Abstract
Aberrant levels of blood markers reflecting inflammation and immune system activation have been implicated in psychotic disorders and linked to psychotic symptom severity. However, their predictive value for the long-term course of psychotic symptoms as well as the potential confounding and moderating role of cannabis use remain underexplored. We tested if baseline levels of immune markers previously linked to psychotic symptoms or treatment response (CRP, IL-1RA, sIL-2R, sTNFR1, sgp130) predicted 10-year outcomes in a first-episode psychosis sample (N = 320), and whether associations were moderated by baseline cannabis use. We assessed psychiatric (re)admissions and number of psychotic episodes during each year of the follow-up period, as well as change in positive psychotic symptom severity from baseline. Apart from sTNFR1, none of the immune markers significantly predicted psychosis outcomes independently of cannabis use. Baseline sTNFR1 was linked to lower risk of both (re)admissions and psychotic episodes, with an increasingly negative association over time. The statistical effects of CRP, IL-1RA, and sgp130 were all dependent on cannabis use. Specifically, negative (CRP, IL-1RA) or positive associations (sgp130) with psychiatric (re)admission risk or psychotic episode risk were observed in cannabis users only. Similarly, sgp130 was negatively associated with symptom change in cannabis users only. Some of these associations varied by follow-up year of the measured outcome (sgp130, IL-1RA). These findings challenge the prognostic and etiological significance of baseline immune markers for the course of positive psychotic symptoms and emphasize the importance of accounting for cannabis use.
Similar content being viewed by others
Introduction
Positive psychotic symptoms, such as delusions and hallucinations, are the transdiagnostic defining symptoms of psychotic disorders, but their long-term course is highly heterogeneous [1, 2]. Hence, prediction of related outcomes, such as risk of relapse, psychiatric hospitalization, or treatment resistance, remains challenging [1, 3,4,5], prompting a search for biomarkers that may improve existing prediction models [5,6,7].
Candidate biomarkers include measures of inflammatory processes and immune system activation, as growing evidence implicates their dysregulation in psychotic disorders such as schizophrenia [8,9,10]. This dysregulation is often reflected in aberrant circulating levels of immune markers, such as pro- and anti-inflammatory cytokines and their receptors as well as robust down-stream markers reflecting overall systemic inflammation such as C-reactive protein (CRP) [8, 9, 11]. While some of these aberrancies seem to be state-dependent, with aberrant levels mainly observed in acute but not chronic illness, some immune markers are considered ‘trait’ markers, with aberrant levels seen in acute and chronic illness phases [11, 12]. Such trait markers include both markers with primarily pro-inflammatory [CRP, interleukin (IL)-1β, IL-6, IL-8, tumor necrosis factor (TNF)-α] and anti-inflammatory [IL-1RA, IL-10] effects, or both [soluble interleukin-2 receptor (sIL-2R)], all circulating at elevated levels in both acute and chronic schizophrenia [12]. Elevated levels of anti-inflammatory markers may reflect a compensatory response to low-grade inflammation in psychosis [12, 13].
Immune marker aberrancies are not restricted to schizophrenia but also present in other severe mental disorders, including bipolar disorder and diagnostically heterogeneous samples of FEP [8, 14,15,16,17,18,19]. Furthermore, circulating immune marker levels have been linked to clinical indicators of illness severity, positive psychotic symptoms and number of relapses, treatment resistance, as well as general psychopathology [9, 20,21,22,23,24,25,26,27,28]. Hence, these markers might prove helpful in predicting the long-term course of psychotic symptoms and recurrence patterns of psychotic episodes. However, longitudinal studies are lacking and even fewer have considered FEP samples and long-term outcomes past the first year. Furthermore, findings have been inconsistent, particularly concerning outcomes capturing positive psychotic symptomatology: Concerning short-medium term outcomes (~1 year) in multi-episode schizophrenia patients, baseline immune markers were predictive of positive symptom change in one [29] but not another study [30], and not linked to relapse risk [31]. In some FEP samples, baseline immune markers, including CRP, IL-6, and soluble TNF-α receptor 1 (sTNFR1; reflective of TNF-α activity), predicted treatment response and positive psychotic change several months [32, 33] or one year later [34], while other studies found no association between baseline immune markers and short- [35] or medium-long term psychiatric outcomes (need for specialist care/psychiatric readmission) [36, 37].
These inconsistent findings could be related to differences in methodology and samples, including assessment of confounding or moderating factors. In the context of positive psychotic symptoms, relapse risk, and treatment resistance, a candidate confounder or moderator of relevance is cannabis use. Cannabis use has been linked to worsening of positive psychotic symptoms, increasing the risk for psychotic relapse and rehospitalization [38,39,40]. Moreover, it can modulate immune system activity [41, 42].
Immune cells express two of the main receptors of the endocannabinoid system, CB2 and (to a lesser extent) CB1, through which both endogenous and exogenous cannabinoids exert their effects [42,43,44]. Both endogenous and exogenous cannabinoids can influence leucocyte proliferation, T-cell and macrophage apoptosis, as well as cytokine secretion from these cells [41, 42]. In vitro and in vivo studies suggest a primarily immunosuppressive and anti-inflammatory effect of cannabinoids [41, 42, 45], including the exogenous cannabinoids Δ9-tetrahydrocannabinol (Δ9-THC) and cannabidiol (CBD), the most researched phytocannabinoids found in the Cannabis sativa plant. In humans, lifetime [46, 47], recent [48, 49], and heavy current [50] cannabis use has been associated with lower levels of various immune markers, including CRP, IL-6, TNF, and soluble TNF-α receptor 2 (sTNFR2).
Very few studies have investigated the relationship between immune markers and cannabis use in psychosis. Here, lower levels of pro-inflammatory and higher levels of anti-inflammatory markers were observed in individuals testing positive for cannabis via urinary drug screen [51,52,53,54] or reporting current [19] or recent [55] cannabis use, than in individuals who did not, and cannabis use cessation was found to increase CRP levels while improving clinical symptoms after four weeks [51, 52]. Considering the immunosuppressant and detrimental clinical effects of cannabis, its use is a highly relevant potential confounder of the association between immune marker levels and the course of positive psychotic symptoms. Furthermore, cross-sectional studies suggest an additional moderating (or ‘quasi-moderating’ [56]) role of cannabis use, with daily and adolescent cannabis use interacting with immune status to predict psychosis risk [14] and associations between cannabis use and psychotic symptom severity in established psychosis depending on current cannabis use status [53, 54]. However, to our knowledge, the confounding and possibly moderating role of cannabis use has so far not been adequately addressed in longitudinal studies on the relationship between immune markers and the long-term course of positive psychotic symptoms.
Our study aims to address the lack of studies on the long-term predictive potential of immune markers and on the putative role of cannabis use in moderating immune marker associations with psychosis outcomes. In a FEP sample, we measured multiple immune markers at baseline, reflecting activity in immunoinflammatory pathways that a) are assumed to be altered in a state-independent manner in psychotic disorders [12], and b) have previously been linked to treatment resistance, illness severity, and/or positive symptoms across different psychotic disorders in cross-sectional studies (CRP: e.g., [22,23,24, 57,58,59]; IL-1RA: e.g., [25, 60, 61]; sTNFR1: e.g., [26, 60, 62, 63]; sIL-2R: e.g., [28, 64, 65]; IL-6 pathway: e.g., [23, 24, 27, 59, 66]). Associations between these markers and the 10-year course of positive psychotic symptoms were investigated, captured by psychiatric (re)admissions, a commonly used indicator of relapse [67, 68], as well as by self-reports of concrete psychotic episodes and change in positive symptom severity from baseline to 10-year follow-up. Recent cannabis use at baseline was controlled for in analyses, and its possibly moderating role was investigated with interaction terms.
