Abstract
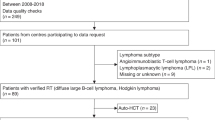
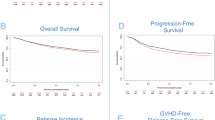
After allogeneic hematopoietic stem cell transplantation (allo-HSCT), the recurrence of recent thymic emigrants (RTE) and self-tolerant T cells indicate normalized thymic function. From 2008 to 2019, we retrospectively analyzed the RTE-reconstitution rate and the minimal time to reach normal age-specific first percentiles for CD31+CD45RA+CD4+T cells in 199 pediatric patients after allo-HSCT for various malignant and non-malignant diseases. The impact of clinically significant graft-versus-host disease (GvHD), age at transplantation, underlying disease and cumulative area under the curve of busulfan on RTE-reemergence was assessed in multivariable longitudinal analysis. RTE-reconstitution (coefficient −0.24, 95% CI −0.33 to −0.14, p < 0.001) was slowed down by GvHD and the time to reach P1 was significantly longer (Event Time Ratio 1.49, 95% CI 1.25 to 1.78, p < 0.001). Older age at transplantation was also associated with a slower RTE-reconstitution (coefficient −0.028, 95% CI −0.04 to −0.02, p < 0.001) and time to reach P1 was significantly longer (Event Time Ratio 1.03, 95% CI 1.02 to 1.05, p < 0.001). RTE-reconstitution velocity was not influenced by underlying disease or cumulative busulfan exposure. In summary, duration until thymic reactivation was independent of both conditioning intensity and underlying disease and was negatively influenced by older age and GvHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Code availability
The R code is available on request from corresponding author.
References
de Koning C, Plantinga M, Besseling P, Boelens JJ, Nierkens S. Immune reconstitution after allogeneic hematopoietic cell transplantation in children. Biol Blood Marrow Transpl. 2016;22:195–206.
Gress RE, Emerson SG, Drobyski WR. Immune reconstitution: how it should work, what’s broken, and why it matters. Biol Blood Marrow Transpl. 2010;16:S133–7.
Dvorak CC, Long-Boyle J, Dara J, Melton A, Shimano KA, Huang JN, et al. Low Exposure Busulfan Conditioning to Achieve Sufficient Multilineage Chimerism in Patients with Severe Combined Immunodeficiency. Biol Blood Marrow Transpl. 2019;25:1355–62.
Goldberg JD, Zheng J, Ratan R, Small TN, Lai K-C, Boulad F, et al. Early recovery of T-cell function predicts improved survival after T-cell depleted allogeneic transplant. Leuk Lymphoma. 2017;58:1859–71.
Duinhouwer LE, Beije N, van der Holt B, Rijken-Schelen A, Lamers CH, Somers J, et al. Impaired thymopoiesis predicts for a high risk of severe infections after reduced intensity conditioning without anti-thymocyte globulin in double umbilical cord blood transplantation. Bone Marrow Transpl. 2018;53:673–82.
de Koning C, Prockop S, van Roessel I, Kernan N, Klein E, Langenhorst J, et al. CD4+ T-cell reconstitution predicts survival outcomes after acute graft-versus-host-disease: a dual-center validation. Blood. 2021;137:848–55.
Berger M, Figari O, Bruno B, Raiola A, Dominietto A, Fiorone M, et al. Lymphocyte subsets recovery following allogeneic bone marrow transplantation (BMT): CD4+ cell count and transplant-related mortality. Bone Marrow Transplant. 2008;41:55–62.
Dekker L, de Koning C, Lindemans C, Nierkens S. Reconstitution of T cell subsets following allogeneic hematopoietic cell transplantation. Cancers. 2020;12:1974.
Moutuou MM, Pagé G, Zaid I, Lesage S, Guimond M. Restoring T cell homeostasis after allogeneic stem cell transplantation; principal limitations and future challenges. Front Immunol. 2018;9:1237.
Mellgren K, Nierop AFM, Abrahamsson J. Use of multivariate immune reconstitution patterns to describe immune reconstitution after allogeneic stem cell transplantation in children. Biol Blood Marrow Transpl. 2019;25:2045–53.
