Abstract
This study investigates the role of Early Growth Response 1 (EGR1) in extranodal natural killer/T-cell lymphoma (ENKTL) and its correlation with PD-L1 expression. Analysis of 62 ENKTL patient samples revealed that high EGR1 expression was linked to PD-L1 positivity, the immune evasion-A subtype, and early-stage disease. Although EGR1 expression was not an independent prognostic factor for overall survival, patients with higher EGR1 levels showed a trend toward better outcomes. In ENKTL cell lines (YT, SNK6), EGR1 positively regulated LMP1 and PD-L1 expression. Knockdown of EGR1 reduced PD-L1 levels, decreased PTEN, increased AKT phosphorylation, and abrogated STAT3 phosphorylation. Conversely, EGR1 overexpression enhanced PD-L1. Treatment with the histone deacetylase inhibitor entinostat upregulated both EGR1 and PD-L1, but this effect was lost in EGR1-depleted cells, indicating EGR1’s necessity for HDAC inhibitor–induced PD-L1 expression. These findings reveal EGR1’s pivotal role in tumor immune modulation and highlight potential combination therapies targeting EGR1, epigenetic regulators, and PD-1/PD-L1 checkpoints.

Similar content being viewed by others
Introduction
Extranodal natural killer/T-cell lymphoma (ENKTL) is a rare yet aggressive malignancy predominantly affecting East Asian and Latin American populations [1]. Although the Epstein-Barr virus (EBV) is well recognized as a key factor in ENKTL development, the molecular mechanisms underlying its development and progression remain poorly understood [2]. The adoption of concurrent chemoradiotherapy (CCRT), in combination with platinum-based or L-asparaginase-containing regimens, alongside the shift away from anthracycline-based treatments, has markedly improved outcomes for patients with ENKTL [3, 4]. Despite these advancements, the prognosis for patients with relapsed or refractory (R/R) ENKTL remains poor, underscoring the pressing need for more effective therapeutic strategies for this challenging population [5].
PD-L1 expression in ENKTL has been reported to be high (56-93%), spurring interest in PD-1/PD-L1 inhibitors [6,7,8]. A small Asian study evaluating pembrolizumab, an anti-PD-1 antibody, in seven patients with R/R ENKTL showed promising results: all patients responded to treatment and five achieved complete responses [9]. However, due to the limited sample size, the overall response to PD-1 blockade remains uncertain. Recent studies on pembrolizumab for R/R ENKTL have demonstrated modest overall response rates, yet responders exhibited promising 2-year progression-free survival (PFS) and overall survival (OS) rates of 53.0% and 60.7%, respectively. Furthermore, a notable plateau in survival curves suggests the potential for long-term disease control or even a ‘cure’ state through immune checkpoint inhibitors [10]. These findings underscore the critical need to identify robust predictive biomarkers for response to immune checkpoint inhibitors in R/R ENKTL. In a phase 2 study by Kim et al., treatment with avelumab in patients with R/R ENKTL indicated potential efficacy in a subset of patients, with PD-L1 expression emerging as a possible predictor of treatment response [11].
Early Growth Response 1 (EGR1) is a zinc finger transcription factor pivotal in regulating genes involved in cell proliferation, differentiation, and apoptosis [12]. In hematological malignancies, the role of EGR1 remains incompletely understood. Notably, increased EGR1 gene expression has been consistently observed in localized stages and low-risk groups, suggesting that EGR1 could serve as a potential prognostic marker for ENKTL [13]. Moreover, a novel classification system has been proposed to categorize ENKTL into four tumor immune microenvironment subtypes, among which the immune tolerance and immune evasion-A subtype is frequently observed in early-stage ENKTL [14].
In this study, we aim to explore the relationship between EGR1 and early-stage tumorigenesis, as well as the potential role EGR1 may play in maintaining immune tolerance or evasion. By elucidating the function of EGR1 in ENKTL, we hope to identify novel therapeutic targets that could enhance clinical outcomes for patients suffering from this aggressive lymphoma.
Methods
Patient selection and tissue samples
Patients diagnosed with ENKTL between 2006 and 2020 were included in this retrospective study. Inclusion criteria were pre-established and required: (1) a confirmed ENKTL diagnosis based on histological review according to the latest WHO classification criteria, and (2) availability of analyzable medical records. Formalin-fixed, paraffin-embedded (FFPE) tissue samples archived from these patients were utilized. Samples were excluded if they had insufficient tissue for analysis or a non-confirmed ENKTL diagnosis. Clinical data, including age, sex, Ann Arbor stage, Eastern Cooperative Oncology Group (ECOG) performance status, B symptoms, peripheral blood Epstein-Barr virus (EBV) DNA status, prognostic index for natural killer cell lymphoma (PINK), and treatment outcomes, were obtained from patient medical records. OS was calculated from the date of enrollment to the date of final follow-up or death from any cause. A total of 62 patient samples were included based on tissue availability, with no formal sample size calculation performed due to the retrospective nature of the study.
