Abstract
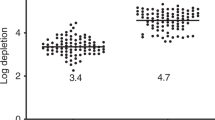
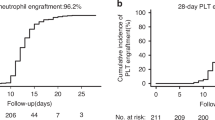
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) aims to cure patients without inducing severe graft-versus-host disease (GVHD) or relapse. In prospective studies of mostly pediatric patients with haploidentical donors, ex vivo αβTCR/CD19 depletion has shown to have low incidences of GVHD, but data for adults with matched related (MRD) or unrelated donors (MUD) remain limited. We analyzed the outcomes of recipients who received a myeloablative regimen plus ATG, followed by an αβTCR/CD19-depleted allograft (cohort D+ATG (n = 122)), and compared outcomes to T cell-replete cohorts (cohort R (N = 60)); without ATG; R+ATG = with ATG (N = 129) in a single-center retrospective analysis. In D+ATG, the incidence of aGVHD grade III–IV was 7%, compared to 13% in R and 16% in R+ATG (p = 0.09). Extensive cGVHD was reduced from 23% in R and 10% in R+ATG to 2% in D+ATG (p < 0.001). The reduced incidence of cGVHD led to a superior GVHD-relapse-free survival (GRFS) of 56.7% in D+ATG versus 36.7% in R and 42.8% in R+ATG (p = 0.03) at 2 years. In conclusion, the combination of myeloablative conditioning, ATG, and ex vivo αβTCR/CD19 depletion appears to be a promising approach to enhance GRFS in adult patients up to 75 years of age undergoing allo-HSCT.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from EBMT the registry, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the corresponding author.
References
Korngold R, Sprent J. Lethal graft-versus-host disease after bone marrow transplantation across minor histocompatibility barriers in mice. Prevention by removing mature T cells from marrow. J Exp Med. 1978;148:1687–98.
Shlomchik WD. Graft-versus-host disease. Nat Rev Immunol. 2007;7:340–52.
Penack O, Marchetti M, Aljurf M, Arat M, Bonifazi F, Duarte RF, et al. Prophylaxis and management of graft-versus-host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2024;2:e147-e159.
Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR, et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol. 2009;10:855–64.
Mohty M, Labopin M, Balere ML, Socie G, Milpied N, Tabrizi R, et al. Antithymocyte globulins and chronic graft-vs-host disease after myeloablative allogeneic stem cell transplantation from HLA-matched unrelated donors: a report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Leukemia. 2010;24:1867–74.
Pidala J, Tomblyn M, Nishihori T, Ayala E, Field T, Fernandez H, et al. ATG prevents severe acute graft-versus-host disease in mismatched unrelated donor hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2011;17:1237–44.
Socie G, Schmoor C, Bethge WA, Ottinger HD, Stelljes M, Zander AR, et al. Chronic graft-versus-host disease: long-term results from a randomized trial on graft-versus-host disease prophylaxis with or without anti-T-cell globulin ATG-Fresenius. Blood. 2011;117:6375–82.
Bonifazi F, Rubio MT, Bacigalupo A, Boelens JJ, Finke J, Greinix H, et al. Rabbit ATG/ATLG in preventing graft-versus-host disease after allogeneic stem cell transplantation: consensus-based recommendations by an international expert panel. Bone Marrow Transplant. 2020;55:1093–102.
Penack O, Abouqateb M, Peczynski C, Boreland W, Kroger N, Stelljes M, et al. ATG or post-transplant cyclophosphamide to prevent GVHD in matched unrelated stem cell transplantation? Leukemia. 2024;38:1156–63.
Berger M, Lanino E, Cesaro S, Zecca M, Vassallo E, Faraci M, et al. Feasibility and outcome of haploidentical hematopoietic stem cell transplantation with post-transplant high-dose cyclophosphamide for children and adolescents with hematologic malignancies: an AIEOP-GITMO Retrospective Multicenter Study. Biol Blood Marrow Transplant. 2016;22:902–9.
Mussetti A, Greco R, Peccatori J, Corradini P. Post-transplant cyclophosphamide, a promising anti-graft versus host disease prophylaxis: where do we stand? Expert Rev Hematol. 2017;10:479–92.
