Abstract
Background
Kidney transplant (KT) patients have higher risks of developing de novo colorectal cancer (CRC) compared to the general population. However, there is still a knowledge gap in their clinical characteristics, as most single- or multi-center efforts are underpowered and lack generalizability.
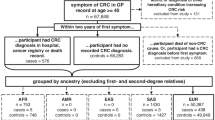
Methods
PubMed, Web of Science, Cochrane CENTRAL, and Scopus databases were queried for studies published until July 22nd, 2024. Studies reporting the clinicopathologic characteristics and outcomes of de novo CRC among KT recipients were included.
Results
There were 49 articles included involving 1855 KT patients who developed CRC. The mean time from transplantation to CRC diagnosis was 8·7 years (95%CI 7·2, 10·3 years; I2 = 98·3%). De novo CRC was most commonly located in the ascending colon (43·6%; 95%CI 29·5%, 58·9%; I2 = 55·3%), and 37·1% had advanced CRC at diagnosis (95%CI 22·3%, 54·8%; I2 = 64·1%). Although 68·8% underwent curative intent treatment (95%CI 45·4%, 85·4%; I2 = 65·4%), pooled 5-year survival rate was 31·8% (95%CI 10·5%, 65·1%; I2 = 82·5%).
Conclusions
De novo CRC was diagnosed in under 10 years after KT, and nearly 40% of patients already have advanced stage disease at diagnosis. The pooled rate of 5-year survival was 31.8%. However, there was wide heterogeneity between studies and further research is required. PROSPERO Registration: CRD42023415767.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data used in the results of this systematic review and meta-analysis, its study protocol, and statistical analysis plan will be made available following publication upon request. Please contact the corresponding author via email with a study proposal (e.g., statistical plan, study protocol) and details regarding how the data will be used.
References
Jager KJ, Kovesdy C, Langham R, Rosenberg M, Jha V, Zoccali C. A single number for advocacy and communication—worldwide more than 850 million individuals have kidney diseases. Nephrol Dialysis Transplant. 2019;34:1803–5.
Revuelta I, Moya-Rull D, García-Herrera A, Rovira J, Ayala De La Peña F, Misiego A, et al. Role of oncogenic pathways and KRAS/BRAF mutations in the behavior of colon adenocarcinoma in renal transplant patients. Transplantation. 2012;93:509–17.
Kwon JH, Koh SJ, Kim JY, Kim JW, Lee KL, Kim BG, et al. Prevalence of advanced colorectal neoplasm after kidney transplantation: surveillance based on the results of screening colonoscopy. Dig Dis Sci. 2015;60:1761–9.
Prenner S, Levitsky J. Comprehensive review on colorectal cancer and transplant. Am J Transplant. 2017;17:2761–74.
Jin F, Vajdic CM, Poynten IM, McGee-Avila JK, Castle PE, Grulich AE. Cancer risk in people living with HIV and solid organ transplant recipients: a systematic review and meta-analysis. Lancet Oncol. 2024;25:933–44.
Safaeian M, Robbins HA, Berndt SI, Lynch CF, Fraumeni JF, Engels EA. Risk of colorectal cancer after solid organ transplantation in the United States. Am J Transplant. 2016;16:960–7.
Au E, Wong G, Chapman JR. Cancer in kidney transplant recipients. Nat Rev Nephrol. 2018;14:508–20.
Acuna SA, Huang JW, Scott AL, Micic S, Daly C, Brezden-Masley C, et al. Cancer screening recommendations for solid organ transplant recipients: a systematic review of clinical practice guidelines. Am J Transplant. 2017;17:103–14.
Kasiske BL, Vazquez MA, Harmon WE, Brown RS, Danovitch GM, Gaston RS, et al. Recommendations for the outpatient surveillance of renal transplant recipients. J Am Soc Nephrol. 2000;11:S1.
Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2023. CA A Cancer J Clin. 2023;73:233–54.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. Available from: https://www.bmj.com/content/372/bmj.n71.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–12.
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2024. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Shi J, Luo D, Weng H, Zeng XT, Lin L, Chu H. et al. Optimally estimating the sample standard deviation from the five-number summary. Res Synth Methods. 2020;11:641–54.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805.
Kim JY, Ju MK, Kim MS, Kim NK, Sohn SK, Kim SI, et al. Clinical characteristics and treatment outcomes of colorectal cancer in renal transplant recipients in Korea. Yonsei Med J. 2011;52:454.
Park JM, Choi M‐G, Kim SW, Chung I‐S, Yang CW, Kim YS, et al. Increased incidence of colorectal malignancies in renal transplant recipients: a case control study. Am J Transplant. 2010;10:2043–50.
Dobies A, Renke M, Wołyniec W, Palenicek L, Januszczyk J, Król E, et al. Gastrointestinal pathologies in patients after successful renal transplantation—a pilot study. Transplant Proc. 2016;48:1566–9.
Heo J, Noh OK, Oh YT, Chun M, Kim L. Cancer risk after renal transplantation in South Korea: a nationwide population-based study. BMC Nephrol. 2018;19:311.
Friman TK, Jäämaa‐Holmberg S, Åberg F, Helanterä I, Halme M, Pentikäinen MO, et al. Cancer risk and mortality after solid organ transplantation: a population‐based 30‐year cohort study in Finland. Int J Cancer. 2022;150:1779–91.
Murray SL, O’Leary E, De Bhailís ÁM, Deady S, Daly FE, O’Kelly P, et al. Cancer survival in kidney transplant recipients in Ireland. Nephrol Dial Transplant. 2020;35:1802–10.
Blosser CD, Haber G, Engels EA. Changes in cancer incidence and outcomes among kidney transplant recipients in the United States over a thirty-year period. Kidney Int. 2021;99:1430–8.
Kim M, Kim CW, Hwang S, Kim YH, Lee JL, Yoon YS, et al. Characteristics and prognosis of colorectal cancer after liver or kidney transplantation. World J Surg. 2021;45:3206–13.
Papaconstantinou HT, Sklow B, Hanaway MJ, Gross TG, Beebe TM, Trofe J, et al. Characteristics and survival patterns of solid organ transplant patients developing de novo colon and rectal cancer. Dis Colon Rectum. 2004;47:1898–903.
Privitera F, Gioco R, Civit AI, Corona D, Cremona S, Puzzo L, et al. Colorectal cancer after kidney transplantation: a screening colonoscopy case-control study. Biomedicines. 2021;9:937.
Ho H, Russ G, Stephens J, Rieger N. Colorectal cancer in patients with chronic renal failure: the effect of dialysis or renal transplantation. Colorectal Dis. 2002;4:193–6.
Collett D, Mumford L, Banner NR, Neuberger J, Watson C. Comparison of the Incidence of Malignancy in Recipients of Different Types of Organ: A UK Registry Audit. Am J Transplant. 2010;10:1889–96.
Wang HE, Liao YC, Hu JM, Wu WC, Chou WY, Chen YC, et al. Correlation between kidney transplantation and colorectal cancer in hemodialysis patients: a nationwide, retrospective, population-based cohort study. BMC Cancer. 2019;19:1120.
Mazzucotelli V, Piselli P, Verdirosi D, Cimaglia C, Cancarini G, Serraino D, et al. De novo cancer in patients on dialysis and after renal transplantation: north-western Italy, 1997–2012. J Nephrol. 2017;30:851–7.
Kim B, Kang M, Kim Y, Lee HS, Kim B, Lee JJ, et al. De novo cancer incidence after kidney transplantation in South Korea from 2002 to 2017. JCM. 2021;10:3530.
Gioco R, Corona D, Agodi A, Privitera F, Barchitta M, Giaquinta A, et al. De novo cancer incidence and prognosis after kidney transplantation: a single center analysis. Transplant Proc. 2019;51:2927–30.
