Abstract
Background
Epidemiological studies have linked psychological stress with an increased risk of breast cancer, however few studies have linked stress hormone signalling to cancer initiation mechanistically. This may be particularly pertinent in populations already at risk due to mutations in the cancer predisposition genes BRCA1/2.
Methods
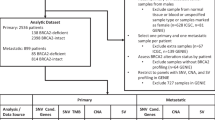
Here we employ BRCA1/2 knockdown in breast and prostate epithelial cells to examine the effects of the stress hormone cortisol on DNA damage and repair. We perform a retrospective analysis of plasma cortisol and urinary 8-OHdG in a female BRCA-mutation carriers cohort (n = 62) and validate our findings in a male cohort (n = 70).
Results
Cortisol promotes DNA damage in normal mammary epithelial cells, and in a BRCA-deficient setting, delays DNA repair. In female BRCA-mutation carriers higher plasma cortisol levels are associated with an increased risk of cancer. In a male BRCA-mutation cohort risk of prostate cancer was also significantly increased in those with higher cortisol levels. Urinary 8-OHdG, a biomarker of oxidative DNA damage, was also correlated with a risk of breast cancer and prostate cancer.
Conclusion
Taken together these findings demonstrate that psychological stress, through the induction of DNA damage by cortisol, may increase the cumulative risk of cancer in BRCA-mutation carriers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to participant confidentiality but are available from the corresponding author on reasonable request.
References
Magnon C. Cancer Builds a Noxious Partnership with Psychologic Stress. Cancer Res. 2024;84:956–7.
Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pr Oncol. 2008;5:466–75.
Batty GD, Russ TC, Stamatakis E, Kivimaki M. Psychological distress in relation to site specific cancer mortality: pooling of unpublished data from 16 prospective cohort studies. BMJ. 2017;356:j108.
Wang X, Wang N, Zhong L, Wang S, Zheng Y, Yang B, et al. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol Psychiatry. 2020;25:3186–97.
Ringwald J, Wochnowski C, Bosse K, Giel KE, Schäffeler N, Zipfel S, et al. Psychological Distress, Anxiety, and Depression of Cancer-Affected BRCA1/2 Mutation Carriers: a Systematic Review. J Genet Couns. 2016;25:880–91.
Dibble KE, Donorfio LKM, Britner PA, Bellizzi KM. Stress, anxiety, and health-related quality of life in BRCA1/2-positive women with and without cancer: A comparison of four US female samples. Gynecologic Oncol Rep. 2022;42:101033.
Wenzel L, Osann K, Lester J, Kurz R, Hsieh S, Nelson EL, et al. Biopsychological stress factors in BRCA mutation carriers. Psychosomatics. 2012;53:582–90.
Falcinelli M, Thaker PH, Lutgendorf SK, Conzen SD, Flaherty RL, Flint MS. The role of psychological stress in cancer initiation: clinical relevance and potential molecular mechanisms. Cancer Res. 2021: canres.0684.2021.
Reeder A, Attar M, Nazario L, Bathula C, Zhang A, Hochbaum D, et al. Stress hormones reduce the efficacy of paclitaxel in triple negative breast cancer through induction of DNA damage. Br J Cancer. 2015;112:1461–70.
Flint MS, Baum A, Chambers WH, Jenkins FJ. Induction of DNA damage, alteration of DNA repair and transcriptional activation by stress hormones. Psychoneuroendocrinology. 2007;32:470–9.
Flaherty RL, Owen M, Fagan-Murphy A, Intabli H, Healy D, Patel A, et al. Glucocorticoids induce production of reactive oxygen species/reactive nitrogen species and DNA damage through an iNOS mediated pathway in breast cancer. Breast Cancer Res. 2017;19:35.
Fridlich R, Annamalai D, Roy R, Bernheim G, Powell SN. BRCA1 and BRCA2 protect against oxidative DNA damage converted into double-strand breaks during DNA replication. DNA Repair (Amst). 2015;30:11–20.
Gray GK, Li CM-C, Rosenbluth JM, Selfors LM, Girnius N, Lin J-R, et al. A human breast atlas integrating single-cell proteomics and transcriptomics. Developmental Cell. 2022;57:1400–1420.e7.
Qu Y, Han B, Yu Y, Yao W, Bose S, Karlan BY, et al. Evaluation of MCF10A as a Reliable Model for Normal Human Mammary Epithelial Cells. PLoS ONE. 2015;10:e0131285.