Methods
Participants
The study sample included patients recruited to the Thematically Organized Psychosis (TOP) project during their first adequate treatment from Oslo and two adjacent counties (Østfold and Innlandet) in Norway between 2004 and 2012. All were diagnosed with a non-affective psychotic disorder or a bipolar disorder with psychotic symptoms [69].
Of the initial 513 individuals with FEP, only those with plasma levels of at least one immune marker of interest, measured within ± 6 months of clinical baseline interviews, were selected for the current study (see below: Immune markers). Participants with CRP values ≥ 10 mg/L were excluded to rule out the influence of acute infections. This resulted in a baseline sample of N = 320 individuals (Supplementary Figure S1). Baseline data of this sample was linked to the National Patient Registry (NPR) to obtain information about contacts with specialized psychiatric health services within a 10-year follow-up time frame. For a subsample of these 320 individuals (n = 132), personal interview data collected after approximately 10 years (M = 9.30, SD = 1.56) was available for at least one of the measures of interest described in detail below: psychotic episodes during follow-up (n = 126) and change in positive psychotic symptom severity from baseline to follow-up (n = 130).
The study and all contributing procedures were conducted in line with the Declaration of Helsinki and approved by the Regional Committee for Medical Research Ethics South East Norway. All participants provided written informed consent before participation, which included permission to link their study data with data obtained from the NPR.
Clinical and cannabis use assessments
At baseline, psychiatric diagnoses were confirmed with the Structured Clinical Interview for Mental Disorders (SCID-I) [70], according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Demographic and clinical information was recorded, including age, sex, consumption of tobacco and/or nicotine products (daily nicotine yes vs. no), and current (antipsychotic) medication. To represent antipsychotic medication load, the daily dose of the currently prescribed primary antipsychotic (PDD) was divided by the corresponding Defined Daily Dose [71] (PDD/DDD ratio).
Recent cannabis use at baseline was measured as self-reported use during the past 6 months in a dichotomized manner (yes vs. no). Since the focus of the current study was to assess cannabis use status as a potential confounder and/or moderator as opposed to its predictive value of psychosis outcomes per se, and considering its comparatively acute effects on immune markers, lifetime use or frequency of use were not of primary interest. The dichotomized operationalization of recent or current use in this context is also more in line with previous, mainly cross-sectional, research in this field [19, 51,52,53,54,55].
At both baseline and 10-year follow-up, symptom severity was assessed with the Positive and Negative Symptom Scale (PANSS) [72]. Symptoms were grouped according to the 5-factor model proposed by Wallwork et al. [73], a recommended model for assessing symptoms in FEP [74]. Only the positive symptoms subscale was selected for the current study, consisting of the average rating across items p1 (delusions), p3 (hallucinations), p5 (grandiosity), g9 (unusual thought content), with larger scores reflecting higher symptom severity. Change in positive psychotic symptom severity from baseline to follow-up was calculated as ΔPANSS-Pos = PANSS-Pos baseline – PANSS-Pos follow-up. Here, larger positive scores indicate more improvement, i.e., a larger decrease in symptom severity, while negative scores indicate deterioration. Only participants with available ΔPANSS-pos scores were included in PANSS-based analyses (n = 130).
At follow-up, the number of episodes with manifest psychotic symptoms lasting ≥1 week during each year of the 10-year follow-up period was assessed retrospectively, using a time chart with a visual analog timeline. For analyses, these data were dichotomized per year (psychotic episode yes vs. no), and only participants with information on at least one of the 10 years were included (n = 126; average number of missing years: M = 0.85, SD = 1.50).
Registry data
Data from the NPR encompassed dates, duration, and level of care (inpatient care, outpatient contacts, or day treatment) of any contacts with specialized health services, as well as the primary ICD-10 diagnoses associated with a given contact. For each participant of the baseline sample (N = 320), any contacts due to schizophrenia spectrum diagnoses (ICD-10 codes F20-F29) or bipolar disorder (F31) that occurred during the ten years following the study baseline were extracted per year. For analyses, these data were dichotomized per year to reflect psychiatric (re)admission (yes vs. no). Since the digitally available data from the NPR only covered a time frame from 01.01.2008 to 31.12.2020, data were missing for some of the earlier years in earlier recruited participants and some of the later years in later recruited participants. For all 320 participants, information was available for at least four of the 10 included follow-up years (average number of missing years: M = 0.93, SD = 1.18).
Immune markers
Immune markers of interest measured at baseline included: CRP, a common marker of inflammation and infection, circulating at elevated levels during inflammatory conditions [75]; IL-1RA, a protein reflecting IL-1 concentrations and inhibiting IL-1 signaling, counteracting its pro-inflammatory effects by binding to IL-1 receptors [76]; sIL-2R, a soluble cytokine receptor reflecting T-cell activity and an ongoing immune response, with the potential for both pro- and anti-inflammatory effects through augmentation or inhibition, respectively, of pro-inflammatory IL-2 activity [77]; and sTNFR1, a soluble cytokine receptor reflecting TNF (α and β) activity and inhibiting its pro-inflammatory actions [78, 79]. To gauge activity in the IL-6 signaling pathway, sgp130 was measured, a soluble cytokine receptor with inhibiting effects on primarily the pro-inflammatory IL-6 trans-signaling [80,81,82]. While previous research on immune markers in psychosis has often focused on IL-6, sgp130 was selected here because, just like the other selected markers, it is assumed to be adequately robust, circulating at reasonably high plasma concentrations even in low-inflammation conditions, and with a sufficiently long biological half-life. Plasma levels of cytokines are not always detectable and/or reproducible [83], especially in low-inflammation conditions and when the respective cytokines are typically circulating at levels close to the detection threshold of conventional assays. Cytokine receptors, however, are often present at higher levels, are therefore more reliably detectable (e.g., sTNFR1 instead of TNF-α, sgp130 instead of IL-6) [60, 84, 85] and were thus selected for this study.
Baseline blood samples were taken approximately three weeks after the baseline clinical assessments. Occasionally, blood sampling was conducted earlier or had to be postponed, and samples measured within ± 6 months of the clinical interviews were still included in current analyses, overlapping with the time window of cannabis use assessments. For n = 11 participants, the time difference between baseline clinical assessments and blood sampling was >90 days. The average absolute time difference between baseline clinical assessments and blood sampling was M = 21.72 days (SD = 23.95). Baseline blood samples were taken between 8:00 and 17:00 from the antecubital vein and collected in EDTA vials. After overnight storage at 4 °C, plasma was extracted and stored at −80 °C. Immunological analyses of the thawed samples were conducted in 2013 at the Research Institute of Internal Medicine, Oslo University Hospital, with the accumulated storage time depending on the time point of sampling (M = 4.89 years, SD = 1.97 in the baseline sample, N = 320). Plasma levels of the different immune markers were measured in duplicate using enzyme immunoassays (EIA) with antibodies from R&D Systems (Minneapolis, MN, USA) in a 384-well plate, a SELMA (Jena, Germany) pipetting robot and a BioTek (Winooski, VT, USA) dispenser/washer. An Enzyme-Linked Immunosorbent Assay (ELISA) plate reader was used to measure absorbance at 450 nm, with wavelength correction set to 540 nm. Test reproducibility was good, with all intra- and inter-assay coefficients of variation <10%. Concentrations were measured in mg/L (CRP), ng/ml (sIL-2R, sTNFR1, sgp130) and pg/ml (IL-1RA). Values were log- and z-transformed for analyses. CRP concentrations were available for all 320 participants, but for four participants levels of IL-1RA, sTNFR1, sIL-2R, and sgp130 were missing.