Miao Y, Everly JJ, Gross TG, Tevar AD, First MR, Alloway RR, et al. De novo cancers arising in organ transplant recipients are associated with adverse outcomes compared with the general population. Transplantation. 2009;87:1347.
Taborelli M, Serraino D, Cimaglia C, Furian L, Biancone L, Busnach G, et al. The impact of cancer on the risk of death with a functioning graft of Italian kidney transplant recipients. Am J Transplant. 2022;22:588–98.
Jeong S, Lee HS, Kong SG, Kim DJ, Lee S, Park MJ, et al. Incidence of malignancy and related mortality after kidney transplantation: a nationwide, population-based cohort study in Korea. Sci Rep. 2020;10:21398.
Tessari G, Naldi L, Boschiero L, Minetti E, Sandrini S, Nacchia F, et al. Incidence of primary and second cancers in renal transplant recipients: a multicenter cohort study. Am J Transplant. 2013;13:214–21.
Teo S, Lee K, Lim G, Koo S, Ramirez M, Chow K, et al. Incidence, risk factors and outcomes of malignancies after kidney transplantation in Singapore: a 12-year experience. Singapore Med J. 2019;60:253–9.
Hwang JK, Moon IS, Kim JI. Malignancies after kidney transplantation: a 40-year single-center experience in Korea. Transplant Int. 2011;24:716–21.
Sampaio MS, Cho YW, Qazi Y, Bunnapradist S, Hutchinson IV, Shah T. Posttransplant malignancies in solid organ adult recipients: an analysis of the U.S. national transplant database. Transplant. 2012;94:990–8.
Park HY, Chang BJ, Lim SW, Kim J, Kim JY, Chang DK, et al. Risk of colorectal neoplasia in patients with solid organ transplantation. Clin Transplant. 2012;26:50–6.
Collins MG, Teo E, Cole SR, Chan CY, McDonald SP, Russ GR, et al. Screening for colorectal cancer and advanced colorectal neoplasia in kidney transplant recipients: cross sectional prevalence and diagnostic accuracy study of faecal immunochemical testing for haemoglobin and colonoscopy. BMJ. 2012;345:e4657.
Christenson ES, Lee V, Wang H, Yarchoan M, De Jesus-Acosta A, Azad N, et al. Solid organ transplantation is associated with an increased rate of mismatch repair deficiency and PIK3CA mutations in colorectal cancer. Curr Oncol. 2023;30:75–84.
Ramsey-Goldman R, Brar A, Richardson C, Salifu MO, Clarke A, Bernatsky S, et al. Standardised incidence ratios (SIRs) for cancer after renal transplant in systemic lupus erythematosus (SLE) and non-SLE recipients. Lupus Sci Med. 2016;3:e000156.
Ju MK, Joo DJ, Kim SJ, Huh KH, Kim MS, Jeon KO, et al. Chronologically different incidences of post-transplant malignancies in renal transplant recipients: single center experience. Transplant Int. 2009;22:644–53.
Braconnier P, Del Marmol V, Broeders N, Kianda M, Massart A, Lemy A, et al. Combined introduction of anti-IL2 receptor antibodies, mycophenolic acid and tacrolimus: effect on malignancies after renal transplantation in a single-centre retrospective cohort study. Nephrol Dial Transplant. 2012;27:2547–53.
Cheung CY, Ma MKM, Chak WL, Chau KF, Tang SCW. Conversion to mammalian target of rapamycin inhibitors in kidney transplant recipients with de novo cancers. Oncotarget. 2017;8:44833–41.
Oliveira RC, Tavares-Silva E, Abrantes AM, Antunes H, Teixeira P, Gomes A, et al. De novo colorectal cancer after liver and kidney transplantation–microenvironment disturbance. Transplant Rep. 2020;5:100057.