Castro E, Eeles R. The role of BRCA1 and BRCA2 in prostate cancer. Asian J Androl. 2012;14:409–14.
Karthaus WR, Hofree M, Choi D, Linton EL, Turkekul M, Bejnood A, et al. Regenerative potential of prostate luminal cells revealed by single-cell analysis. Science. 2020;368:497–505.
Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31:1748–57.
Antonova L, Mueller CR. Hydrocortisone down-regulates the tumor suppressor gene BRCA1 in mammary cells: a possible molecular link between stress and breast cancer. Genes Chromosomes Cancer. 2008;47:341–52.
Hara MR, Kovacs JJ, Whalen EJ, Rajagopal S, Strachan RT, Grant W, et al. A stress response pathway regulates DNA damage through beta(2)-adrenoreceptors and beta-arrestin-1. Nature. 2011;477:349–U129.
Warner E. Impact of MRI surveillance and breast cancer detection in young women with BRCA mutations. Ann Oncol. 2011;22:i44–9.
Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychological Med. 2010;40:1797–810.
Kudielka BM, Hellhammer J, Hellhammer DH, Wolf OT, Pirke K-M, Varadi E, et al. Sex Differences in Endocrine and Psychological Responses to Psychosocial Stress in Healthy Elderly Subjects and the Impact of a 2-Week Dehydroepiandrosterone Treatment1. J Clin Endocrinol Metab. 1998;83:1756–61.
Choi MH. Clinical and Technical Aspects in Free Cortisol Measurement. Endocrinol Metab (Seoul). 2022;37:599–607.
Loft S, Poulsen HE. Cancer risk and oxidative DNA damage in man. J Mol Med (Berl). 1996;74:297–312.
Roelfsema F, van Heemst D, Iranmanesh A, Takahashi P, Yang R, Veldhuis JD. Impact of age, sex and body mass index on cortisol secretion in 143 healthy adults. Endocr Connect. 2017;6:500–9.
Sofer Y, Osher E, Limor R, Shefer G, Marcus Y, Shapira I, et al. Gender determines serum free cortisol: higher levels in men. Endocr Pr. 2016;22:1415–21.
Herhaus B, Ullmann E, Chrousos G, Petrowski K. High/low cortisol reactivity and food intake in people with obesity and healthy weight. Transl Psychiatry. 2020;10:40.
Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Esquivel-Soto J, Morales-González A, Esquivel-Chirino C, et al. Inflammation, oxidative stress, and obesity. Int J Mol Sci. 2011;12:3117–32.
Hansen JL, Carroll JE, Seeman TE, Cole SW, Rentscher KE. Lifetime chronic stress exposures, stress hormones, and biological aging: Results from the Midlife in the United States (MIDUS) study. Brain Behav Immun. 2025;123:1159–68.
Bhardwaj P, Iyengar NM, Zahid H, Carter KM, Byun DJ, Choi MH, et al. Obesity promotes breast epithelium DNA damage in women carrying a germline mutation in BRCA1 or BRCA2. Sci Transl Med. 2023;15:eade1857.
Mouchacca J, Abbott GR, Ball K. Associations between psychological stress, eating, physical activity, sedentary behaviours and body weight among women: a longitudinal study. BMC Public Health. 2013;13:828.
Chen H, Wu J, Zhang Z, Tang Y, Li X, Liu S, et al. Association Between BRCA Status and Triple-Negative Breast Cancer: A Meta-Analysis. Front Pharm. 2018;9:909.
Badve S, Dabbs DJ, Schnitt SJ, Baehner FL, Decker T, Eusebi V, et al. Basal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pathologists and oncologists. Mod Pathol. 2011;24:157–67.
Lim E, Vaillant F, Wu D, Forrest NC, Pal B, Hart AH, et al. Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nat Med. 2009;15:907–13.
Zhou J, Chen Q, Zou Y, Chen H, Qi L, Chen Y. Stem cells and cellular origins of breast cancer: updates in the rationale, controversies, and therapeutic Implications. Front Oncol. 2019;9:820.
Yeh S, Hu YC, Rahman M, Lin HK, Hsu CL, Ting HJ, et al. Increase of androgen-induced cell death and androgen receptor transactivation by BRCA1 in prostate cancer cells. Proc Natl Acad Sci USA. 2000;97:11256–61.
