All data are stored with the corresponding author and can be asked directly (anke.scheel-sailer@paraplegie.ch).
References
von Groote PM, Bickenbach JE, Gutenbrunner C. The World Report on Disability–implications, perspectives and opportunities for physical and rehabilitation medicine (PRM). J Phys Med Rehabil. 2014;93:S4–11. https://doi.org/10.1097/PHM.0000000000000016
Group GD Pressure ulcers: prevention and management of pressure ulcers. 2014.
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016;43:585–97. https://doi.org/10.1097/won.0000000000000281
Ehrmann C, Mahmoudi SM, Prodinger B, Kiekens C, Ertzgaard P. Impact of spasticity on functioning in spinal cord injury: an application of graphical modelling. J Rehabilit Med. 2020;52:jrm00037.
Tschannen D, Anderson C. The pressure injury predictive model: a framework for hospital-acquired pressure injuries. J Clin Nurs. 2020;29:1398–421. https://doi.org/10.1111/jocn.15171. Epub 2020.
Henzel MK, Bogie KM, Guihan M, Ho CH Pressure ulcer management and research priorities for patients with spinal cord injury: consensus opinion from SCI QUERI Expert Panel on Pressure Ulcer Research Implementation. J RehabilitRes Dev. 2011;48:xi–xxxii.
van der Wielen H, Post MWM, Lay V, Glasche K, Scheel-Sailer A. Hospital-acquired pressure ulcers in spinal cord injured patients: time to occur, time until closure and risk factors. J Spinal Cord. 2016;54:726–31. https://doi.org/10.1038/sc.2015.239. Epub 2016.
Scheel-Sailer A, Wyss A, Boldt C, Post MW, Lay V. Prevalence, location, grade of pressure ulcers and association with specific patient characteristics in adult spinal cord injury patients during the hospital stay: a prospective cohort study. J Spinal Cord. 2013;51:828–33. https://doi.org/10.1038/sc.2013.91. Epub 2013.
Hoh DJ, Rahman M, Fargen KM, Neal D, Hoh BL. Establishing standard hospital performance measures for cervical spinal trauma: a Nationwide In-patient Sample study. Spinal Cord. 2016;54:306–13.
Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. J Spinal Cord. 1996;34:255–63. https://doi.org/10.1038/sc.1996.46
Marin J, Nixon J, Gorecki C. A systematic review of risk factors for the development and recurrence of pressure ulcers in people with spinal cord injuries. Spinal Cord. 2013;51:522–7.
Norton D. Calculating the risk: reflections on the Norton Scale. 1989. Adv Wound Care: J Prev Healing. 1996;9:38–43.
Bergstrom N, Braden BJ, Laguzza A, VH. TheBraden scale for predicting pressure sore risk. J Nurs Res. 1987;36:205–10.
Waterlow J. Pressure sores: a risk assessment card. Nursing. 1985;81:49–55.
Afridi A, Rathore FA. Are Risk Assessment Tools Effective for the Prevention of Pressure Ulcers Formation?: A Cochrane Review Summary With Commentary. Am J Phys Med Rehabilit. 2020;99:357–8.
Salzberg CA, Byrne DW, Cayten CG, van Niewerburgh P, Murphy JG, Viehbeck M. A new pressure ulcer risk assessment scale for individuals with spinal cord injury. Am J Phys Med Rehabil. 1996;75:96–104. https://doi.org/10.1097/00002060-199603000-00004
Scheel-Sailer A, Plattner C, Flückiger B, Ling B, Schaefer D, Baumberger M, et al. Dekubitus – ein. Update. 2016;16:489–98.
Meier C, Boes S, Gemperli A, Gmünder HP, Koligi K, Metzger S, et al. Treatment and cost of pressure injury stage III or IV in four patients with spinal cord injury: the Basel Decubitus Concept. Spinal Cord Ser Cases. 2019;5:30–30.
Mortenson WB, Miller WC. A review of scales for assessing the risk of developing a pressure ulcer in individuals with SCI. Spinal Cord. 2008;46:168–75. https://doi.org/10.1038/sj.sc.3102129. Epub 2007.
Betz R, Biering-Sørensen F, Burns SP, Donovan W, Graves DE, Guest J, et al. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)—What’s new? J Spinal Cord. 2019;57:815–17. https://doi.org/10.1038/s41393-019-0350-9. Epub 2019.
Organization WH Body Mass Index – BMI: WHO; 2020. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-massindex-bmi.
Association AH Blood Pressure Systolic 2020. https://www.heart.org/en/healthtopics/high-blood-pressure/understanding-blood-pressure-readings
Akpinar P, Atici A, Ozkan FU, Aktas I, Kulcu DG, Sarı A, et al. Reliability of the Modified Ashworth Scale and Modified Tardieu Scale in patients with spinal cord injuries. Spinal Cord. 2017;55:944–9.