Statistical analyses
Associations between immune marker levels and the different psychosis outcomes were assessed with logistic mixed effects models (psychiatric admissions, psychotic episodes) with a random intercept for participants, and linear regression models (ΔPANSS-Pos), implemented separately for the different immune markers. Predictors included main effects of the respective immune marker, cannabis use, and follow-up year (in mixed models only), as well as interactions between immune marker, cannabis use, and follow-up year (in mixed models only). Follow-up year interactions were included to consider that the predictive value of baseline immune marker levels may change as the illness progresses. All models were adjusted for baseline characteristics (age, sex, daily nicotine consumption, antipsychotic medication). ΔPANSS-Pos regression models were additionally adjusted for PANSS-Pos baseline scores, and scores were log-transformed prior to change score calculation to normalize model residuals. Testing was conducted two-sided, with a significance level of α = 0.05. As an incidence sample from a low-incidence disorder, the sample size is determined by baseline recruitment. Nevertheless, the relatively large sample size, recruited from a large and representative catchment area, and the use of a repeated measures approach, provide a strong foundation for detecting meaningful patterns in the data.
Analyses were implemented in R (version 4.2.3) [86], using the lme4 package for logistic mixed effects models (version 1.1-32) [87] and the sjPlot package for visualization of interaction effects (version 2.8.15) [88]. Model diagnostics were tested by inspection of residual distributions, using the DHARMa package (version 0.4.6) [89] for mixed models. Here, no issues concerning outliers, over- or underdispersion, or non-normality were detected, while minor deviations in quantile plots were tolerated.
Results
Study sample
Baseline characteristics of the 320 FEP participants are summarized in Table 1. Contrasts of immune marker levels by cannabis use status are provided in the Supplementary Information but are not of main interest for the current study. No significant differences were observed (see Supplementary Table S1).
Registry-based analyses
Logistic mixed effects models with psychiatric admission per follow-up year as the dependent variable revealed no significant main effects of either immune marker levels or cannabis use (Table 2). However, there were significant interactions between immune markers and cannabis use and/or year for the models including either CRP, IL-1RA, sgp130, or sTNFR1 as predictors.
Specifically, the effect of both CRP (OR = 0.27, p = 0.009, CI [0.1, 0.72]) and IL-1RA (OR = 0.20, p = 0.002, CI [0.07, 0.55]) on psychiatric admission risk varied by cannabis use, with a negative association observed in users but not in non-users (Fig. 1A, B). That is, in cannabis-using individuals, high baseline levels of these immune markers were associated with lower psychiatric admission risk over the 10-year follow-up period. In contrast, no association was observed in non-users (see Supplementary Tables S17, 18 for post-hoc analyses stratified by cannabis use).
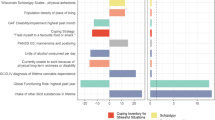
A–C Predicted probabilities of the significant interaction terms from the logistic mixed effects models, with CRP*cannabis use (A), IL-1RA*cannabis use (B), and sgp130*cannabis use*year (C). Colors indicate cannabis use category; shaded areas are 95% confidence intervals. For demonstration purposes, only 3 of the 10 follow-up years are displayed in C, see Figure S2 for all. D Summarized raw data, for demonstration purposes only: proportion of participants with psychiatric admissions per binned follow-up year pair, plotted separately for cannabis users and non-users, colored by level of sgp130 baseline concentration (above or below the median of the sample with available data on psychiatric readmissions, sgp130 levels, and cannabis use).
The effect of sgp130 was also dependent on cannabis use, but this varied additionally by follow-up year (OR = 1.20, p = 0.001, CI [1.07, 1.34]). With increasing years since baseline, higher sgp130 levels were associated with higher admission risk in cannabis users (Fig. 1C, D and S2; see Supplementary Table S19 for post-hoc analyses stratified by cannabis use).
Lastly, and independently of cannabis use, the effect of sTNFR1 on admission risk varied by follow-up year, albeit with a small effect size (OR = 0.95, p = 0.043, CI [0.91, 1.00]). Here, higher baseline concentrations of sTNFR1 were increasingly associated with a lower risk of psychiatric admission as time progressed (Fig. 2A, B).
A and C Predicted probabilities of the significant sTNFR1*year interaction term from the logistic mixed effects models with either psychiatric admission (A) or psychotic episode (C) as outcome. Colors indicate follow-up year; shaded areas are 95% confidence intervals. For demonstration purposes, only 3 of the 10 follow-up years are displayed. B and D Summarized raw data, for demonstration purposes only: proportion of participants with psychiatric admissions (B) or psychotic episodes (D) per binned follow-up year pair, colored by level of sTNFR1 baseline concentration (above or below the median of the sample with available data on the respective outcome, and sTNFR1 levels).
Interview-based analyses
To assess whether observations from the registry-based analyses could be replicated when investigating positive psychotic episodes specifically, and whether they would extend to changes in positive symptom severity, additional analyses were conducted, using the subsample of FEP participants with available clinical interview data at the 10-year follow-up (n = 132).
Psychotic episodes during follow-up
Like the registry-based analyses, logistic mixed effects models with psychotic episodes per follow-up year as the dependent variable revealed no significant main effects of either immune marker levels or cannabis use (Table 3). Instead, significant interactions between some of the immune markers, cannabis use and/or year were observed, although fewer than in registry-based analyses.
Here, the effect of IL-1RA was dependent on cannabis use, and this varied additionally by follow-up year (OR = 1.20, p = 0.024, CI [1.02, 1.40]). That is, similar to registry-based analyses, higher baseline concentrations of IL-1RA were associated with a lower risk of experiencing a psychotic episode but only in cannabis-using individuals. However, this effect diminished over time and was most pronounced during earlier follow-up years (Fig. 3A, B and S3; see Supplementary Table S20 for post-hoc analyses stratified by cannabis use). While association patterns for sgp130 mirrored those of registry-based analyses, with an interaction with cannabis use and follow-up year of similar effect size, indicating an increasingly positive association in later years in cannabis users, these findings did not reach the level of significance in this smaller sample (p = 0.056, Table 3).