Immunohistochemistry
To evaluate EGR1 protein expression, immunohistochemistry (IHC) was performed on FFPE sections cut at a thickness of 4 µm. Slides were dried at 60 °C for 1 hour, deparaffinized in xylene, and rehydrated through a graded ethanol series. For EGR1 immunostaining, antigen retrieval was performed using citrate buffer (pH 9.0) in a pressure cooker for 30 minutes. Endogenous peroxidase activity was blocked with 3% H2O2 for 10 minutes. The primary antibody, anti-EGR1 rat monoclonal antibody (cat. # MAB28181; R&D Systems, MN, USA), was diluted 1:50 and incubated with the slides overnight at 4 °C. The VisUCyteTM HRP Polymer Antibody (cat. # VC001; R&D Systems) was used as the secondary antibody, and detection was carried out by treating the slides with 3,3’-diaminobenzidine (DAB) for 5 minutes. Hematoxylin was applied for nuclear counterstaining. All slides were processed alongside both positive and negative controls. Levels of expression were scored semi-quantitatively by assessing the average signal intensity in the nuclei of tumor cells. In this study, EGR1 expression with staining intensity equal to or greater than that of the basal cells in normal squamous epithelium was categorized as high expression; otherwise, it was categorized as low expression. Expression levels were semi-quantitatively scored based on average signal intensity (0 to 3). For this study, EGR1 expression was defined as high if the IHC score was ≥2 and low if it was <2.
IHC for immune subtype classification was conducted for CD68 (PG-M1, mild32, 1:300, Dako), PD-L1 (22C3, opti64/32, 1:50, Dako), and FoxP3 (236 A/E7, std1hr, 1:100, Abcam) using methods described in a previous study by Cho et al., except for single staining of PD-L1 instead of the double staining of PD-L1/EBV [6]. EBV in situ hybridization (EBV-ISH) was performed using an INFORM EBER (Epstein–Barr Virus Early RNA) Probe (#05278660001; Ventana Medical Systems) and a VENTANA ISH iVIEWBlue Detection Kit (#05278511001; Ventana Medical Systems) according to the manufacturer’s instructions. A BenchMark Ultra system (Ventana Medical Systems, Oro Valley, AZ, USA) was used for these IHC stainings and EBV-ISH.
Cell lines and culture conditions
The YT cell line was obtained from DSMZ (ACC434, Braunschweig, Germany), while the NK92-MI (CRL-2408) and 293 T (CRL-3216) cell lines were obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). The SNK6 cell line was kindly provided by Prof. Norio Shimizu (Tokyo Medical and Dental University, Tokyo, Japan). The YT cell line was maintained in Iscove’s Modified Dulbecco’s Medium (IMDM) supplemented with 20% fetal bovine serum (FBS) and 1% penicillin-streptomycin (PS). The NK92-MI cell line was maintained in alpha-MEM supplemented with 25% FBS, 0.2 mM inositol, 0.1 mM mercaptoethanol, 0.2 mM folic acid, and 1% PS. The SNK6 cell line was maintained at RPMI 1640 supplemented with 10% human serum (HS), 1% gentamycin, and 700 U/mL IL-2.
Antibodies and reagents
Phosphate buffered saline (PBS) was purchased from Welgene (Daejeon, Republic of Korea). Entinostat (S1053) waspurchased from Selleckchem (Houston, TX, USA). EGR1 (ab55160), LMP1 (ab78113), and PD-L1 (ab210931, ab213524) were purchased from Abcam (Cambridge, MA, USA). PTEN (cs#9188), p-AKT S473 (cs#4058), AKT (cs#9272), p-STAT3 T705 (cs#9145), β-actin (cs#4970), and vinculin (cs#9145) were purchased from Cell Signaling Technology (Beverly, MA, USA). RIG1 (sc-376845) and GAPDH (sc25778) were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). The BCA protein assay kit (BCA0500) and enhanced chemiluminescence (ECL, BWF0100) were purchased from BIOMAX (Guri, Republic of Korea). The lipofectamine 2000 reagent (11668019) was purchased from Thermo Fisher Scientific (Waltham, MA, USA). The human interleukin-2 (IL-2, C017-1000) was purchased from Enzynomics (Daejeon, Republic of Korea). The APC anti-human PD-L1 antibody (329708) was purchased from BioLegend (San Diego, California, USA). Entinostat (S1053), azacitidine (S1782), and decitabine (S1200) were purchased from Selleckchem (Houston, TX, USA). The human IL-2 (431807) and IFN-γ (430107) were purchased from BioLegend (San Diego, CA, USA).
