Abstract
Objectives
Contributions of TGFβ to cancer progression are well documented. However, plasma TGFβ levels often do not correlate with clinicopathological data. We examine the role of TGFβ carried in exosomes isolated from murine and human plasma as a contributor to disease progression in head and neck squamous cell carcinoma (HNSCC).
Materials and methods
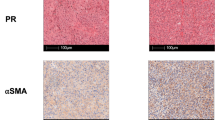
The 4-nitroquinoline-1-oxide (4-NQO) mouse model was used to study changes in TGFβ expression levels during oral carcinogenesis. In human HNSCC, TGFβ and Smad3 protein expression levels and TGFB1 gene expression were determined. Soluble TGFβ levels were evaluated by ELISA and TGFβ bioassays. Exosomes were isolated from plasma using size exclusion chromatography, and TGFβ content was quantified using bioassays and bioprinted microarrays.
Results
During 4-NQO carcinogenesis, TGFβ levels in tumour tissues and in serum increased as the tumour progressed. The TGFβ content of circulating exosomes also increased. In HNSCC patients, TGFβ, Smad3 and TGFB1 were overexpressed in tumour tissues and correlated with increased soluble TGFβ levels. Neither TGFβ expression in tumours nor levels of soluble TGFβ correlated with clinicopathological data or survival. Only exosome-associated TGFβ reflected tumour progression and correlated with tumour size.
Conclusions
Circulating TGFβ+ exosomes in the plasma of patients with HNSCC emerge as potential non-invasive biomarkers of disease progression in HNSCC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, TLW.
References
Batlle E, Massagué J. Transforming growth factor-β signaling in immunity and cancer. Immunity. 2019;50:924–40.
Tuxhorn JA, McAlhany SJ, Yang F, Dang TD, Rowley DR. Inhibition of transforming growth factor-β activity decreases angiogenesis in a human prostate cancer-reactive stroma xenograft model. Cancer Res. 2002;62:6021–5.
Todorović-Raković N, Milovanović J, Nikolić-Vukosavljević D. TGF‑β and its coreceptors in cancerogenesis: an overview. Biomark Med. 2011;5:855–63.
Colak S, Dijke P. Targeting TGF-β signaling in cancer. Trends Cancer. 2017;3:56–71.
Hinck AP, Mueller TD, Springer TA. Structural biology and evolution of the TGF-β family. Cold Spring Harb Perspect Biol. 2016;8:1–51.
Blobe G, Schiemann W, Lodish H. Role of transforming growth factor β in human disease. N Engl J Med. 2002;342:1350–8.
Szczepanski MJ, Szajnik M, Welsh A, Whiteside TL, Boyiadzis M. Blast-derived microvesicles in sera from patients with acute myeloid leukemia suppress natural killer cell function via membrane-associated transforming growth factor-beta1. Haematologica. 2011;96:1302–9.
Hong C-S, Muller L, Whiteside TL, Boyiadzis M. Plasma exosomes as markers of therapeutic response in patients with acute myeloid leukemia. Front Immunol. 2014;5:160.
Ludwig S, Floros T, Theodoraki M-N, Hong C-S, Jackson E, Lang S, et al. Suppression of lymphocyte functions by plasma exosomes correlates with disease activity in patients with head and neck cancer. Clin Cancer Res. 2017;23:4843–54.
Xiao H, Wong DTW. Proteomic analysis of microvesicles in human saliva by gel electrophoresis with liquid chromatography-mass spectrometry. Anal Chim Acta. 2012;723:61–7.
Sharma P, Diergaarde B, Ferrone S, Kirkwood JM, Whiteside TL. Melanoma cell-derived exosomes in plasma of melanoma patients suppress functions of immune effector cells. Sci Rep. 2020;10:1–11.
Hoshino A, Kim HS, Bojmar L, Gyan KE, Cioffi M, Hernandez J, et al. Extracellular vesicle and particle biomarkers define multiple human cancers. Cell. 2020;182:1044–61.e18.
Razzo BM, Ludwig N, Hong C, Sharma P, Fabian KP, Fecek RJ, et al. Tumor-derived exosomes promote carcinogenesis of murine oral squamous cell carcinoma. Carcinogenesis. 2019;41:625–33.
Webber J, Steadman R, Mason MD, Tabi Z, Clayton A. Cancer exosomes trigger fibroblast to myofibroblast differentiation. Cancer Res. 2010;70:9621–30.
Costa-silva B, Aiello NM, Ocean AJ, Singh S, Thakur BK, Becker A, et al. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat Cell Biol. 2015;17:816–26.
Ludwig N, Wieteska Ł, Hinck CS, Yerneni SS, Azambuja JH, Bauer RJ, et al. Novel TGFβ inhibitors ameliorate oral squamous cell carcinoma progression and improve the antitumor immune response of anti–PD-L1 immunotherapy. Mol Cancer Ther. 2021;20:1102–11.
Tesseur I, Zou K, Berber E, Zhang H, Wyss-Coray T. Highly sensitive and specific bioassay for measuring bioactive TGF-β. BMC Cell Biol. 2006;7:1–7.
Ludwig N, Hong C-S, Ludwig S, Azambuja JH, Sharma P, Theodoraki M-N, et al. Isolation and analysis of tumor-derived exosomes. Curr Protoc Immunol. 2019;127:e91.
Théry C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD, Andriantsitohaina R, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2019;8:1535750.
Huang T, Hinck AP. Production, isolation, and structural analysis of ligands and receptors of the TGF-β superfamily. Methods Mol Biol. 2016;1344:63–92.