A Psychotic episode risk: predicted probabilities of the significant interaction term from the logistic mixed effects model: IL-1RA*cannabis use*year. Colors indicate cannabis use category; shaded areas are 95% confidence intervals. For demonstration purposes, only 3 of the 10 follow-up years are displayed, see Figure S3 for all. B Summarized raw data, for demonstration purposes only: proportion of participants with psychotic episodes per binned follow-up year pair, plotted separately for cannabis users and non-users, colored by level of IL-1RA baseline concentration (above or below the median of the sample with available data on psychotic episodes, IL-1RA levels, and cannabis use). C ΔPANSS-Pos: predicted values of the significant interaction term from the linear regression model: sgp130*cannabis use. Colors indicate cannabis use category; shaded areas are 95% confidence intervals. D Summarized raw data, for demonstration purposes only: PANSS-Pos scores at baseline and 10-year follow-up, plotted separately for cannabis users and non-users, colored by level of sgp130 baseline concentration (above or below the median of the sample with available data on PANSS-pos scores, sgp130 levels, and cannabis use).
Similar to registry-based analyses, the effect of sTNFR1 on psychotic episode risk varied by follow-up year only (OR = 0.93, p = 0.038, CI [0.87, 1.00]). Again, higher baseline concentrations of sTNFR1 were increasingly associated with a lower risk over time and thus most strongly linked to a lower risk in later follow-up years (Fig. 2C, D).
Change in positive psychotic symptom severity
In linear regression analyses with ΔPANSS-Pos as the dependent variable, the effect of sgp130 was again dependent on cannabis use, while none of the other markers showed significant associations (Table 3). Specifically, in cannabis users, higher baseline concentrations of sgp130 were associated with less improvement in positive symptom severity (b = −0.21, p = 0.034, CI [−0.41, −0.02]; Fig. 3C, D; see Supplementary Table S21 for post-hoc analyses stratified by cannabis use).
Discussion
This study aimed to investigate the predictive value of various immune markers for the long-term course of psychotic symptoms and relapse in FEP while considering cannabis use as a potential confounder and moderator. Apart from sTNFR1, none of the immune markers were predictive of outcomes per se and independently of cannabis use. Instead, associations between psychosis outcomes and baseline levels of CRP, IL-1RA, and sgp130 varied significantly by cannabis use status.
Associations between immune markers and outcomes: cannabis-use independent effects
The only immune marker with a statistical effect on psychosis outcomes not moderated by cannabis use was sTNFR1, with higher baseline levels linked to lower risk of psychiatric admissions and psychotic episodes, particularly in later follow-up years. This conflicts with previous findings of primarily cross-sectional studies where higher sTNFR1 levels were linked to prior hospitalizations, treatment resistance, and poor functioning (e.g., [26, 60, 62, 63]), or where no associations between sTNFR1 levels and hospitalizations or symptom severity were observed (e.g., [90, 91]).
None of these studies, however, have considered long-term outcomes. Further, most of these studies assessed multi-episode and not FEP samples [26, 60, 62, 63] and treatment resistance was not specifically operationalized based on positive psychotic symptoms [26, 62, 63]. Importantly, concentrations of sTNFR1 have been found to increase with antipsychotic dose [63], and in response to clozapine [92]. Thus, previously observed links between levels of sTNFR1 and indicators of treatment resistance may at least partly be explained by the effects of clozapine and high doses of antipsychotics commonly administered in treatment-resistant patients. The findings of the current study may in part be affected by the relatively high percentage of individuals with a first psychotic bipolar disorder in the sample, shown to have particularly high sTNFR1 levels compared to other severe mental disorders [93] and a lower long-term risk of psychotic episode reoccurrence.
Notably, the sTNFR1 findings remain the exception in terms of cannabis-use-independent effects on psychosis outcomes. The prominent lack of main effects in covariate- and cannabis-controlled analyses and the absence of associations between most immune markers and outcomes in non-users of cannabis, challenge the assumption of a causal link between increased inflammation/immune system activation and the course of psychosis, at least as reflected by circulating levels of markers in our study. Such findings are in line with the null findings of some of the few existing longitudinal studies conducted to test the predictive value of baseline immune markers for psychosis outcomes similar to those of the current study, both in FEP [35,36,37] and in schizophrenia samples [31].
This does not preclude the possibility of inflammation contributing to the risk of developing a psychotic disorder initially, but might suggest that within individuals with psychosis, inflammation plays less of a causal role for positive psychotic symptom development in the long run.
Associations between immune markers and outcomes: cannabis-use dependent effects
In cannabis users only, baseline levels of CRP and IL-1RA showed a negative association with psychiatric admission risk over 10 years, with higher levels predicting lower risk. In contrast, levels of sgp130 were positively associated with admission risk in cannabis users, though predominantly in later follow-up years. Except for the CRP findings, these observations were largely replicated in analyses using the risk of new psychotic episodes as the outcome, though here the effect of IL-1RA diminished over time, and the effect of sgp130 did not reach statistical significance. Analyses of positive psychotic symptom change from baseline to 10-year follow-up revealed a comparable and significant effect of baseline sgp130, with higher levels predicting less symptom improvement.
The apparent diverging effects of the anti-inflammatory markers IL-1RA and sgp130 may be because the release of IL-1RA, similar to CRP, is stimulated by pro-inflammatory signals, including the pro-inflammatory cytokine IL-6 [76, 94], while levels of sgp130 do not seem to correlate consistently with levels of IL-6 [80,81,82, 95, 96]. Hence, one might speculate that levels of CRP and IL-1RA reflect pro-inflammatory activity, and levels of sgp130 anti-inflammatory activity, suggesting that in cannabis users, higher levels of markers indicating inflammation are associated with a lower risk of adverse outcomes, and higher levels of anti-inflammatory markers with a higher risk.
These findings are in line with the cross-sectional observations by Gibson et al. [54], who found a negative association between levels of IL-6 and positive symptom severity in cannabis users, but no association in non-users. Similarly, Romeo et al. [51] found that cannabis use cessation led to an increase in CRP levels accompanied by a decrease in clinical symptom severity in individuals with schizophrenia. Not considering cannabis use in analyses but including a substantial proportion of cannabis users in their sample of individuals with psychotic disorders, Stojanovic et al. [27] also observed a negative correlation between IL-6 levels and positive symptom severity.
Again, such findings are not easily reconcilable with the assumption of a causal link between increased inflammation/immune system activation and psychotic symptoms. While the underlying mechanisms are unknown, differences in use patterns within the group of cannabis users may offer an explanation. Dose-dependent effects of cannabinoids have been observed both for inflammation and psychotic relapse risk, with more frequent use and/or use of more potent substances linked to lower levels of pro-inflammatory and higher levels of anti-inflammatory immune markers (e.g., [97,98,99]), while increasing psychotic relapse risk (e.g., [2, 38, 100]). Hence, while speculative, within the group of cannabis users, those with particularly low baseline levels of pro- and high levels of anti-inflammatory markers might be those who tend to use cannabis more often or in stronger concentrations and are perhaps more likely to continue using throughout the course of illness, thus suppressing inflammation but increasing relapse risk in the long run.