Lentivirus production and transduction
Plasmids pMDLg/pRRE (Addgene #12251), pRSV/REV (Addgene #12253), and pMD2.G (Addgene #12259) were kindly provided by Prof. Didier Trono [PMID: 9765382]. The pLKO.1 puro plasmid (Addgene #8453) was kindly provided by Prof. Robert Weinberg [PMID: 12649500]. For EGR1 knockdown, a shRNA sequence (CTGTCTACTATTAAGGCCTTT) was inserted into pLKO.1 puro. Lentiviral particles carrying shEGR1 or control shRNA (scrambled) were produced in 293 T cells and used to transduce YT and SNK6 cells. Transduced cells were then treated with puromycin (2 µg/mL) for 7 days to achieve stable knockdown, followed by cell sorting. Knockdown efficiency was confirmed by western blot analysis of EGR1 protein levels.
Retrovirus production and transduction
The pMXs-hs-EGR1 plasmid (Addgene #52724) was kindly provided by Prof. Shinya Yamanaka [PMID: 24239284]. For EGR1 overexpression, the full-length EGR1 gene (pMXs-EGR1) was transfected into SNK6 cells using Lipofectamine 2000, following the manufacturer’s protocol. An empty plasmid (pMXs) served as a negative control. Successful EGR1 overexpression was confirmed by western blot.
Immunoblotting
Protein extracts were prepared by lysing cells in RIPA buffer containing protease and phosphatase inhibitors. Protein concentrations were determined using the BCA protein assay. Equal amounts of protein (20–30 µg) were separated on 10% SDS-PAGE gels, transferred to PVDF membranes, and blocked with 5% non-fat milk in TBS-T for 1 hour at room temperature. Membranes were incubated overnight at 4 °C with primary antibodies against EGR1 (1:2000), LMP1 (1:2000), RIG-1 (1:2000), PD-L1 (1:2000), γ-H2AX (1:2000), β-actin (1:2000), vinculin (1:2000), and GAPDH (1:2000), followed by HRP-conjugated secondary antibodies for 1 hour at room temperature. Protein bands were visualized using ECL solution.
Flow cytometry analysis
To assess membrane PD-L1 expression, cells were harvested, stained with a PD-L1 antibody (1:50 dilution) in the dark at 4 °C for 60 minutes, and subsequently washed three times in FACS wash buffer (15 minutes each wash). Data were acquired using an Attune NxT flow cytometer (Thermo Fisher Scientific, Waltham, MA, USA) and analyzed using FlowJo software. Results were presented as histograms comparing shCTRL and shEGR1 cells.
Cytokine measurement
The levels of IFN-γ in the culture supernatants were measured using ELISA kits (BioLegend, San Diego, CA, USA). Supernatants were collected 48 hours after transfection or knockdown, centrifuged to remove cell debris, and stored at −80 °C until analysis. The assays were performed according to the manufacturer’s instructions, and absorbance was measured at 450 nm using a Synergy H1 BioTek microplate reader.
Evaluation of the effect of HDAC inhibition on EGR1 and PD-L1 expression
Based on previous studies showing that histone deacetylase (HDAC) inhibitors enhance EGR1 expression [15, 16], we investigated whether HDAC inhibition could also augment PD-L1 expression. SNK6 cells were treated with increasing concentrations (0, 1, 5, or 10 μM) of entinostat for 24 hours. Protein levels of EGR1 and PD-L1 were analyzed by western blot using whole cell lysates.
Statistical analysis
Statistical analyses were performed using SPSS software version 25.0 (IBM Corp., USA) and GraphPad Prism version 8.0 (GraphPad Software, Inc., USA). Data are expressed as the mean ± standard deviation. For small sample sizes (n < 5), individual data points were plotted where applicable. Comparisons between groups were made using the Student’s t-test or analysis of variance (ANOVA) for continuous variables and the χ²-test for categorical variables. Data normality was assumed for parametric tests (t-test, ANOVA), and variance was assumed to be similar between groups unless otherwise indicated. Non-parametric tests were used where appropriate. OS was analyzed using the Kaplan-Meier method and the log-rank test. The correlation between EGR1 expression and clinical features or treatment response was assessed by the χ²-test. All tests were two-sided, and no adjustments were made for multiple comparisons. Two-sided P-values < 0.05 were considered statistically significant. This study adheres to the REMARK guidelines for reporting prognostic markers where applicable.