Adani GL, Baccarani U, Lorenzin D, Gropuzzo M, Tulissi P, Montanaro D, et al. De novo gastrointestinal tumours after renal transplantation: role of CMV and EBV viruses. Clin Transplant. 2006;20:457–60.
Krishnan A, Wong G, Teixeira-Pinto A, Lim WH. Incidence and outcomes of early cancers after kidney transplantation. Transplant Int. 2022;35:10024.
Rascente M, Pisani F, Barletta A, D’Angelo M, Giammaria A, Parzanese I, et al. Malignancies after kidney transplantation. Transplant Proc. 2005;37:2529–31.
Végső G, Tóth M, Hídvégi M, Toronyi É, Mlanger R, Dinya E, et al. Malignancies after renal transplantation during 33 years at a single center. Pathol Oncol Res. 2007;13:63–9.
Arichi N, Kishikawa H, Nishimura K, Mitsui Y, Namba Y, Tokugawa S, et al. Malignancy following kidney transplantation. Transplant Proc. 2008;40:2400–2.
Alasari S, Kim MS, Baik SH, Min BS, Kim NK. Minimally invasive colorectal resection in kidney transplant recipients: technical tips, short- and long-term outcomes. Int Sch Res Not. 2014;2014:1–5.
Rocha A, Malheiro J, Fonseca I, Martins LS, Dias L, Almeida M, et al. Noncutaneous neoplasms after kidney transplantation: analysis at single center. Transplant Proc. 2013;45:1102–5.
Lizakowski S, Kolonko A, Imko-Walczuk B, Komorowska-Jagielska K, Rutkowski B, Więcek A, et al. Solid organ cancer and melanoma in kidney transplant recipients: TumorTx base preliminary results. Transplant Proc. 2018;50:1881–8.
Balhareth A, Reynolds IS, Solon JG, Harte EG, Boland F, O’Sullivan JM, et al. Thirty-seven-year population-based study of colorectal cancer rates in renal transplant recipients in Ireland. Transplant Proc. 2018;50:3434–9.
Kato T, Kakuta Y, Abe T, Yamanaka K, Imamura R, Okumi M, et al. The benefits of cancer screening in kidney transplant recipients: a single‐center experience. Cancer Med. 2015;5:153–8.
Aguiar B, Santos Amorim T, Romãozinho C, Santos L, Macário F, Alves R, et al. Malignancy in kidney transplantation: a 25-year single-center experience in Portugal. Transplant Proc. 2015;47:976–80.
Kehinde EO, Petermann A, Morgan JD, Butt ZA, Donnelly PK, Veitch PS, et al. Triple therapy and incidence of de novo cancer in renal transplant recipients. Br J Surg. 1994;81:985–6.
Lim SM, Jung M, Shin SJ, Baek SJ, Hur H, Min BS, et al. Clinical implications from a single-center study of colorectal adenocarcinoma in transplant recipients. Oncol. 2014;88:195–200.
Kessler M, Jay N, Molle R, Guillemin F. Excess risk of cancer in renal transplant patients. Transplant Int. 2006;19:908–14.
Srisuwarn P, Sutharattanapong N, Disthabanchong S, Kantachuvesiri S, Kitiyakara C, Phakdeekitcharoen B, et al. Incidence of de novo post-transplant malignancies in Thai adult kidney transplant recipients: a single-center, population-controlled, retrospective cohort study at the highest volume kidney transplant center in Thailand. Transplant Int. 2024;37:11614.
Hsiao FY, Hsu WWY. Epidemiology of post-transplant malignancy in Asian renal transplant recipients: a population-based study. Int Urol Nephrol. 2014;46:833–8.
Franke TF. PI3K/Akt: getting it right matters. Oncogene. 2008;27:6473–88.
Dhillon AS, Hagan S, Rath O, Kolch W. MAP kinase signalling pathways in cancer. Oncogene. 2007;26:3279–90.
Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990;61:759–67.