Uygun V, Karasu G, Daloglu H, Ozturkmen S, Caki Kilic S, Hazar V, et al. Haploidentical hematopoietic stem cell transplantation with post-transplant high-dose cyclophosphamide in high-risk children: a single-center study. Pediatr Transplant. 2019;23:e13546.
Sharma A, Rastogi N, Chatterjee G, Kapoor R, Nivargi S, Yadav SP. Haploidentical stem cell transplantation with post-transplant cyclophosphamide for pediatric acute leukemia is safe and effective. J Pediatr Hematol Oncol. 2021;43:e1033–e6.
Broers AEC, de Jong CN, Bakunina K, Hazenberg MD, van Marwijk Kooy M, de Groot MR, et al. Posttransplant cyclophosphamide for prevention of graft-versus-host disease: results of the prospective randomized HOVON-96 trial. Blood Adv. 2022;6:3378–85.
Bolanos-Meade J, Hamadani M, Wu J, Al Malki MM, Martens MJ, Runaas L, et al. Post-transplantation cyclophosphamide-based graft-versus-host disease prophylaxis. N Engl J Med. 2023;388:2338–48.
Finazzi MC, Boschini C, Craddock C, Rambaldi A, Ward J, Malladi RK. Characteristics of graft-versus-host disease occurring after alemtuzumab-containing allogeneic stem cell transplants: incidence, organ involvement, risk factors and survival. Br J Haematol. 2020;188:550–9.
de Witte MA, Mooyaart JE, Hoogenboom JD, Chabannon C, Malard F, Ruggeri A, et al. Activity of ex vivo graft and DLI Engineering within the last decade increases, a survey from the EBMT Cellular Therapy & Immunobiology Working Party. Bone Marrow Transplant. 2023;58:719–22.
Nijssen K, Westinga K, Stuut A, Janssen A, van Rhenen A, van der Wagen L, et al. Graft engineering: how long can you wait, how low can you go, and pandemic readiness. Bone Marrow Transplant. 2023;58:820–2.
Bertaina A, Romano M, Rutella S, Palumbo G, Pagliara D, Ceccarelli S, et al. HLA haploidentical stem cell transplantation after removal of αβ+ T lymphocytes and B lymphocytes is an effective treatment for children with life-threatening, non-malignant disorders. Blood. 2012;120:2018.
Locatelli F, Merli P, Pagliara D, Li Pira G, Falco M, Pende D, et al. Outcome of children with acute leukemia given HLA-haploidentical HSCT after alphabeta T-cell and B-cell depletion. Blood. 2017;130:677–85.
Bethge WA, Eyrich M, Mielke S, Meisel R, Niederwieser D, Schlegel PG, et al. Results of a multicenter phase I/II trial of TCRalphabeta and CD19-depleted haploidentical hematopoietic stem cell transplantation for adult and pediatric patients. Bone Marrow Transplant. 2022;57:423–30.
Leahy AB, Li Y, Talano JA, Elgarten CW, Seif AE, Wang Y, et al. Unrelated donor alpha/beta T cell- and B cell-depleted HSCT for the treatment of pediatric acute leukemia. Blood Adv. 2022;6:1175–85.
de Witte MA, Janssen A, Nijssen K, Karaiskaki F, Swanenberg L, van Rhenen A, et al. alphabeta T-cell graft depletion for allogeneic HSCT in adults with hematological malignancies. Blood Adv. 2021;5:240–9.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5675–87.
Chaleff S, Otto M, Barfield RC, Leimig T, Iyengar R, Martin J, et al. A large-scale method for the selective depletion of alphabeta T lymphocytes from PBSC for allogeneic transplantation. Cytotherapy. 2007;9:746–54.