Results
Patient demographics and clinicopathologic features
A total of 62 patients with ENKTL were included in the study (Table 1). The median age was 52.8 years (IQR: 45.8–67.1), with 59.7% of patients aged ≤60 years. Most patients were male (77.4%). Most patients had an ECOG performance status of 0-1 (79.0%), and 64.5% were free of B symptoms. The primary tumor site was predominantly nasal (88.7%), and 74.2% of patients presented with Ann Arbor stage I-II disease. Regarding immune subtypes, 61.3% of patients were classified as immune evasion-A, followed by immune silenced (21.0%), immune evasion-B (14.5%), and immune tolerance (3.2%).
EGR1 expression and correlation with clinicopathologic characteristics
Analysis of EGR1 expression in tissue samples revealed significant associations with PD-L1 status and immune subtypes (Table 2). Patients with high EGR1 expression exhibited a higher rate of PD-L1 positivity compared to those with low EGR1 expression (81.3% vs. 43.3%, p = 0.002). Significant differences were also observed in the distribution of immune subtypes between the high and low EGR1 expression groups (p = 0.009). Specifically, the immune evasion-A subtype was more prevalent in the high EGR1 expression group than in the low EGR1 expression group, whereas the immune evasion-B and immune silenced subtypes were more common among patients with low EGR1 expression. Figure 1 shows representative histopathologic features, EBV in situ hybridization, and EGR1 immunohistochemistry findings from ENKTL patients. Panels A–C depict an 82-year-old male with the immune evasion-A subtype and high EGR1 expression, whereas panels D–F illustrate a 77-year-old female with the immune evasion-B subtype and low EGR1 expression. Additionally, patients with Ann Arbor stage I–II exhibited a higher proportion of high EGR1 expression compared to those with stage III–IV (p = 0.058), suggesting a potential trend of decreased EGR1 expression in advanced disease stages.
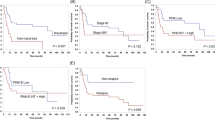
Survival analysis
Univariate and multivariate analyses were conducted to evaluate the prognostic impact of EGR1 expression and other clinicopathologic factors on overall survival (OS) (Table 3). In the univariate analysis, ECOG ≥ 2 (HR: 12.05, 95% CI: 4.78–30.41, p < 0.001) and high-risk PINK (HR: 8.88, 95% CI: 3.06–25.78, p < 0.001) were significantly associated with poorer OS. Low EGR1 expression showed a trend toward worse survival (HR: 1.65, 95% CI: 0.72–3.77, p = 0.235), but this did not reach statistical significance (Fig. 2). In multivariate analysis, ECOG ≥ 2 remained an independent predictor of poor OS (HR: 11.76, 95% CI: 4.13-33.52, p < 0.001). Although low EGR1 expression did not achieve statistical significance (HR: 2.12, 95% CI: 0.88-5.12, p = 0.096), it showed a potential association with reduced survival, suggesting that EGR1 may contribute to disease progression.
Differential expression of LMP1, RIG1, EGR1, and PD-L1 in ENKTL cell lines
Western blot analysis was performed to compare the expression of LMP1, RIG1, EGR1, and PD-L1 in ENKTL cell lines (YT, SNK6) and the non-tumorigenic control NK92-MI cells (Fig. 3A). Among these lines, SNK6 showed notably higher levels of LMP1, RIG1, EGR1, and membrane-bound PD-L1 compared to the other cell lines. To elucidate the role of EGR1 in regulating LMP1 and PD-L1 expression, we conducted EGR1 knockdown experiments in YT and SNK6 cells using shRNA (Fig. 3B). Western blot analysis showed that EGR1 depletion led to a marked reduction in LMP1 expression in both cell lines, with a particularly pronounced effect in SNK6 cells. Importantly, both the reduced and membrane-bound forms of PD-L1 showed substantial decreases following EGR1 knockdown, most notably in SNK6 cells (Fig. 3B). Flow cytometry further confirmed that EGR1 knockdown significantly decreased surface PD-L1 levels in SNK6 cells (p < 0.001), while YT cells demonstrated a similar but less pronounced effect (Fig. 3C). Collectively, these results suggest that EGR1 functions as a positive regulator of both LMP1 and PD-L1 expression in ENKTL, revealing a novel regulatory mechanism in ENKTL pathogenesis.
To evaluate the impact of EGR1 overexpression on LMP1, RIG1, and PD-L1 expression, SNK6 cells were transfected with the pMXs-EGR1 plasmid and analyzed by Western blot (Fig. 3D). LMP1 expression appeared slightly increased in pMXs-EGR1-transfected cells, while RIG1 showed minimal change. In contrast, PD-L1 protein expression exhibited a notable increase in pMXs-EGR1-treated cells compared to controls. This upregulation of PD-L1 suggests that EGR1 overexpression enhances the expression of this important immune checkpoint molecule in SNK6 cells.