Dantal J, Hourmant M, Cantarovich D, Giral M, Blancho G, Dreno B, et al. Effect of long-term immunosuppression in kidney-graft recipients on cancer incidence: randomised comparison of two cyclosporin regimens. Lancet. 1998;351:623–8.
Kao CC, Liu JS, Chang YK, Lin MH, Lin YC, Chen HH, et al. Cancer and mTOR inhibitors in kidney transplantation recipients. PeerJ. 2018;6:e5864.
Yokoyama I, Hayashi S, Kobayashi T, Yasutomi M, Uchida K, Takagi H. Immunosuppressive drugs and their effect on experimental tumor growth. Transplant Int. 1995;8:251–5.
Basu A, Contreras AG, Datta D, Flynn E, Zeng L, Cohen HT, et al. Overexpression of vascular endothelial growth factor and the development of post-transplantation cancer. Cancer Res. 2008;68:5689–98.
Hojo M, Morimoto T, Maluccio M, Asano T, Morimoto K, Lagman M, et al. Cyclosporine induces cancer progression by a cell-autonomous mechanism. Nature. 1999;397:530–4.
Jung DH, Hwang S, Song GW, Ahn CS, Moon DB, Ha TY, et al. Survival benefit of early cancer detection through regular endoscopic screening for de novo gastric and colorectal cancers in Korean liver transplant recipients. Transplant Proc. 2016;48:145–51.
Wong G, Chapman JR, Craig JC. Cancer screening in renal transplant recipients: What is the evidence? Clin J Am Soc Nephrol. 2008;3:S87–100.
Bini EJ, Kinkhabwala A, Goldfarb DS. Predictive value of a positive fecal occult blood test increases as the severity of CKD worsens. Am J Kidney Dis. 2006;48:580–6.
Wong G, Howard K, Craig JC, Chapman JR. Cost-effectiveness of colorectal cancer screening in renal transplant recipients. Transplantation. 2008;85:532.
Hadjiliadis D, Khoruts A, Zauber AG, Hempstead SE, Maisonneuve P, Lowenfels AB. Cystic fibrosis colorectal cancer screening consensus recommendations. Gastroenterology. 2018;154:736–45.e14.
Lin JS, Perdue LA, Henrikson NB, Bean SI, Blasi PR. Screening for colorectal cancer: updated evidence report and systematic review for the US preventive services task force. JAMA. 2021;325:1978.
Ashkar MH, Chen J, Shy C, Crippin JS, Chen CH, Sayuk GS, et al. Increased risk of advanced colonic adenomas and timing of surveillance colonoscopy following solid organ transplantation. Dig Dis Sci. 2022;67:1858–68.
Puttarajappa C, Yabes J, Bei L, Shah N, Bernardo J, McCauley J, et al. Cancer risk with alemtuzumab following kidney transplantation. Clin Transplant. 2013;27:E264–71.
Author information
Authors and Affiliations
Contributions
BJH and OSE conceptualized the study. BJH, AO, MG, MM, LSLM, and OSE designed the review and meta-analysis methodology. LSLM conducted the literature search, while BJH, AO, and MG handled the review and data extraction. BJH curated the software and created the visualizations. BJH and MM performed the formal analysis. BJH and OSE drafted the manuscript, with AO, MG, HI, MDW, VV, RRR, OSE, and LSLM reviewing multiple iterations. All authors contributed to interpreting the results, had access to the raw data, and approved the final manuscript. OSE supervised the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval and consents to participate were not necessary for the study as it is a systematic review and meta-analysis of previously published, public data. No new human participant data were obtained and includes studies that were conducted in accordance to relevant ethical guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hasjim, B.J., Ostowari, A., Gandawidjaja, M. et al. De novo colorectal cancer after kidney transplantation: a systematic review and meta-analysis. Br J Cancer 132, 1010–1018 (2025). https://doi.org/10.1038/s41416-025-02994-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-02994-7