Li Pira G, Malaspina D, Girolami E, Biagini S, Cicchetti E, Conflitti G, et al. Selective depletion of alphabeta T cells and B cells for human leukocyte antigen-haploidentical hematopoietic stem cell transplantation. A three-year follow-up of procedure efficiency. Biol Blood Marrow Transplant. 2016;22:2056–64.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Carreras E, Dufour C, Mohty M, Kroger N, editors. The EBMT handbook: hematopoietic stem cell transplantation and cellular therapies. 7th ed. Cham: Springer; 2019.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone marrow Transplant. 1995;15:825–8.
Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2003;9:215–33.
Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood. 2016;127:2427–38.
Fujimoto A, Suzuki R. Epstein-Barr virus-associated post-transplant lymphoproliferative disorders after hematopoietic stem cell transplantation: pathogenesis, risk factors and clinical outcomes. Cancers. 2020;12:328–51.
Kroger N, Solano C, Wolschke C, Bandini G, Patriarca F, Pini M, et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N Engl J Med. 2016;374:43–53.
de Witte M, Daenen LGM, van der Wagen L, van Rhenen A, Raymakers R, Westinga K, et al. Allogeneic stem cell transplantation platforms with ex vivo and in vivo immune manipulations: count and adjust. Hemasphere. 2021;5:e580.
Luznik L, Pasquini MC, Logan B, Soiffer RJ, Wu J, Devine SM, et al. Randomized phase III BMT CTN trial of calcineurin inhibitor-free chronic graft-versus-host disease interventions in myeloablative hematopoietic cell transplantation for hematologic malignancies. J Clin Oncol. 2021;40:356–68.
Lum SH, Albert MH, Gilbert P, Sirait T, Algeri M, Muratori R, et al. Outcomes of HLA-mismatched HSCT with TCRalphabeta/CD19 depletion or post-HSCT cyclophosphamide for inborn errors of immunity. Blood. 2024;144:565–80.
Marty FM, Ljungman P, Chemaly RF, Maertens J, Dadwal SS, Duarte RF, et al. Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N Engl J Med. 2017;377:2433–44.
Marzolini MAV, Mehra V, Thomson KJ, Tholouli E, Bloor AJC, Parker A, et al. Letermovir prophylaxis in T-cell-depleted transplants: breakthrough and rebound infections in the postmarketing setting. Blood Adv. 2021;5:4500–3.
Russo D, Schmitt M, Pilorge S, Stelljes M, Kawakita T, Teal VL, et al. Efficacy and safety of extended duration letermovir prophylaxis in recipients of haematopoietic stem-cell transplantation at risk of cytomegalovirus infection: a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Haematol. 2024;11:e127–e35.
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transplant. 2020;55:1114–25.
Pagliuca S, Schmid C, Santoro N, Simonetta F, Battipaglia G, Guillaume T, et al. Donor lymphocyte infusion after allogeneic haematopoietic cell transplantation for haematological malignancies: basic considerations and best practice recommendations from the EBMT. Lancet Haematol. 2024;11:e448–58.
Author information
Authors and Affiliations
Contributions
MdW and JK were responsible for the conception and design of the study. MdW and JK were funded for the study. LvdW, AvR, LvH, AJ, HK, RF, JK, and MdW actively managed the patients. AS, CN, FV, IB, FVL, HK, RF, HJP and KW collected the data. AS, CN, IB, and FV had full access to and verified the underlying data. AS, CN, JD, JK, and MdW contributed to data analysis and interpretation. AS, CN, JD, JK, and MdW wrote the original draft of the manuscript. AS and CN prepared the figures. AS and MdW were responsible for the submission of the manuscript. All authors were responsible for the critical revision of the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
JK is the inventor of multiple patents dealing with gdTCRs, ligands, and isolation strategies of engineered immune cells. JK is cofounder and shareholder of Gadeta (www.gadeta.nl). JK received research, advisor, and clinical study support from Miltenyi Biotech. JK received further research support from Novartis and Gadeta.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stuut, A.H.G., Nijssen, C., van der Wagen, L. et al. Improved GVHD-free and relapse-free survival after ex vivo αβTCR and CD19 depleted allogeneic HSCT compared to T cell replete HSCT. Bone Marrow Transplant 60, 673–681 (2025). https://doi.org/10.1038/s41409-025-02538-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02538-w