Regulation of signaling pathways by EGR1 knockdown in ENKTL cell lines
To investigate the downstream signaling pathways regulated by EGR1 in ENKTL cells, we examined the expression of key signaling molecules in YT and SNK6 cells following EGR1 knockdown (Fig. 4A). Western blot analysis revealed distinct patterns of pathway activation between the two cell lines. In SNK6 cells, EGR1 knockdown led to significant changes in multiple signaling pathways. Notably, there was decreased PTEN expression accompanied by increased AKT phosphorylation at Ser473, indicating enhanced activation of the PI3K/AKT pathway. HIF-1α levels showed a slight increase, while STAT3 phosphorylation at Tyr705 was completely abolished following EGR1 depletion. In contrast, YT cells showed minimal changes in these signaling pathways after EGR1 knockdown. These findings imply that EGR1 plays a crucial role in regulating the PTEN/AKT axis in SNK6 cells, where its depletion decreases PTEN expression and consequently activates AKT signaling. Additionally, the complete loss of STAT3 phosphorylation in SNK6 cells indicates that EGR1 is essential for maintaining STAT3 activation in these cells.
Western blot analysis showing the effect of IFN-γ (20 ng/mL, 24 h) treatment on PD-L1 protein expression in YT and SNK6 cells (Fig. 4B). In YT cells, IFN-γ treatment results in minimal changes in PD-L1 expression. In contrast, SNK6 cells exhibit a significant upregulation of PD-L1 in the shCTRL condition upon IFN-γ treatment, whereas the shEGR1 condition shows little to no induction. These data indicate that IFN-γ–mediated PD-L1 induction in SNK6 cells is dependent on EGR1.
Effect of HDAC inhibitor on EGR1 and PD-L1 expression
Western blot analysis of EGR1 and PD-L1 protein levels was performed in SNK6 cells treated with varying concentrations of entinostat (0, 1, 5, and 10 µM) for 24 hours. EGR1 expression increased in a dose-dependent manner following entinostat treatment, accompanied by a corresponding upregulation of PD-L1 (Fig. 5A). Additional Western blot analysis of PD-L1 expression in SNK6 cells transduced with either control shRNA (shCTRL) or EGR1 knockdown shRNA (shEGR1_a) and treated with entinostat (0, 1, or 10 µM) for 24 hours revealed that PD-L1 expression increased upon entinostat treatment in shCTRL cells (shown in both short and long exposures). However, this increase was significantly attenuated in EGR1 knockdown cells (shEGR1_a), indicating that EGR1 is required for entinostat-induced PD-L1 expression (Fig. 5B).
Discussion
This study provides novel insights into the role of EGR1 in ENKTL pathogenesis and highlights its potential as a therapeutic target. Our findings reveal complex interactions between EGR1, PD-L1, and key signaling pathways in ENKTL, with significant implications for disease progression and treatment strategies.
Our analysis of 62 ENKTL patients revealed significant associations between EGR1 expression and important clinicopathologic features. First, the correlation between high EGR1 expression and PD-L1 positivity suggests that EGR1 may be involved in modulating the tumor immune microenvironment in ENKTL. This relationship is further supported by the enrichment of the immune evasion-A subtype—known for its active immune escape features—in patients with high EGR1 expression. In contrast, low EGR1 expression was associated with the immune silenced subtype, indicating that EGR1 may help shape the immunological phenotype of ENKTL and potentially influence the balance between active immune evasion and passive immune silence. This finding is consistent with our in vitro results and supports the hypothesis that EGR1 plays a crucial role in immune evasion mechanisms in ENKTL. Moreover, the observation that patients with early-stage disease tended to have higher EGR1 expression, coupled with a trend toward better survival in patients with high EGR1 expression, suggests that EGR1 may influence the tumor’s ability to engage the immune system during the early stages of the disease.