Flinn AM, Gennery AR. Treatment of Pediatric Acute Graft-versus-Host Disease—Lessons from Primary Immunodeficiency? Front Immunol. 2017;8. https://doi.org/10.3389/fimmu.2017.00328.
Ringhoffer S, Rojewski M, Dohner H, Bunjes D, Ringhoffer M. T-cell reconstitution after allogeneic stem cell transplantation: assessment by measurement of the sjTREC/ TREC ratio and thymic naive T cells. Haematologica. 2013;98:1600–8.
Bains I, Thiebaut R, Yates AJ, Callard R. Quantifying thymic export: combining models of naive T cell proliferation and TCR excision circle dynamics gives an explicit measure of thymic output. J Immunol. 2009;183:4329–36.
Junge S, Kloeckener-Gruissem B, Zufferey R, Keisker A, Salgo B, Fauchere J-C, et al. Correlation between recent thymic emigrants and CD31+ (PECAM-1) CD4+ T cells in normal individuals during aging and in lymphopenic children. Eur J Immunol. 2007;37:3270–80.
Kohler S, Wagner U, Pierer M, Kimmig S, Oppmann B, Möwes B, et al. Post-thymic in vivo proliferation of naive CD4+ T cells constrains the TCR repertoire in healthy human adults. Eur J Immunol. 2005;35:1987–94.
Satwani P, Cooper N, Rao K, Veys P, Amrolia P. Reduced intensity conditioning and allogeneic stem cell transplantation in childhood malignant and nonmalignant diseases. Bone Marrow Transpl. 2008;41:173–82.
Jiménez M, Martínez C, Ercilla G, Carreras E, Urbano-Ispízua Á, Aymerich M, et al. Reduced-intensity conditioning regimen preserves thymic function in the early period after hematopoietic stem cell transplantation. Exp Hematol. 2005;33:1240–8.
Larosa F, Marmier C, Robinet E, Ferrand C, Saas P, Deconinck E, et al. Peripheral T-cell expansion and low infection rate after reduced-intensity conditioning and allogeneic blood stem cell transplantation. Bone Marrow Transpl. 2005;35:859–68.
Lum SH, Hoenig M, Gennery AR, Slatter MA. Conditioning regimens for hematopoietic cell transplantation in primary immunodeficiency. Curr Allergy Asthma Rep. 2019;19:52.
Flinn AM, Roberts CF, Slatter MA, Skinner R, Robson H, Lawrence J, et al. Thymopoiesis following HSCT; a retrospective review comparing interventions for aGVHD in a pediatric cohort. Clin Immunol. 2018;193:33–7.
Hauri-Hohl MM, Keller MP, Gill J, Hafen K, Pachlatko E, Boulay T, et al. Donor T-cell alloreactivity against host thymic epithelium limits T-cell development after bone marrow transplantation. Blood. 2007;109:4080–8.
Felber M, Steward CG, Kentouche K, Fasth A, Wynn RF, Zeilhofer U, et al. Targeted busulfan-based reduced-intensity conditioning and HLA-matched HSCT cure hemophagocytic lymphohistiocytosis. Blood Adv. 2020;4:1998–2010.
Güngör T, Teira P, Slatter M, Stussi G, Stepensky P, Moshous D, et al. Reduced-intensity conditioning and HLA-matched haemopoietic stem-cell transplantation in patients with chronic granulomatous disease: a prospective multicentre study. Lancet. 2014;383:436–48.
Dougoud ST Age-specific percentiles of CD31 and CD127 receptor expression on variable T cell subsets in 74 healthy children from birth until adolescence. 2012.https://www.zora.uzh.ch/id/eprint/73955/ (accessed 7 April 2019).
Eberle P, Berger C, Junge S, Dougoud S, Büchel EV, Riegel M, et al. Persistent low thymic activity and non-cardiac mortality in children with chromosome 22q11·2 microdeletion and partial DiGeorge syndrome. Clin Exp Immunol. 2009;155:189–98.
Güngör T, Rufibach K, Dougoud S, Hauri-Hohl M, Oberholzer-Koechli S. Restoration and maintenance of naive CD31+ and CD31-CD45RA+RO-CD4+T-cell compartments after paediatric allogeneic haematopoietic stem cell transplantation. Physicians Abstracts. Bone Marrow Transplant 46, S35 (2011).