Shin S, Verma IM. BRCA2 cooperates with histone acetyltransferases in androgen receptor-mediated transcription. Proc Natl Acad Sci. 2003;100:7201–6.
Arora VK, Schenkein E, Murali R, Subudhi SK, Wongvipat J, Balbas MD, et al. Glucocorticoid receptor confers resistance to antiandrogens by bypassing androgen receptor blockade. Cell. 2013;155:1309–22.
Kach J, Conzen SD, Szmulewitz RZ. Targeting the glucocorticoid receptor in breast and prostate cancers. Sci Transl Med. 2015;7:305ps19.
Spera G, Fresco R, Fung H, Dyck JRB, Pituskin E, Paterson I, et al. Beta blockers and improved progression-free survival in patients with advanced HER2 negative breast cancer: a retrospective analysis of the ROSE/TRIO-012 study. Ann Oncol. 2017;28:1836–41.
Løfling LL, Støer NC, Sloan EK, Chang A, Gandini S, Ursin G, et al. β-blockers and breast cancer survival by molecular subtypes: a population-based cohort study and meta-analysis. Br J Cancer. 2022;127:1086–96.
Hiller JG, Cole SW, Crone EM, Byrne DJ, Shackleford DM, Pang J-MB, et al. Preoperative β-Blockade with Propranolol Reduces Biomarkers of Metastasis in Breast Cancer: A Phase II Randomized Trial. Clin Cancer Res. 2020;26:1803–11.
Tian X, Zhou X, Sun M, Yu NX, Peng Y, Zheng X, et al. The effectiveness of positive psychological interventions for patients with cancer: A systematic review and meta-analysis. J Clin Nurs. 2024;33:3752–74.
Bognár SA, Teutsch B, Bunduc S, Veres DS, Szabó B, Fogarasi B, et al. Psychological intervention improves quality of life in patients with early-stage cancer: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2024;14:13233.
Flaherty RL, Intabli H, Falcinelli M, Bucca G, Hesketh A, Patel BA, et al. Stress hormone-mediated acceleration of breast cancer metastasis is halted by inhibition of nitric oxide synthase. Cancer Lett. 2019;459:59–71.
Acknowledgements
We are indebted to all of the men and women who are taking part in this study. We also would like to thank the research collaborators and steering committee (Appendix A).
Funding
MF is supported by Rosetrees Trust. The clinical studies are coordinated by the Institute of Cancer Research, London, UK and supported by grants from Cancer Research UK (Grant references (C5047/A21332, C5047/A13232 and C5047/A17528), The Ronald and Rita McAulay Foundation, Prostate Cancer UK – London Movember Centre of Excellence (CEO13_2-002), and the support of the NIHR to the Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualisation and funding – MSF and RE. Sample collection – EB, EP and RE. Experimental design and investigations – RLF, MF, BAP. Data processing and analysis -RLF, MF and ARH. Writing, review and editing – RLF, MSF, MF, EB, EP, RE and ASH.
Corresponding author
Ethics declarations
Competing interests
Professor Rosalind Eeles has the following conflicts of interest to declare: Honoraria from GU-ASCO, Janssen, University of Chicago, Dana Farber Cancer Institute USA as a speaker. Educational honorarium from Bayer and Ipsen, member of external expert committee to Astra Zeneca UK and Member of Active Surveillance Movember Committee. She is a member of the SAB of Our Future Health. She undertakes private practice as a sole trader at The Royal Marsden NHS Foundation Trust and 90 Sloane Street SW1X 9PQ and 280 Kings Road SW3 4NX, London, UK. The remaining authors declare no competing interest.
Ethical approval
The IMPACT study protocol was reviewed and approved by the West-Midlands Research and Ethics Committee in the UK (reference: 05/MRE07/25) and subsequently by each participating institution’s local committee. All participants provided written consent, and the study was performed in accordance with the Declaration of Helsinki. The clinical studies are coordinated by the Institute of Cancer Research, London, UK. This project represents independent research supported by The National Institute for Health Research (NIHR) Biomedical Research Centre at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flaherty, R.L., Falcinelli, M., Hesketh, A.R. et al. Biomarkers of psychological stress are associated with increased susceptibility to the development of breast and prostate cancer in BRCA1/2 mutation carriers. Br J Cancer 133, 615–624 (2025). https://doi.org/10.1038/s41416-025-03085-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03085-3