The early prominence of the interaction effect between IL1-RA and cannabis use on psychotic episode risk may reflect a diminishing predictive power of certain baseline characteristics as the illness progresses, with cannabis use patterns, inflammatory status, and other psychotic relapse risk factors likely changing over time. In contrast, it is unclear why baseline sgp130 in cannabis users seems more predictive of long- than short-term outcomes. However, IL-6 signaling is complex and can be both pro- and anti-inflammatory depending on context [101]. Furthermore, while sgp130 has been shown to specifically attenuate IL-6 trans-signaling, reflecting an anti-inflammatory effect, sgp130 may also influence classical IL-6 signaling depending on molar excess of soluble IL-6 receptor sIL-6R [102]. Though speculative, high baseline sgp130 may confer short-term anti-inflammatory effects but could also reflect sustained IL-6 signaling which could be maladaptive and non-beneficial in the long-term. Notably, similar nonlinear associations have been reported in patients with acute coronary syndromes, where sgp130 may reflect a shift from compensatory to detrimental gp130-mediated signaling in the presence of high levels [103].
Limitations
Though longitudinal in nature, this study was purely observational, limiting the extent to which conclusions can be drawn about causality. The study focused on the predictive and clinically practical value of immune marker measurements, thus, only baseline levels of immune markers were considered. While most blood samples were taken close to the clinical baseline assessments (3 weeks), there was some variation among participants. Ideally, measures for all participants would be taken on the day of the assessments to minimize differences in treatment exposure. To shed more light on questions about causality and obtain a more fine-grained picture of how acute changes in immune marker levels are associated with acute changes in illness expression, future studies should measure immune markers repeatedly throughout the course of illness. Capturing time windows both during stable periods, acute relapse, and leading up to a relapse could elucidate whether increased immune marker levels precede or follow symptom exacerbation. Practically, this is difficult, however, and studies would need to be conducted at large scale so that enough sampling happens to fall into periods just before a relapse. It would further be interesting to assess immune marker levels prior to and after cannabis consumption to assess its acute and direct effects, but this remains ethically challenging.
Cannabis use was assessed in a dichotomous manner and only covering the past 6 months prior to baseline. Baseline cannabis use status was primarily considered as a confounder and/or moderator of the association between baseline immune markers and psychosis outcomes, and the study did not aim to assess effects of cannabis use on immune markers or psychosis outcomes per se. Hence, the question of potential frequency- or dose-dependent effects was less central, and the selected measure was deemed adequate for the purpose of the current study. Nevertheless, explorative subgroup analyses with information about cannabis use history, use frequency, use dosage, modes of use, and phytocannabinoid concentrations in the consumed product, would have been interesting and could have supported interpretations of observed effects. However, data at hand were insufficient for such analyses.
Lastly, although multiple potential confounders were considered in analyses, medication other than antipsychotics was not controlled for and residual confounding cannot be ruled out. The same is true for use of other recreational drugs, including alcohol. Previous research has specifically emphasized the role of cannabis both for psychosis outcomes and for immunoactivity, thus making it the main factor of interest for the current study. However, to what extent effects of other drugs, with e.g. primarily pro-inflammatory actions such as alcohol, also may moderate the relationship between immune markers and psychosis outcomes, remains to be investigated.
Concluding remarks
The findings of the current study provide only weak support for a general predictive value of various immune markers for the long-term course of psychotic symptoms but highlight the influence of cannabis use on this relationship. In light of the known interplay between the immune and the endocannabinoid system and the high prevalence of cannabis use in psychotic disorders, the number of studies investigating the effect of cannabis use on immune markers in individuals with psychosis is strikingly low [19, 49,50,51,52,53]. Additional research, both of cross-sectional and longitudinal nature, is urgently needed in this area.
The findings further cast doubt on the idea that increased inflammation per se is causally linked to a more severe long-term course of psychotic symptoms. Within cannabis users, mainly reverse associations were observed, with lower inflammation indicating a higher risk for selected adverse psychosis outcomes. Such observations might suggest that cannabis use-related dysregulation in immune responses, and not increased inflammation per se, could carry a certain risk for psychotic relapse. However, they may also be attributable to unmeasured factors such as particular use patterns, and the observed associations may not be causal. Observations of association patterns in non-users also mostly suggest an absence of any associations between immune markers and psychosis outcomes. It is possible that such associations emerge primarily over shorter timespans, e.g. leading up to a psychotic relapse, or that they are more prevalent in specific subgroups.
Data availability
Due to ethical restrictions, the data used in the current study are not publicly available. Interested parties may request access from the corresponding author through a reasonable inquiry, subject to approval by the Regional Ethics Committee.
References
Morgan C, Dazzan P, Lappin J, Heslin M, Donoghue K, Fearon P. Rethinking the course of psychotic disorders: modelling long-term symptom trajectories. Psychol Med. 2021;52:1–10.
Kreis I, Lagerberg TV, Wold KF, Åsbø G, Simonsen C, Flaaten CB, et al. Behind the heterogeneity in the long-term course of first-episode psychosis: different psychotic symptom trajectories are associated with different patterns of cannabis and stimulant use. Schizophr Res. 2024;271:91–99.
Alvarez-Jimenez M, Priede A, Hetrick SE, Bendall S, Killackey E, Parker AG, et al. Risk factors for relapse following treatment for first episode psychosis: A systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012;139:116–28.
Strålin P, Skott M, Cullberg J. Early predictors for late hospitalizations up to 14 years after first episode psychosis. Soc Psychiatry Psychiatr Epidemiol. 2021;56:1371–80.
Osimo EF, Perry BI, Mallikarjun P, Pritchard M, Lewis J, Katunda A, et al. Predicting treatment resistance from first-episode psychosis using routinely collected clinical information. Nat Ment Health. 2023;1:25–35.
Suvisaari J, Mantere O, Keinänen J, Mäntylä T, Rikandi E, Lindgren M, et al. Is it possible to predict the future in first-episode psychosis? Front Psychiatry. 2018;9:580.
Schubert KO, Clark SR, Baune BT. The use of clinical and biological characteristics to predict outcome following First Episode Psychosis. Aust N Z J Psychiatry. 2015;49:24–35.
Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–709.
Rodrigues-Amorim D, Rivera-Baltanas T, Spuch C, Caruncho HJ, Gonzalez-Fernandez A, Olivares JM, Agis-Balboa RC. Cytokines dysregulation in schizophrenia: a systematic review of psychoneuroimmune relationship. Schizophr Res. 2018;197:19–33.
Mongan D, Ramesar M, Föcking M, Cannon M, Cotter D. Role of inflammation in the pathogenesis of schizophrenia: a review of the evidence, proposed mechanisms and implications for treatment. Early Interv Psychiatry. 2020;14:385–97.
Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70:663–71.
Halstead S, Siskind D, Amft M, Wagner E, Yakimov V, Shih-Jung Liu Z, et al. Alteration patterns of peripheral concentrations of cytokines and associated inflammatory proteins in acute and chronic stages of schizophrenia: a systematic review and network meta-analysis. Lancet Psychiatry. 2023;10:260–71.
Roomruangwong C, Noto C, Kanchanatawan B, Anderson G, Kubera M, Carvalho AF, Maes M. The role of aberrations in the immune-inflammatory response system (IRS) and the compensatory immune-regulatory reflex system (CIRS) in different phenotypes of schizophrenia: the IRS-CIRS theory of schizophrenia. Mol Neurobiol. 2020;57:778–97.
Corsi-Zuelli F, Marques L, da Roza DL, Loureiro CM, Shuhama R, Di Forti M, et al. The independent and combined effects of cannabis use and systemic inflammation during the early stages of psychosis: exploring the two-hit hypothesis. Psychol Med. 2022;52:3874–84.
