Abstract
Introduction
Although neurological complications are well recognized in patients with sickle cell disease, myelopathy has been rarely described, with few reported cases of compressive and ischemic myelopathy. We present the first case report of longitudinally extensive myelitis (LETM) in SCD and review the differential diagnosis of myelopathy in these patients.
Case presentation
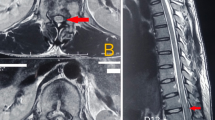
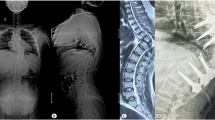
We report the case of a 29-year-old African-Brazilian man with SCD, who experienced a subacute flaccid paraparesis, with T2 sensory level and urinary retention. Cerebrospinal fluid analysis showed a lymphocytic pleocytosis and increased protein levels. MRI disclosed a longitudinally extensive spinal cord lesion, with a high T2/STIR signal extending from C2 to T12. We searched Medline/PubMed, Embase, Scopus, and Google Scholar databases for myelopathy in SCD patients.
Discussion
Spinal cord compression by vertebral fractures, extramedullary hematopoietic tissue, and Salmonella epidural abscess have been reported in SCD. We found only three case reports of spinal cord infarction, which is unexpectedly infrequent compared to the prevalence of cerebral infarction in SCD. We found only one case report of varicella-zoster myelitis and no previous report of LETM in SCD patients. Specific and time-sensitive causes of myelopathy should be considered in SCD patients. In addition to compression and ischemia, LETM is a possible mechanism of spinal cord involvement in SCD patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Data were obtained from the patient’s medical record, with the patient’s agreement. Patient personal information—including name or picture —is not mentioned in the text.
References
Sarnaik SA, Lusher JM. Neurological complications of sickle cell anemia. Am J Pediatr Hematol Oncol. 1982;4:386–94.
Holmstedt C, Adams RJ. Neurologic Complications of Hemoglobinopathies. Continuum 2011;17:56–72.
Farooq S, Testai FD. Neurologic complications of sickle cell disease. Curr Neurol Neurosci Rep. 2019;19:1–8.
Rudy HL, Yang D, Nam AD, Cho W. Review of sickle cell disease and spinal pathology. Glob Spine J. 2019;9:761–6.
Lewkow LM, Shah I. Sickle cell anemia and epidural extramedullary hematopoiesis. Am J Med. 1984;76:748–51.
Gardner RV. Salmonella vertebral osteomyelitis and epidural abscess in a child with sickle cell anemia. Pediatr Emerg Care. 1985;1:87–9.
Khoo HW, Chua YY, Chen JL. Salmonella typhi vertebral osteomyelitis and epidural abscess. Case Rep Orthop. 2016;2016:1–3.
Wolman L, Hardy AG. Spinal cord infarction associated with the sickle cell trait. Spinal Cord. 1970;7:282–91.
Rothman SM, Nelson JS. Spinal cord infarction in a patient with sickle cell anemia. Neurology. 1980;30:1072.
Márquez JC, Granados AM, Castillo M. MRI of cervical spinal cord infarction in a patient with sickle cell disease. Clin Imaging. 2012;36:595–8.
Mousali YM, Sobhi EM, Makkawi SO. Zoster myelitis in sickle cell anemia. Neurosci (Riyadh). 2011;16:273–5.
Kaplin AI, Krishnan C, Deshpande DM, Pardo CA, Kerr DA. Diagnosis and management of acute myelopathies. Neurologist. 2005;11:2–18.
Olaniyi JA, Alagbe K. Spinal Cord Discitis and Pathological Lumbar Fracture in a Sickle Cell Anaemia Patient: a case report. Int J Med Sci Public Health. 2015;48:1709.
Papavasiliou C, Gouliamos A, Vlahos L, Trakadas S, Kalovidouris A, Pouliades GR. CT and MRI of symptomatic spinal involvement by extramedullary haemopoiesis. Clin Radio. 1990;42:91–2.
Salehi SA, Koski T, Ondra SL. Spinal cord compression in beta-thalassemia: case report and review of the literature. Spinal Cord. 2004;42:117–23.
Sato DK, Callegaro D, Lana-Peixoto MA, Nakashima I, Fujihara K. Seronegative Neuromyelitis Optica Spectrum-The challenges on disease definition and pathogenesis. Arq Neuropsiquiatr. 2014;72:445–50.
Richert ME, Hosier H, Weltz AS, Wise ES, Joshi M, Diaz JJ. Acute transverse myelitis associated with Salmonella Bacteremia: a case report. Am J Case Rep. 2016;17:929.
Trebst C, Raab P, Voss EV, Rommer P, Abu-Mugheisib M, Zettl UK. Longitudinal extensive transverse myelitis- it ‘s not all neuromyelitis optica. Nat Rev Neurol. 2011 Dec;7:688.
Alblas CL, Bouvy WH, à Nijeholt GJ, Boiten J. Acute spinal-cord ischemia: evolution of MRI findings. J Clin Neurol. 2012;8:218.
Grassner L, Klausner F, Wagner M, McCoy M, Golaszewski S, Leis S, et al. Acute and chronic evolution of MRI findings in a case of posterior spinal cord ischemia. Spinal Cord. 2014;52:S23–4.
Barreras P, Fitzgerald KC, Mealy MA, Jimenez JA, Becker D, Newsome SD, et al. Clinical biomarkers differentiate myelitis from vascular and other causes of myelopathy. Neurology. 2018;90:e12–21.
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85:177–89.
Conran N, Belcher JD. Inflammation in sickle cell disease. Clin Hemorheol Microcirc. 2018;68:263–99.
Author contributions
Brum IV, Silva GD, Sodre DS, Nogueira FM, Pereira SLA, and Castro LHM made substantial contributions to the conception and design of the work, as well as acquisition, analysis, and interpretation of data; drafted the work or revised it critically for important intellectual content; approved the final version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
Written consent was obtained from the patient.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Brum, I.V., Silva, G.D., Sodre, D.S. et al. Myelopathy in sickle cell disease: a case-oriented review. Spinal Cord Ser Cases 7, 85 (2021). https://doi.org/10.1038/s41394-021-00449-8
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-021-00449-8