Ludwig N, Gillespie D, Reichert T, Jackson E, Whiteside TL. Purine metabolites in tumor-derived exosomes may facilitate immune escape of head and neck squamous cell carcinoma. Cancers. 2020;12:1602.
Ludwig N, Whiteside TL, Reichert TE. Challenges in exosome isolation and analysis in health and disease. Int J Mol Sci. 2019;20:4684.
Ludwig N, Yerneni SS, Razzo BM, Whiteside TL. Exosomes from HNSCC promote angiogenesis through reprogramming of endothelial cells. Mol Cancer Res. 2018;16:1798–808.
Koliha N, Heider U, Ozimkowski T, Wiemann M, Bosio A, Wild S. Melanoma affects the composition of blood cell-derived extracellular vesicles. Front Immunol. 2016;7:1–12.
Liu L, Zhang Z, Zhou L, Hu L, Yin C, Qing D, et al. Cancer associated fibroblasts-derived exosomes contribute to radioresistance through promoting colorectal cancer stem cells phenotype. Exp Cell Res. 2020;391:111956.
Li M, Xin Y, Liu M, Yu K. Platelet-derived exosomes promote the epithelial–mesenchymal transition in MCF7 cells. Mol Cell Toxicol. 2022;18:31–7.
Biswas S, Mandal G, Chowdhury S, Purohit S, Payne K, Anadon C, et al. Exosomes produced by mesenchymal stem cells drive differentiation of myeloid cells into immunosuppressive M2-polarized macrophages in breast cancer. J Immunol. 2019;203:3447–60.
Zhu QJ, Zhu M, Xu XX, Meng XM, Wu YG. Exosomes from high glucose–treated macrophages activate glomerular mesangial cells via TGF-β1/Smad3 pathway in vivo and in vitro. FASEB J. 2019;33:9279–90.
Karolczak K, Watala C. Blood platelets as an important but underrated circulating source of TGFβ. Int J Mol Sci. 2021;22:4492.
Ko SY, Lee WJ, Kenny HA, Dang LH, Ellis LM, Jonasch E, et al. Cancer-derived small extracellular vesicles promote angiogenesis by heparin-bound, bevacizumab-insensitive VEGF, independent of vesicle uptake. Commun Biol. 2019;2:1–17.
Sung BH, Weaver AM. Exosome secretion promotes chemotaxis of cancer cells. Cell Adhes Migr. 2017;11:187–95.
Jablonska J, Rist M, Spyra I, Tengler L, Domnich M, Kansy B, et al. Evaluation of immunoregulatory biomarkers on plasma small extracellular vesicles for disease progression and early therapeutic response in head and neck cancer. Cells. 2022;11:902.
Ludwig N, Yerneni S, Azambuja J, Gillespie D, Menshikova E, Jackson E, et al. Tumor-derived exosomes promote angiogenesis via adenosine A2B receptor signaling. Angiogenesis. 2020;23:599–610.
Acknowledgements
The authors would like to thank late Professor Lee E. Weiss (The Robotics Institute, Carnegie Mellon University, Pittsburgh, PA) for building the custom inkjet bioprinter that enabled the fabrication of TβR microarrays, and Dr. Tomasz Szafarowski (Department of Otolaryngology, Faculty of Dental Medicine, Medical University of Warsaw) for collecting tissue samples.
Funding
This work was supported by National Institutes of Health grants R01-CA 168628 and U01-DE029759 to TLW. NL was supported by the Leopoldina Fellowships LPDS 2017-12 and LPDR 2019-02 from the German National Academy of Sciences Leopoldina and by the Walter Schulz Foundation. AG was supported by the Medical University of Warsaw MB/M/48[79]#. MJS was supported by National Science Centre, Poland UMO-2017/26/M/NZ5/00877#.
Author information
Authors and Affiliations
Contributions
Conceptualisation: NL, SSY and TLW; formal analysis: NL, SSY, MH, MJS, AG and TJ; funding acquisition: NL, MJS, AG and TLW; investigation: NL, SSY, MH, MJS, AG, TJ and CSH; methodology: NL, SSY and TLW; project administration: NL, MJS, GS, JT, SS, JKM, PGC, TER, APH and TLW; resources: NL, SSY, MJS, WK, PGC, TER, APH and TLW; supervision: NL, MJS, GS, PGC, TER, APH and TLW; visualisation: NL, SSY, MJS and AG; writing—original draft: NL; writing—review & editing: NL, SSY, MH, MJS, AG, WK, TJ, GS, JT, SS, JKM, CSH, PGC, TER, APH and TLW.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee at the Medical University of Warsaw (#AKBE/50/12) and the Institutional Review Board (IRB) of the University of Pittsburgh (IRB approvals #0403105 and #0506140).
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ludwig, N., Yerneni, S.S., Harasymczuk, M. et al. TGFβ carrying exosomes in plasma: potential biomarkers of cancer progression in patients with head and neck squamous cell carcinoma. Br J Cancer 128, 1733–1741 (2023). https://doi.org/10.1038/s41416-023-02184-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-023-02184-3
This article is cited by
-
Expression of vesiculation-related genes is associated with a tumor-promoting microenvironment: a pan-cancer analysis
Clinical and Translational Oncology (2025)
-
Emerging roles of exosomes in oral diseases progression
International Journal of Oral Science (2024)
-
Does circulating tumor DNA apply as a reliable biomarker for the diagnosis and prognosis of head and neck squamous cell carcinoma?
Discover Oncology (2024)
-
Small extracellular vesicle TGF-β in cancer progression and immune evasion
Cancer Gene Therapy (2023)