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transpl. 2015;21:389–401.e1.
Diggle P, Heagerty P, Liang K-Y, Zeger S. Analysis of Longitudinal Data. Second Edition. Oxford University Press: Oxford, New York, 2013.
Heinze G, Wallisch C, Dunkler D. Variable selection – A review and recommendations for the practicing statistician. Biom J. 2018;60:431–49.
Carroll KJ. On the use and utility of the Weibull model in the analysis of survival data. Control Clin Trials. 2003;24:682–701.
Köchli Oberholzer S. Short- and long-term immune reconstitution of naive CD31+ and CD31-CD45RA+RO-CD4+ T-cells in children after hematopoietic stem-cell transplantation (HSCT). 2012.https://www.zora.uzh.ch/id/eprint/75704/ (accessed 7 Apr2019).
Pinheiro, et al. nlme: Linear and Nonlinear Mixed Effects Models. 2020. https://CRAN.R-project.org/package=nlme (accessed 5 December 2020).
Therneau TM. (until 2009) TL original S->R port and R maintainer, Elizabeth A, Cynthia C. survival: Survival Analysis. 2021 https://CRAN.R-project.org/package=survival (accessed 9 April 2021).
Wickham H, Chang W, Henry L, Pedersen TL, Takahashi K, Wilke C, et al. ggplot2: Create Elegant Data Visualisations Using the Grammar of Graphics. 2020.https://CRAN.R-project.org/package=ggplot2 (accessed 5 December 2020).
Sarkar D Lattice: Multivariate Data Visualization with R. Springer-Verlag: New York, 2008 https://doi.org/10.1007/978-0-387-75969-2.
Devine SM, Adkins DR, Khoury H, Brown RA, Vij R, Blum W, et al. Recent advances in allogeneic hematopoietic stem-cell transplantation. J Lab Clin Med. 2003;141:7–32.
Fallen PR, McGreavey L, Madrigal JA, Potter M, Ethell M, Prentice HG, et al. Factors affecting reconstitution of the T cell compartment in allogeneic haematopoietic cell transplant recipients. Bone Marrow Transpl. 2003;32:1001–14.
Geddes M, Storek J. Immune reconstitution following hematopoietic stem-cell transplantation. Best Pr Res Clin Haematol. 2007;20:329–48.
Admiraal R, Lindemans CA, van Kesteren C, Bierings MB, Versluijs AB, Nierkens S, et al. Excellent T-cell reconstitution and survival depend on low ATG exposure after pediatric cord blood transplantation. Blood. 2016;128:2734–41.
Clave E, Busson M, Douay C, Peffault de Latour R, Berrou J, Rabian C, et al. Acute graft-versus-host disease transiently impairs thymic output in young patients after allogeneic hematopoietic stem cell transplantation. Blood. 2009;113:6477–84.
Clave E, Lisini D, Douay C, Giorgiani G, Busson M, Zecca M, et al. Thymic function recovery after unrelated donor cord blood or T-cell depleted HLA-haploidentical stem cell transplantation correlates with leukemia relapse. Front Immunol. 2013;4. https://doi.org/10.3389/fimmu.2013.00054.
Prelog M, Keller M, Geiger R, Brandstätter A, Würzner R, Schweigmann U, et al. Thymectomy in early childhood: significant alterations of the CD4+CD45RA+CD62L+ T cell compartment in later life. Clin Immunol. 2009;130:123–32.
Toubert A, Glauzy S, Douay C, Clave E. Thymus and immune reconstitution after allogeneic hematopoietic stem cell transplantation in humans: never say never again. Tissue Antigens. 2012;79:83–9.
Toubert A, Einsele H. How to improve immune reconstitution in allogeneic hematopoietic stem cell transplantation? Frontiers SA Media, 2015 https://doi.org/10.3389/978-2-88919-491-9.
Bejanyan N, Brunstein CG, Cao Q, Lazaryan A, Luo X, Curtsinger J, et al. Delayed immune reconstitution after allogeneic transplantation increases the risks of mortality and chronic GVHD. Blood Adv. 2018;2:909–22.
Boelens JJ, Hosszu KK, Nierkens S. Immune monitoring after allogeneic hematopoietic cell transplantation: toward practical guidelines and standardization. Front Pediatr. 2020;8:454.