EBV infection plays a pivotal role in the development of ENKTL. EBV-infected NK/T cells typically exhibit a latency II gene expression profile characterized by LMP1 expression, a viral protein implicated in tumorigenesis [17, 18]. LMP1 promotes oncogenesis by activating multiple signaling pathways, including NF-κB and JAK/STAT, thereby facilitating cell proliferation and survival [19, 20]. LMP1 also upregulates PD-L1 expression, enabling tumor cells to evade T cell-mediated immune surveillance and foster a tumor-promoting microenvironment [21, 22]. The data obtained from ENKTL cell lines, particularly SNK6, strongly support EGR1 as a positive regulator of LMP1 and PD-L1 expression. The pronounced reduction in both reduced and membrane-bound PD-L1 following EGR1 knockdown underscores the importance of EGR1 in maintaining PD-L1 levels. Since PD-L1 is a critical immune checkpoint molecule enabling tumor immune escape, EGR1’s influence on PD-L1 suggests that it may help shape the tumor’s immunosuppressive microenvironment. Beyond immune checkpoint regulation, our analyses revealed significant EGR1-dependent signaling alterations. In SNK6 cells, EGR1 depletion reduced PTEN levels and enhanced AKT phosphorylation, indicating that EGR1 normally restrains the PI3K/AKT pathway. The complete loss of STAT3 phosphorylation in EGR1 knockdown cells further emphasizes the multifaceted nature of EGR1’s regulatory functions, as STAT3 is a crucial transcription factor involved in cell growth, survival, and immune modulation [23, 24]. Taken together, these findings suggest that EGR1 coordinates a complex network of signals, simultaneously regulating tumor growth, survival pathways, and immune evasion strategies. Furthermore, our experiments demonstrated that EGR1 was essential for IFN-γ–mediated PD-L1 expression, underscoring its critical role in immune signaling and modulation in ENKTL. Garcia-Diaz et al. reported that IFN-γ regulated PD-L1 expression through the JAK1/JAK2–STAT1–IRF1 axis in a melanoma model [25]. In the present study, the mechanism by which EGR1 is involved in IFN-γ signaling in ENKTL may be similar to or interact with that of IRF1. However, further research is needed to explore the effects of EGR1 on other immune-regulatory genes beyond PD-L1 downstream of IFN-γ signaling.
Previous studies have shown that although PD-L1 expression is elevated in ENKTL, responses to PD-1 blockade therapies have been modest [10, 11]. Retrospective analyses of pembrolizumab-treated patients indicate that some responders achieve long-term disease control and favorable prognoses, while non-responders experience rapid disease progression. Notably, patients with the immune evasion-A subtype tend to respond well to PD-1 blockade, whereas those with the immune evasion-B and immune silence subtypes do not respond [11, 14]. EGR1 overexpression experiments reinforce its importance in regulating PD-L1. The observation that elevated EGR1 drives PD-L1 upregulation aligns with our knockdown data and further confirms EGR1’s role as a critical enhancer of PD-L1 expression. To elucidate the therapeutic potential of targeting the EGR1-PD-L1 axis, we selected the HDAC inhibitor entinostat, given its established role in reactivating EGR1 expression in other malignancies [15, 16].The attenuated PD-L1 induction under entinostat treatment in EGR1-depleted cells demonstrates that EGR1 is required for the epigenetic modulation of PD-L1 expression. To explore other epigenetic regulators, we tested the hypomethylating agent Azacitidine in SNK6 cells but observed no significant dose-dependent increase in EGR1 or PD-L1 expression, unlike entinostat. This suggests that HDAC inhibitors may be more effective in modulating the EGR1-PD-L1 axis in ENKTL, though further studies on DNA methyltransferase inhibitors and other HDACs are warranted. Preclinical and early-phase clinical trials have shown promise for combining HDAC and PD-1 inhibitors to overcome resistance to checkpoint blockade immunotherapy [26, 27]. A recent phase Ib/II trial demonstrated that the combination of sintilimab (an anti-PD-1 antibody) and chidamide (a HDAC inhibitor) might be effective in patients with R/R ENKTL [28]. This suggests that epigenetic therapies might leverage EGR1 to potentiate immune checkpoint expression, potentially enhancing the effectiveness of immunotherapy in ENKTL.
Despite these promising findings, several limitations must be acknowledged. First, while low EGR1 expression showed a trend toward worse OS, it did not reach statistical significance, rendering the clinical prognostic impact of EGR1 unclear. This may be attributable to the relatively small sample size and the heterogeneity of ENKTL, which likely constrained statistical power. Consequently, further validation in larger cohorts is warranted to clarify the potential of EGR1 as a prognostic marker in ENKTL. Second, as ENKTL is a rare malignancy, recruiting sufficient patients at a single institution is challenging, resulting in a limited cohort size that restricts the generalizability of our findings, particularly given the heterogeneity of ENKTL immune subtypes. Validation in larger, multi-institutional cohorts is therefore essential to confirm the broader applicability of our results. Third, the translational relevance of EGR1’s role in PD-L1 regulation for PD-1 blockade therapy remains uncertain due to the small number of patients treated with pembrolizumab (n = 7) and the lack of biopsy samples at the time of treatment, necessitating reliance on diagnostic biopsies for EGR1 assessment. Larger studies correlating EGR1 expression and immune subtype status with PD-1 inhibitor response are needed. Fourth, although our in vitro experiments provided valuable insights, in vivo validation is necessary to substantiate these findings.