Upthegrove R, Manzanares-Teson N, Barnes NM. Cytokine function in medication-naive first episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2014;155:101–8.
Pillinger T, Osimo EF, Brugger S, Mondelli V, McCutcheon RA, Howes OD. A meta-analysis of immune parameters, variability, and assessment of modal distribution in psychosis and test of the immune subgroup hypothesis. Schizophr Bull. 2019;45:1120–33.
Noto C, Ota VK, Santoro ML, Ortiz BB, Rizzo LB, Higuchi CH, et al. Effects of depression on the cytokine profile in drug naïve first-episode psychosis. Schizophr Res. 2015;164:53–58.
Borovcanin M, Jovanovic I, Radosavljevic G, Djukic Dejanovic S, Bankovic D, Arsenijevic N, Lukic ML. Elevated serum level of type-2 cytokine and low IL-17 in first episode psychosis and schizophrenia in relapse. J Psychiatr Res. 2012;46:1421–6.
Di Nicola M, Cattaneo A, Hepgul N, Di Forti M, Aitchison KJ, Janiri L, et al. Serum and gene expression profile of cytokines in first-episode psychosis. Brain Behav Immun. 2013;31:90–95.
Miller BJ, Goldsmith DR. Inflammatory biomarkers in schizophrenia: Implications for heterogeneity and neurobiology. Biomarkers Neuropsychiatry. 2019;1:100006.
Fond G, Lançon C, Auquier P, Boyer L. C-reactive protein as a peripheral biomarker in schizophrenia. An updated systematic review. Front Psychiatry. 2018;9:392.
Liemburg EJ, Nolte IM, Klein HC, Knegtering H. Relation of inflammatory markers with symptoms of psychotic disorders: a large cohort study. Prog Neuropsychopharmacol Biol Psychiatry. 2018;86:89–94.
De Picker L, Fransen E, Coppens V, Timmers M, de Boer P, Oberacher H, et al. Immune and neuroendocrine trait and state markers in psychotic illness: decreased kynurenines marking psychotic exacerbations. Front Immunol. 2020;10:2971.
Garcia-Rizo C, Fernandez-Egea E, Oliveira C, Justicia A, Bernardo M, Kirkpatrick B. Inflammatory markers in antipsychotic-naïve patients with nonaffective psychosis and deficit vs. nondeficit features. Psychiatry Res. 2012;198:212–5.
Klemettilä JP, Kampman O, Seppälä N, Viikki M, Hämäläinen M, Moilanen E, Leinonen E. Cytokine and adipokine alterations in patients with schizophrenia treated with clozapine. Psychiatry Res. 2014;218:277–83.
Noto C, Maes M, Ota VK, Teixeira AL, Bressan RA, Gadelha A, Brietzke E. High predictive value of immune-inflammatory biomarkers for schizophrenia diagnosis and association with treatment resistance. World J Biol Psychiatry. 2015;16:422–9.
Stojanovic A, Martorell L, Montalvo I, Ortega L, Monseny R, Vilella E, Labad J. Increased serum interleukin-6 levels in early stages of psychosis: associations with at-risk mental states and the severity of psychotic symptoms. Psychoneuroendocrinology. 2014;41:23–32.
Igue R, Potvin S, Bah R, Stip E, Bouchard RH, Lipp O, et al. Soluble interleukin-2 receptor levels correlated with positive symptoms during quetiapine treatment in schizophrenia-spectrum disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1695–8.
Gonzalez-Blanco L, Maria PG-P, Garcia-Alvarez L, Lorena de la F-T, Garcia CI, Pilar AS, Julio B. Elevated C-reactive protein as a predictor of a random one-year clinical course in the first ten years of schizophrenia. Psychiatry Res. 2018;269:688–91.
Feng T, McEvoy JP, Miller BJ. Longitudinal study of inflammatory markers and psychopathology in schizophrenia. Schizophr Res. 2020;224:58–66.
Miller BJ, Lemos H, Schooler NR, Goff DC, Kopelowicz A, Lauriello J, et al. Longitudinal study of inflammation and relapse in schizophrenia. Schizophr Res. 2023;252:88–95.
Mondelli V, Ciufolini S, Belvederi Murri M, Bonaccorso S, Di Forti M, Giordano A, et al. Cortisol and inflammatory biomarkers predict poor treatment response in first episode psychosis. Schizophr Bull. 2015;41:1162–70.
Noto MN, Maes M, Nunes SOV, Ota VK, Rossaneis AC, Verri WA Jr., et al. Activation of the immune-inflammatory response system and the compensatory immune-regulatory system in antipsychotic naive first episode psychosis. Eur Neuropsychopharmacol. 2019;29:416–31.
Nettis MA, Pergola G, Kolliakou A, O’Connor J, Bonaccorso S, David A, et al. Metabolic-inflammatory status as predictor of clinical outcome at 1-year follow-up in patients with first episode psychosis. Psychoneuroendocrinology. 2019;99:145–53.
Barbosa S, Martinuzzi E, Sommer IE, Dazzan P, McGuire P, Arango C. Baseline levels of C-reactive protein and proinflammatory cytokines are not associated with early response to amisulpride in patients with first episode psychosis: the OPTiMiSE cohort study. Schizophrenia Bull Open. 2021;2:1–12.
Osimo EF, Perry BI, Cardinal RN, Lynall ME, Lewis J, Kudchadkar A, et al. Inflammatory and cardiometabolic markers at presentation with first episode psychosis and long-term clinical outcomes: a longitudinal study using electronic health records. Brain Behav Immun. 2021;91:117–27.
Horsdal HT, Köhler-Forsberg O, Benros ME, Gasse C. C-reactive protein and white blood cell levels in schizophrenia, bipolar disorders and depression - associations with mortality and psychiatric outcomes: a population-based study. Eur Psychiatry. 2017;44:164–72.
Schoeler T, Petros N, Di Forti M, Pingault JB, Klamerus E, Foglia E, et al. Association between continued cannabis use and risk of relapse in first-episode psychosis: a quasi-experimental investigation within an observational study. JAMA Psychiatry. 2016;73:1173–9.
Levi L, Bar-Haim M, Winter-van Rossum I, Davidson M, Leucht S, Fleischhacker WW, et al. Cannabis use and symptomatic relapse in first episode schizophrenia: trigger or consequence? data from the OPTIMISE study. Schizophr Bull. 2023;49:903–13.
Colizzi M, Burnett N, Costa R, De Agostini M, Griffin J, Bhattacharyya S. Longitudinal assessment of the effect of cannabis use on hospital readmission rates in early psychosis: a 6-year follow-up in an inpatient cohort. Psychiatry Res. 2018;268:381–7.
Anil SM, Peeri H, Koltai H. Medical cannabis activity against inflammation: active compounds and modes of action. Front Pharmacol. 2022;13:908198.
Katchan V, David P, Shoenfeld Y. Cannabinoids and autoimmune diseases: a systematic review. Autoimmun Rev. 2016;15:513–28.
Lu HC, Mackie K. An introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79:516–25.
Kaplan BL. The role of CB1 in immune modulation by cannabinoids. Pharmacol Ther. 2013;137:365–74.