Neven B, Leroy S, Decaluwe H, Le Deist F, Picard C, Moshous D, et al. Long-term outcome after hematopoietic stem cell transplantation of a single-center cohort of 90 patients with severe combined immunodeficiency. Blood. 2009;113:4114–24.
Kohler S, Thiel A. Life after the thymus: CD31+ and CD31- human naive CD4+ T-cell subsets. Blood. 2009;113:769–74.
van den Broek T, Borghans JAM, van Wijk F. The full spectrum of human naive T cells. Nat Rev Immunol. 2018;18:363–73.
Rajasekar R, Mathews V, Lakshmi KM, George B, Viswabandya A, Chandy M, et al. Cellular immune reconstitution and its impact on clinical outcome in children with β Thalassemia major undergoing a matched related myeloablative allogeneic bone marrow transplant. Biol Blood Marrow Transpl. 2009;15:597–609.
Eyrich M, Wollny G, Tzaribaschev N, Dietz K, Brügger D, Bader P, et al. Onset of thymic recovery and plateau of thymic output are differentially regulated after stem cell transplantation in children. Biol Blood Marrow Transpl. 2005;11:194–205.
Wiegering V, Eyrich M, Winkler B, Schlegel PG. Comparison of immune reconstitution after allogeneic vs. autologous stem cell transplantation in 182 pediatric recipients. Pediatr Hematol Oncol J. 2017;2:2–6.
Bhatt ST, Bednarski JJ, Berg J, Trinkaus K, Murray L, Hayashi R, et al. Immune reconstitution and infection patterns after early alemtuzumab and reduced intensity transplantation for nonmalignant disorders in pediatric patients. Biol Blood Marrow Transpl. 2019;25:556–61.
Lankester AC, Albert MH, Booth C, Gennery AR, Güngör T, Hönig M, et al. EBMT/ESID inborn errors working party guidelines for hematopoietic stem cell transplantation for inborn errors of immunity. Bone Marrow Transpl. 2021;56:2052–62.
Peters C, Dalle J-H, Locatelli F, Poetschger U, Sedlacek P, Buechner J, et al. Total body irradiation or chemotherapy conditioning in childhood ALL: a multinational, randomized, noninferiority phase III study. J Clin Oncol. 2021;39:295–307.
Acknowledgements
The authors thank Maja Rutishauser, senior laboratory technician, who played a major role implementing the flowcytometry analyses and the percentiles for CD4+CD31+ T-cells into the routine laboratory diagnostics at University Children’s Hospital Zürich, Switzerland.
Funding
DD received a grant for this study from the Children’s Research Center, University Children’s Hospital Zürich, University of Zürich, Zürich, Switzerland. MHH is supported by the Prof. Max Cloëtta Foundation.
Author information
Authors and Affiliations
Contributions
DD, TG, MH, SO and SD conceived and designed the study, analyzed the data and wrote the manuscript. KP and LH performed the statistical analysis and reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was granted by the Ethics Committee of Canton Zürich, Switzerland (2017-02040). Informed consent was obtained from all study participants transplanted after 01.01.2014. For patients transplanted before 01.01.2014 the informed consent was waived by the Ethics Committee of Canton Zürich, Switzerland.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Drozdov, D., Petermann, K., Dougoud, S. et al. Dynamics of recent thymic emigrants in pediatric recipients of allogeneic hematopoetic stem cell transplantation. Bone Marrow Transplant 57, 620–626 (2022). https://doi.org/10.1038/s41409-022-01594-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-022-01594-w
This article is cited by
-
Zinc as a therapeutic adjunct: enhancing t-cell reconstitution in hematopoietic stem cell transplant recipients—a double-blind clinical study
BMC Immunology (2025)
-
Impact of CAR T cell therapy on thymus size in children and young adults with acute lymphoblastic leukemia
Scientific Reports (2025)
-
Measuring thymic output across the human lifespan: a critical challenge in laboratory medicine
GeroScience (2025)
-
Evaluating Pediatric Reference Ranges for Extended Immunophenotyping from a Finnish Cohort against Published References
Journal of Clinical Immunology (2025)
-
Early-life thymectomy leads to an increase of granzyme-producing γδ T cells in children with congenital heart disease
Nature Communications (2024)