In conclusion, this study elucidates EGR1’s pivotal role in ENKTL pathogenesis, particularly in regulating PD-L1 expression and key signaling pathways. These findings deepen our understanding of ENKTL biology and open new avenues for therapeutic interventions targeting this aggressive lymphoma.
Data availability
The data may be obtained from the corresponding authors on reasonable request.
References
Jaffe ES, Chan JK, Su IJ, Frizzera G, Mori S, Feller AC, et al. Report of the workshop on nasal and related extranodal angiocentric t/natural killer cell lymphomas. Definitions, differential diagnosis, and epidemiology. Am J Surg Pathol. 1996;20:103–11.
Shimoyama Y, Oyama T, Asano N, Oshiro A, Suzuki R, Kagami Y, et al. Senile epstein-barr virus-associated b-cell lymphoproliferative disorders: A mini review. J Clin Exp Hematop. 2006;46:1–4.
Kim SJ, Kim K, Kim BS, Kim CY, Suh C, Huh J, et al. Phase ii trial of concurrent radiation and weekly cisplatin followed by vipd chemotherapy in newly diagnosed, stage ie to iie, nasal, extranodal nk/t-cell lymphoma: Consortium for improving survival of lymphoma study. J Clin Oncol. 2009;27:6027–32.
Yamaguchi M, Suzuki R, Oguchi M. Advances in the treatment of extranodal nk/t-cell lymphoma, nasal type. Blood. 2018;131:2528–40.
Lim SH, Hong JY, Lim ST, Hong H, Arnoud J, Zhao W, et al. Beyond first-line non-anthracycline-based chemotherapy for extranodal nk/t-cell lymphoma: Clinical outcome and current perspectives on salvage therapy for patients after first relapse and progression of disease. Ann Oncol. 2017;28:2199–205.
Jo JC, Kim M, Choi Y, Kim HJ, Kim JE, Chae SW, et al. Expression of programmed cell death 1 and programmed cell death ligand 1 in extranodal nk/t-cell lymphoma, nasal type. Ann Hematol. 2017;96:25–31.
Kim WY, Jung HY, Nam SJ, Kim TM, Heo DS, Kim CW, et al. Expression of programmed cell death ligand 1 (pd-l1) in advanced stage ebv-associated extranodal nk/t cell lymphoma is associated with better prognosis. Virchows Arch. 2016;469:581–90.
Han L, Liu F, Li R, Li Z, Chen X, Zhou Z, et al. Role of programmed death ligands in effective t-cell interactions in extranodal natural killer/t-cell lymphoma. Oncol Lett. 2014;8:1461–9.
Kwong YL, Chan TSY, Tan D, Kim SJ, Poon LM, Mow B, et al. Pd1 blockade with pembrolizumab is highly effective in relapsed or refractory nk/t-cell lymphoma failing l-asparaginase. Blood. 2017;129:2437–42.
Lee JY, Kwon JH, Hur JY, Yi JH, Lee JH, Cho H, et al. Pembrolizumab for patients with relapsed or refractory extranodal nk/t-cell lymphoma in korea. Cancer Res Treat. 2024;56:681–7.
Kim SJ, Lim JQ, Laurensia Y, Cho J, Yoon SE, Lee JY, et al. Avelumab for the treatment of relapsed or refractory extranodal nk/t-cell lymphoma: An open-label phase 2 study. Blood. 2020;136:2754–63.
Thiel G, Cibelli G. Regulation of life and death by the zinc finger transcription factor egr-1. J Cell Physiol. 2002;193:287–92.
Lee JY, Kim JH, Bang H, Cho J, Ko YH, Kim SJ, et al. Egr1 as a potential marker of prognosis in extranodal nk/t-cell lymphoma. Sci Rep. 2021;11:10342.
Cho J, Kim SJ, Park WY, Kim J, Woo J, Kim G, et al. Immune subtyping of extranodal nk/t-cell lymphoma: A new biomarker and an immune shift during disease progression. Mod Pathol. 2020;33:603–15.
Lanzi C, Favini E, Dal Bo L, Tortoreto M, Arrighetti N, Zaffaroni N, et al. Upregulation of erk-egr1-heparanase axis by hdac inhibitors provides targets for rational therapeutic intervention in synovial sarcoma. J Exp Clin Cancer Res. 2021;40:381.