Compton F, Strauss M, Hortig T, Frey J, Hoffmann F, Zidek W, et al. [Validity of the Waterlow scale for pressure ulcer risk assessment in the intensive care unit: a prospective analysis of 698 patients]. J Pflege. 2008;21:37–48. https://doi.org/10.1024/1012-5302.21.1.37
Anthony D, Parboteeah S, Saleh M, Papanikolaou P. Norton, Waterlow and Braden scores: a review of the literature and a comparison between the scores and clinical judgement. J Clin Nurs. 2008;17:646–53. https://doi.org/10.1111/j.1365-2702.2007.02029.x
Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol. 2014;13:844–54. https://doi.org/10.1016/S1474-4422(14)70120-6
Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75:127–32.
Stanley J, Sarfati D. The new measuring multimorbidity index predicted mortality better than Charlson and Elixhauser indices among the general population. J Clin Epidemiol. 2017;92:99–110. https://doi.org/10.1016/j.jclinepi.2017.08.005. Epub 2017.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. J Disabil Rehabil. 2007;29:1926–33. https://doi.org/10.1080/09638280601046302. Epub 2007.
Jenkins MA, Brown DJ, Ierino FL, Ratnaike SI. Cystatin C for estimation of glomerular filtration rate in patients with spinal cord injury. J Ann Clin Biochem. 2003;40:364–8. https://doi.org/10.1258/000456303766476995
Flett HM, Delparte JJ, Scovil CY, Higgins J, Laramée MT, Burns AS. Determining Pressure Injury Risk on Admission to Inpatient Spinal Cord Injury Rehabilitation: a Comparison of the FIM, Spinal Cord Injury Pressure Ulcer Scale, and Braden Scale. Arch Phys Med Rehabilit. 2019;100:1881–7.
Brienza D, Krishnan S, Karg P, Sowa G, Allegretti AL. Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study. Spinal Cord. 2018;56:28–34.
Grigorian A, Sugimoto M, Joe V, Schubl S, Lekawa M, Dolich M, et al. Pressure Ulcer in Trauma Patients: a Higher Spinal Cord Injury Level Leads to Higher Risk. J Am Coll Clin Wound Specialists. 2017;9:24–31. e1
Gour-Provencal G, Mac-Thiong J-M, Feldman DE, Bégin J, Richard-Denis A Decreasing pressure injuries and acute care length of stay in patients with acute traumatic spinal cord injury. J Spinal Cord Med 2020;1–9. https://doi.org/10.1080/10790268.2020.1718265
Sun ZW, Guo MR, Yang LZ, Chen ZJ, Zhang ZQ. Risk Factor Analysis and Risk Prediction Model Construction of Pressure Injury in Critically Ill Patients with Cancer: a Retrospective Cohort Study in China. Med Sci Monit: Int Med J Exp Clin Res. 2020;26:e926669.
Model D DAGitty Model 2020 [http://dagitty.net/]
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9. https://doi.org/10.1016/s0895-4356(96)00236-3
Fokkema M, Smits N, Zeileis A, Hothorn T, Kelderman H. Detecting treatmentsubgroup interactions in clustered data with generalized linear mixed-effects model trees. Behav Res Methods. 2018;50:2016–34.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885 https://doi.org/10.1371/journal.pmed.1001885.eCollection.
Acknowledgements
We thank the “Decu Care Team” (Jessica Decker, Eva Kissling, Rita Müller, Diana Sigrist-Nix, Ivonne Zamzow) for assistance with data collection and Karin Gläsche as the main supervising and responsible nurse. A special recognition goes to Stefanie Tesini for the composition of the database.
Funding
The authors received no funding in support of this study.
Author information
Authors and Affiliations
Contributions
KN, CN and AS-S: study design, data collection, data analysis, paper preparation. JK, COS: Study design, data analysis and statistics, paper preparation. MB, DJS, RW: Study design, paper preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests with respect to this research, authorship and publication of this paper. The work was a part of KN doctoral thesis (Dr med. Promotion).
Ethical approval
This study was conducted in compliance with the protocol, the current version of the Declaration of Helsinki, the ICH-GCP as well as all national legal and regulatory requirements, and excluded patients who denied their consent of further use of their data. All data were kept confidential and processed anonymously. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [39]. The Ethics Committees of Northwest and Central Switzerland approved this study involving humans on 25th November 2019 (EKNZ ID 2019-02179).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Najmanova, K., Neuhauser, C., Krebs, J. et al. Risk factors for hospital acquired pressure injury in patients with spinal cord injury during first rehabilitation: prospective cohort study. Spinal Cord 60, 45–52 (2022). https://doi.org/10.1038/s41393-021-00681-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-021-00681-x
This article is cited by
-
Risk factors of major complications after flap surgery in the treatment of stage III and IV pressure injury in people with spinal cord injury/disorder: a retrospective cohort study
Spinal Cord (2024)
-
Mixed-variable graphical modeling framework towards risk prediction of hospital-acquired pressure injury in spinal cord injury individuals
Scientific Reports (2024)
-
Predictors of hospital-acquired pressure injuries in patients with complete spinal cord injury: a retrospective case–control study
BMC Musculoskeletal Disorders (2023)
-
Risk constellation of hospital acquired pressure injuries in patients with a spinal cord injury/ disorder - focus on time since spinal cord injury/ disorder and patients’ age
Spinal Cord (2023)