Henshaw FR, Dewsbury LS, Lim CK, Steiner GZ. The effects of cannabinoids on pro- and anti-inflammatory cytokines: a systematic review of in vivo studies. Cannabis Cannabinoid Res. 2021;6:177–95.
Keen L 2nd, Pereira D, Latimer W. Self-reported lifetime marijuana use and interleukin-6 levels in middle-aged African Americans. Drug Alcohol Depend. 2014;140:156–60.
Keen L 2nd, Turner AD. Differential effects of self-reported lifetime marijuana use on interleukin-1 alpha and tumor necrosis factor in African American adults. J Behav Med. 2015;38:527–34.
Okafor CN, Li M, Paltzer J. Self-reported cannabis use and biomarkers of inflammation among adults in the United States. Brain Behav Immun Health. 2020;7:100109.
Ellis RJ, Peterson SN, Li Y, Schrier R, Iudicello J, Letendre S, et al. Recent cannabis use in HIV is associated with reduced inflammatory markers in CSF and blood. Neurol Neuroimmunol Neuroinflamm. 2020;7:e809.
Manuzak JA, Gott TM, Kirkwood JS, Coronado E, Hensley-McBain T, Miller C, et al. Heavy cannabis use associated with reduction in activated and inflammatory immune cell frequencies in antiretroviral therapy-treated human immunodeficiency virus-infected individuals. Clin Infect Dis. 2018;66:1872–82.
Romeo B, Lestra V, Martelli C, Benyamina A, Hamdani N. Cannabis cessation, inflammatory markers and schizophrenia. J Dual Diagnosis. 2022;18:33–41.
Romeo B, Lestra V, Martelli C, Amirouche A, Benyamina A, Hamdani N. Increased markers of inflammation after cannabis cessation and their association with psychotic symptoms. Acta Neuropsychiatrica. 2024;36:118–27.
Miller BJ, Buckley PF, McEvoy JP. Inflammation, substance use, psychopathology, and cognition in phase 1 of the clinical antipsychotic trials of intervention effectiveness study. Schizophr Res. 2018;195:275–82.
Gibson CL, Bassir Nia A, Spriggs SA, DeFrancisco D, Swift A, Perkel C, et al. Cannabinoid use in psychotic patients impacts inflammatory levels and their association with psychosis severity. Psychiatry Res. 2020;293:113380.
Szabo A, Akkouh IA, Ueland T, Lagerberg TV, Dieset I, Bjella T, et al. Cannabis Use Is Associated With Increased Levels of Soluble gp130 in Schizophrenia but Not in Bipolar Disorder. Front Psychiatry. 2020;11:642.
Sharma S, Durand RM, Gur-Arie O. Identification and analysis of moderator variables. J Mark Res. 1981;18:291–300.
Fernandes B, Steiner J, Bernstein H, Dodd S, Pasco J, Dean O, et al. C-reactive protein is increased in schizophrenia but is not altered by antipsychotics: meta-analysis and implications. Mol Psychiatry. 2016;21:554–64.
Weickert TW, Jacomb I, Lenroot R, Lappin J, Weinberg D, Brooks WS, et al. Adjunctive canakinumab reduces peripheral inflammation markers and improves positive symptoms in people with schizophrenia and inflammation: a randomized control trial. Brain Behav Immun. 2024;115:191–200.
Frydecka D, Misiak B, Pawlak-Adamska E, Karabon L, Tomkiewicz A, Sedlaczek P, et al. Interleukin-6: the missing element of the neurocognitive deterioration in schizophrenia? The focus on genetic underpinnings, cognitive impairment and clinical manifestation. Eur Arch Psychiatry Clin Neurosci. 2015;265:449–59.
Hope S, Ueland T, Steen NE, Dieset I, Lorentzen S, Berg AO, et al. Interleukin 1 receptor antagonist and soluble tumor necrosis factor receptor 1 are associated with general severity and psychotic symptoms in schizophrenia and bipolar disorder. Schizophr Res. 2013;145:36–42.
Maes M, Bocchio Chiavetto L, Bignotti S, Battisa Tura G, Pioli R, Boin F, et al. Effects of atypical antipsychotics on the inflammatory response system in schizophrenic patients resistant to treatment with typical neuroleptics. Eur Neuropsychopharmacol. 2000;10:119–24.
Noto C, Gadelha A, Belangero SI, Spindola LM, Rocha NP, de Miranda AS, et al. Circulating levels of sTNFR1 as a marker of severe clinical course in schizophrenia. J Psychiatr Res. 2013;47:467–71.
Nishimon S, Ohnuma T, Takebayashi Y, Katsuta N, Takeda M, Nakamura T, et al. High serum soluble tumor necrosis factor receptor 1 predicts poor treatment response in acute-stage schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2017;76:145–54.
Bresee C, Rapaport MH. Persistently increased serum soluble interleukin-2 receptors in continuously ill patients with schizophrenia. Int J Neuropsychopharmacol. 2009;12:861–5.
Szymona K, Zdzisińska B, Karakuła-Juchnowicz H, Kocki T, Kandefer-Szerszeń M, Flis M, et al. Correlations of Kynurenic Acid, 3-Hydroxykynurenine, sIL-2R, IFN-α, and IL-4 with clinical symptoms during acute relapse of schizophrenia. Neurotox Res. 2017;32:17–26.
Lin A, Kenis G, Bignotti S, Tura GJ, De Jong R, Bosmans E, et al. The inflammatory response system in treatment-resistant schizophrenia: increased serum interleukin-6. Schizophr Res. 1998;32:9–15.
Addington DE, Patten SB, McKenzie E, Addington J. Relationship between relapse and hospitalization in first-episode psychosis. Psychiatr Serv. 2013;64:796–9.
Schoeler T, Monk A, Sami MB, Klamerus E, Foglia E, Brown R, et al. Continued versus discontinued cannabis use in patients with psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:215–25.
Kreis I, Wold KF, Åsbø G, Simonsen C, Flaaten CB, Engen MJ, et al. The relationship between visual hallucinations, functioning, and suicidality over the course of illness: a 10-year follow-up study in first-episode psychosis. Schizophrenia. 2024;10:30.
First MB, Spitzer RL, Gibbon M, Williams JBW Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID I/P, Version 2.0). Biometrics Research Department, New York State Psychiatric Institute: New York, 1995.
WHO Collaborating Centre for Drug Statistics Methodology Norwegian Institute of Public Health, 2019. URL https://www.whocc.no. Accessed 9th June 2019.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76.
Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophr Res. 2012;137:246–50.
Langeveld J, Andreassen OA, Auestad B, Færden A, Hauge LJ, Joa I, et al. Is there an optimal factor structure of the Positive and Negative Syndrome Scale in patients with first-episode psychosis? Scand J Psychol. 2013;54:160–5.
Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Front Immunol. 2018;9:754.
Akdis M, Aab A, Altunbulakli C, Azkur K, Costa RA, Crameri R, et al. Interleukins (from IL-1 to IL-38), interferons, transforming growth factor β, and TNF-α: Receptors, functions, and roles in diseases. J Allergy Clin Immunol. 2016;138:984–1010.
Damoiseaux J. The IL-2 - IL-2 receptor pathway in health and disease: The role of the soluble IL-2 receptor. Clin Immunol. 2020;218:108515.