Wilson AJ, Chueh AC, Tögel L, Corner GA, Ahmed N, Goel S, et al. Apoptotic sensitivity of colon cancer cells to histone deacetylase inhibitors is mediated by an sp1/sp3-activated transcriptional program involving immediate-early gene induction. Cancer Res. 2010;70:609–20.
Gru AA, Haverkos BH, Freud AG, Hastings J, Nowacki NB, Barrionuevo C, et al. The epstein-barr virus (ebv) in t cell and nk cell lymphomas: Time for a reassessment. Curr Hematol Malig Rep. 2015;10:456–67.
Song W, Gao Y, Wu J, Li H, Shi Z, Gong C, et al. Lmp1 enhances aerobic glycolysis in natural killer/t cell lymphoma. Cell Death Dis. 2024;15:604.
Ersing I, Bernhardt K, Gewurz BE. Nf-κb and irf7 pathway activation by epstein-barr virus latent membrane protein 1. Viruses. 2013;5:1587–606.
Gires O, Kohlhuber F, Kilger E, Baumann M, Kieser A, Kaiser C, et al. Latent membrane protein 1 of epstein-barr virus interacts with jak3 and activates stat proteins. Embo j. 1999;18:3064–73.
Fang W, Zhang J, Hong S, Zhan J, Chen N, Qin T, et al. Ebv-driven lmp1 and ifn-γ up-regulate pd-l1 in nasopharyngeal carcinoma: Implications for oncotargeted therapy. Oncotarget. 2014;5:12189–202.
Moyano A, Ferressini N, De Matteo E, Preciado MV, Chabay P. Pd-l1 is upregulated in cd163+ tonsillar macrophages from children undergoing ebv primary infection. Front Immunol. 2022;13:940910.
Wang W, Lopez McDonald MC, Kim C, Ma M, Pan ZT, Kaufmann C, et al. The complementary roles of stat3 and stat1 in cancer biology: Insights into tumor pathogenesis and therapeutic strategies. Front Immunol. 2023;14:1265818.
Wang Y, Shen Y, Wang S, Shen Q, Zhou X. The role of stat3 in leading the crosstalk between human cancers and the immune system. Cancer Lett. 2018;415:117–28.
Garcia-Diaz A, Shin DS, Moreno BH, Saco J, Escuin-Ordinas H, Rodriguez GA, et al. Interferon receptor signaling pathways regulating pd-l1 and pd-l2 expression. Cell Rep. 2017;19:1189–201.
Kim K, Skora AD, Li Z, Liu Q, Tam AJ, Blosser RL, et al. Eradication of metastatic mouse cancers resistant to immune checkpoint blockade by suppression of myeloid-derived cells. Proc Natl Acad Sci USA. 2014;111:11774–9.
Hellmann MD, Jänne PA, Opyrchal M, Hafez N, Raez LE, Gabrilovich DI, et al. Entinostat plus pembrolizumab in patients with metastatic nsclc previously treated with anti-pd-(l)1 therapy. Clin Cancer Res. 2021;27:1019–28.
Gao Y, He H, Li X, Zhang L, Xu W, Feng R, et al. Sintilimab (anti-pd-1 antibody) plus chidamide (histone deacetylase inhibitor) in relapsed or refractory extranodal natural killer t-cell lymphoma (scent): A phase ib/ii study. Signal Transduct Target Ther. 2024;9:121.
Acknowledgements
This research was supported by a grant from the ICKSH Research Project through the Korean Society of Hematology, Republic of Korea (ICKSH-2021-00), the Seoul National University Bundang Hospital Research Fund (09-2021-0001), and the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science and ICT (NRF-2022R1F1A1074801). We want to express our sincere gratitude to Prof. Norio Shimizu (Tokyo Medical and Dental University, Tokyo, Japan) for generously providing the SNK6 cell line used in this study.
Author information
Authors and Affiliations
Contributions
JYL and KJK designed the experiments, interpreted the data, and wrote the manuscript; JYL and JHP conceived the project and obtained funding; JYL, KJK, and JHP performed experiments, analyzed the data, prepared the figures, and drafted the manuscript; SAK, JOL, and SMB contributed in the analysis of results; WP, JS, MK, EHJ, KJS, JWK, SHK, JWK, YJK, KWL, JHK, and TMK. contributed to discussion and interpretation of results; and all authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (B-2104-680-303). The IRB waived the requirement for patient consent due to the retrospective nature of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, J.Y., Kim, KJ., Park, W. et al. Early growth response 1 as a key regulator of PD-L1 expression and immune evasion in extranodal NK/T-cell lymphoma. Blood Cancer J. 15, 108 (2025). https://doi.org/10.1038/s41408-025-01313-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41408-025-01313-w