Girardin E, Roux-Lombard P, Grau GE, Suter P, Gallati H, Dayer JM. Imbalance between tumour necrosis factor-alpha and soluble TNF receptor concentrations in severe meningococcaemia. The J5 Study Group. Immunology. 1992;76:20–23.
Torres DJL, Arruda TR, Barros MDS, Gonçales JP, Soares AKA, Oliveira K, et al. Is a negative correlation between sTNFR1 and TNF in patients with chronic Chagas disease the key to clinical progression? Immunobiology. 2022;227:152166.
Askevold ET, Gullestad L, Dahl CP, Yndestad A, Ueland T, Aukrust P. Interleukin-6 Signaling, Soluble Glycoprotein 130, and Inflammation in Heart Failure. Curr Heart Fail Rep. 2014;11:146–55.
Jostock T, Müllberg J, Özbek S, Atreya R, Blinn G, Voltz N, et al. Soluble gp130 is the natural inhibitor of soluble interleukin-6 receptor transsignaling responses. Eur J Biochem. 2001;268:160–7.
Wolf J, Waetzig GH, Chalaris A, Reinheimer TM, Wege H, Rose-John S, Garbers C. Different soluble forms of the Interleukin-6 family signal transducer gp130 fine-tune the blockade of Interleukin-6 trans-signaling*. J Biol Chem. 2016;291:16186–96.
Gu Y, Zeleniuch-Jacquotte A, Linkov F, Koenig KL, Liu M, Velikokhatnaya L, et al. Reproducibility of serum cytokines and growth factors. Cytokine. 2009;45:44–49.
Baran P, Hansen S, Waetzig GH, Akbarzadeh M, Lamertz L, Huber HJ, et al. The balance of interleukin (IL)-6, IL-6·soluble IL-6 receptor (sIL-6R), and IL-6·sIL-6R·sgp130 complexes allows simultaneous classic and trans-signaling. J Biol Chem. 2018;293:6762–75.
Garbers C, Aparicio-Siegmund S, Rose-John S. The IL-6/gp130/STAT3 signaling axis: recent advances towards specific inhibition. Curr Opin Immunol. 2015;34:75–82.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria, 2023. URL https://www.R-project.org/.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
Lüdecke D sjPlot: Data Visualization for Statistics in Social Science. R package version 2.8.16, 2024. URL https://CRAN.R-project.org/package=sjPlot.
Hartig F DHARMa: Residual Diagnostics for Hierarchical (Multi-Level / Mixed) Regression Models. R package version 0.4.6, 2022. URL https://CRAN.R-project.org/package=DHARMa.
Wang X, Chen W, Gou M, Li W, Li N, Tong J, et al. Relationship between plasma TNF-α levels and agitation symptoms in first episode patients with schizophrenia. BMC Psychiatry. 2024;24:480.
Coelho FM, Reis HJ, Nicolato R, Romano-Silva MA, Teixeira MM, Bauer ME, Teixeira AL. Increased serum levels of inflammatory markers in chronic institutionalized patients with schizophrenia. Neuroimmunomodulation. 2008;15:140–4.
Kluge M, Schuld A, Schacht A, Himmerich H, Dalal MA, Wehmeier PM, et al. Effects of clozapine and olanzapine on cytokine systems are closely linked to weight gain and drug-induced fever. Psychoneuroendocrinology. 2009;34:118–28.
Goh XX, Tang PY, Tee SF. Meta-analysis of soluble tumour necrosis factor receptors in severe mental illnesses. J Psychiatr Res. 2023;165:180–90.
Steensberg A, Fischer CP, Keller C, Møller K, Pedersen BK. IL-6 enhances plasma IL-1ra, IL-10, and cortisol in humans. Am J Physiol Endocrinol Metab. 2003;285:E433–437.
Montero-Julian FA, Brailly H, Sautès C, Joyeux I, Dorval T, Mosseri V, et al. Characterization of soluble gp130 released by melanoma cell lines: a polyvalent antagonist of cytokines from the interleukin 6 family. Clin Cancer Res. 1997;3:1443–51.
Aparicio-Siegmund S, Garbers Y, Flynn CM, Waetzig GH, Gouni-Berthold I, Krone W, et al. The IL-6-neutralizing sIL-6R-sgp130 buffer system is disturbed in patients with type 2 diabetes. Am J Physiol Endocrinol Metab. 2019;317:E411–e420.
Gallily R, Yekhtin Z, Hanuš LO. Overcoming the bell-shaped dose-response of cannabidiol by using cannabis extract enriched in cannabidiol. Pharmacol Pharm. 2015;6:75–85.
Pacifici R, Zuccaro P, Pichini S, Roset PN, Poudevida S, Farré M, et al. Modulation of the immune system in cannabis users. JAMA. 2003;289:1929–31.
Watson CW, Campbell LM, Sun-Suslow N, Hong S, Umlauf A, Ellis RJ, et al. Daily Cannabis use is associated with lower CNS inflammation in people with HIV. J Int Neuropsychol Soc. 2021;27:661–72.
Schoeler T, Petros N, Di Forti M, Klamerus E, Foglia E, Ajnakina O, et al. Effects of continuation, frequency, and type of cannabis use on relapse in the first 2 years after onset of psychosis: an observational study. Lancet Psychiatry. 2016;3:947–53.
Hunter CA, Jones SA. IL-6 as a keystone cytokine in health and disease. Nat Immunol. 2015;16:448–57.
Garbers C, Thaiss W, Jones GW, Waetzig GH, Lorenzen I, Guilhot F, et al. Inhibition of classic signaling is a novel function of soluble glycoprotein 130 (sgp130), which is controlled by the ratio of interleukin 6 and soluble interleukin 6 receptor. J Biol Chem. 2011;286:42959–70.
Askevold ET, Nymo S, Ueland T, Gravning J, Wergeland R, Kjekshus J, et al. Soluble glycoprotein 130 predicts fatal outcomes in chronic heart failure. Circulation: Heart Fail. 2013;6:91–98.
Acknowledgements
We thank all participants for their valuable contribution and our local services for sensitive data storage (Tjenester for Sensitive Data, TSD p33 resource) supported by grant number #NS9666S. This work was further supported by grants from the Research Council of Norway to NORMENT Center of Excellence (Grant Numbers #223273/F50 and #287714) and the Southern and Eastern Norway Regional Health Authority (Grant Numbers #2006258, #2011085, #2014102, #2015088, #2018093). The funders played no role in study design, data collection, data analysis and interpretation, or the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the interpretation of results, the review and the editing of the manuscript. Specific roles, according to CRediT: I.K.: conceptualization, methodology, data curation, formal analysis, visualization, writing - original draft, writing – review and editing. I.M.: project administration and development, conceptualization, methodology, data curation, funding acquisition, supervision, writing – review and editing. K.F.W., G.Å., C.B.F., M.J.E., S.H.L. and L.H.W.: investigation (data collection), writing – review and editing. E.B.: investigation (data collection), data curation, writing – review and editing. M.A.S, M.C.F.W., T.U., N.E.S.: data curation, writing – review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kreis, I., Fjelnseth Wold, K., Åsbø, G. et al. Recent cannabis use affects the association between baseline immune markers and long-term outcomes in psychosis. Transl Psychiatry 15, 282 (2025). https://doi.org/10.1038/s41398-025-03498-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03498-x