Abstract
Background
Childhood malnutrition is well estimated as the major underlying risk factor for morbidity and mortality in children under 5 years. Feeding practices greatly influence the dietary condition of children aged 6–23 months in developing countries. Therefore, this study was performed to determine the association between infant young children feeding (IYCF) practices and the dietary conditions of children aged 6–23 months in Ethiopia.
Method
A cross-sectional study was conducted based on data on 5638 children aged 6–23 months from three Ethiopia Demographic and Health Surveys (EDHS) (2005, 2011, 2016). Multivariable logistic regression was performed to estimate the odd ratios (ORs) and 95% confidence intervals (CIs) of stunting and anaemia with IYCF practices.
Result
The prevalence of stunting among children aged 6–23 months in Ethiopia decreased greatly from 49% in 2005 to 32% in 2016. Among the IYCF practices, consumption of iron-rich foods, minimum dietary diversity (MDD), and minimum acceptable diet (MAD) were significant predictors of stunting. In addition, the prevalence of anaemia declined significantly from 26% in 2005 to 16% in 2011, but increased to 29% in 2016. Among the IYCF practices, breastfeeding and minimum meal frequency (MMF) had lower odds of childhood anaemia.
Conclusions
The present study showed that anaemia and stunting among children aged 6–23 months in Ethiopia is critical public health problems that need urgent attention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Prescott SL, Logan AC, Albrecht G, Campbell DE, Crane J, Cunsolo A. et al. The Canmore Declaration: Statement of Principles for Planetary Health. J Chall. 2018;9:31. https://doi.org/10.3390/challe9020031.
Central Statistical Agency Addis Ababa. Demographic CE Health Survey-2011. Maryland, USA: Ethiopia ICF International Calverton; 2012. 2016.
Addis Ababa: UNECA. The Cost of Hunger in Africa: Social and economic impact of child undernutrition in Egypt, Ethiopia, Swaziland and Uganda. Ethiopia: Addis Ababa: UNECA; 2015.
Social AUC. Journal of the cost of hunger in Africa, economic impact of child undernutrition in Egypt E, Swaziland, Uganda. NEPAD Planning and Coordinating Agency, UN Economic Commission for Africa, and UN World Food Programme. Uganda: Social AUC; 2014.
World Health Organization. The global prevalence of anaemia in 2011. Geneva, Switzerland: World Health Organization; 2015.
Wessells KR, Ouédraogo CT, Young RR, Faye MT, Brito A, Hess SY. Micronutrient status among pregnant women in Zinder, Niger and risk factors associated with deficiency. J Nutrients. 2017;9:430. https://doi.org/10.3390/nu9050430.
Mahmoud H, Muddathir A, Osman S, Ma AKKA. Iron deficiency anemia among children under three years in Kassala, Eastern Sudan. J Sudan J Pub Heal. 2014;9:33–7.
Sop MMK, Mananga M-J, Tetanye E, Gouado I. Risk factors of anemia among young children in rural Cameroon. J Int J Curr Microbiol Appl Sci. 2015;4:925–35.
Diouf S, Folquet M, Mbofung K, Ndiaye O, Brou K, Dupont C, et al. Prevalence and determinants of anemia in young children in French-speaking Africa. Role of iron deficiency. J Arch de Pediatroc. 2015;22:1188–97. https://doi.org/10.1016/j.arcped.2015.08.015.
Ewusie JE, Ahiadeke C, Beyene J, Hamid JS. Prevalence of anemia among under-5 children in the Ghanaian population: estimates from the Ghana demographic and health survey. J BMC Public Health. 2014;14:626. https://doi.org/10.1186/1471-2458-14-626.
Wegmüller R, Bah A, Kendall L, Goheen MM, Mulwa S, Cerami C, et al. Efficacy and safety of hepcidin-based screen-and-treat approaches using two different doses versus a standard universal approach of iron supplementation in young children in rural Gambia: a double-blind randomised controlled trial. J BMC Pediatrics. 2016;16:1–9. https://doi.org/10.1186/s12887-016-0689-4.
Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ. Child malnutrition in sub-Saharan Africa: a meta-analysis of demographic and health surveys (2006-2016). J PloS ONE. 2017;12:e0177338. https://doi.org/10.1371/journal.pone.0177338.
World Health Organization, United Nations Children’s Fund. WHO child growth standards and the identification of severe acute malnutrition in infants and children: a joint statement by the World Health Organization and the United Nations Children’s Fund. Geneva, Switzerland: World Health Organization, United Nations Children’s Fund; 2009.
Setegn T, Belachew T, Gerbaba M, Deribe K, Deribew A, Biadgilign S. Factors associated with exclusive breastfeeding practices among mothers in Goba district, south east Ethiopia: a cross-sectional study. Int Breastfeed J. 2012;7:17. https://doi.org/10.1186/1746-4358-7-17.
Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia, and Calverton, Maryland, USA: Central Statistical Agency and ICF International; 2012.
ORC Macro. Central Statistical Agency: Ethiopia demographic and health survey 2005. Calverton, Maryland, USA: ORC Macro; 2006.
CSA and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
World Health Organization. Global nutrition targets 2025: stunting policy brief. Geneva, Switzerland: World Health Organization; 2014.
CSA and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, Rockville Maryland, USA: CSA and ICF, 2016.
WHO. Joint statement by the WHO and the United Nations Children’s Fund. WHO AnthroPlus for personal computers Manual: Software for assessing growth of the world’s children and adolescents. Geneva, Switzerland: WHO; 2009.
UNICEF. Infant and young child feeding: programming guide. New York: UNICEF; 2011.17-8.
Arakaki L, Green D, Kwist A, Slyker J. Nutrition dae summary report. University of Washington Strategic Analysis, Research & Training (Start) Center. The Bill and Melinda Gates Foundation, 2017.
Disha A, Rawat R, Subandoro A, Menon P. Infant and young child feeding (IYCF) practices in Ethiopia and Zambia and their association with child nutrition: analysis of demographic and health survey data. Afr J Food Agric Nutr Dev. 2012;12:5895–914.
Arimond M, Ruel MT. Dietary diversity is associated with child nutritional status: evidence from 11 demographic and health surveys. J Nutr 2004;134:2579–85. https://doi.org/10.1093/jn/134.10.2579.
Rah JH, Akhter N, Semba RD, De Pee S, Bloem MW, Campbell AA. et al. Low dietary diversity is a predictor of child stunting in rural Bangladesh. Eur J Clin Nutr. 2010;64:1393–8. https://doi.org/10.1038/ejcn.2010.171.
Reese-Masterson A, Maehara M, Gathii MM. Stunting and wasting in children under two years old in a semi-nomadic pastoralist population in Kenya. Kenya: Field Exchange; 2016. 11.
Tadesse A, Hailu D, Bosha T. Nutritional status and associated factors among pastoralist children aged 6–23 months in Benna Tsemay Woreda, South Omo zone, Southern Ethiopia. Int J Nutr Food Sci. 2018;7:11–23. https://doi.org/10.11648/j.ijnfs.20180701.13.
Glover-Amengor M, Agbemafle I, Hagan LL, Mboom FP, Gamor G, Larbi A, et al. Nutritional status of children 0–59 months in selected intervention communities in northern Ghana from the africa RISING project in 2012. J Arch Public Health. 2016;74:12. https://doi.org/10.1186/s13690-016-0124-1.
Ahmed M, Demissie M, Worku A, Abrha A, Berhane Y. Socio-cultural factors favoring home delivery in Afar pastoral community, northeast Ethiopia: a qualitative study. J Reprod Health. 2019;16:1–9. https://doi.org/10.1186/s12978-019-0833-3.
An Evidence-Informed Policy Brief. Reducing Stunting in Ethiopia: “From Promise to Impact”, https://doi.org/10.1007/SpringerReference_300857.
Zerfu TA, Umeta M, Baye K. Dietary habits, food taboos, and perceptions towards weight gain during pregnancy in Arsi, rural central Ethiopia: a qualitative cross-sectional study. J Health Popul Nutr. 2016;35:1–7. https://doi.org/10.1186/s41043-016-0059-8.
Akombi BJ, Agho KE, Hall JJ, Merom D, Astell-Burt T, Renzaho AM. Stunting and severe stunting among children under-5 years in Nigeria: a multilevel analysis. J BMC Pediatrics. 2017;17:15. https://doi.org/10.1186/s12887-016-0770-z.
Mwangome M, Prentice A, Plugge E, Nweneka C. Determinants of appropriate child health and nutrition practices among women in rural Gambia. J Health Popul Nutr. 2010;28:167.
de-Graft Aikins A. Food beliefs and practices during pregnancy in Ghana: implications for maternal health interventions. J Health Care Women Int. 2014;35:954–72. https://doi.org/10.1080/07399332.2014.926902.
Lartey A. Maternal and child nutrition in Sub-Saharan Africa: challenges and interventions. J Proc Nutr Soc. 2008;67:105–8. https://doi.org/10.1017/S0029665108006083.
Agize A, Jara D, Dejenu G. Level of knowledge and practice of mothers on minimum dietary diversity practices and associated factors for 6–23-month-old children in Adea Woreda, Oromia, Ethiopia. J BioMed Res Int. 2017;2017, https://doi.org/10.1155/2017/7204562.
World Health Organization. Working group on infant and young child feeding indicators, developing and validating simple indicators of dietary quality and energy intake of infants and young child in developing countries. Washington, DC, USA: World Health Organization; 2007.
Fekadu Y, Mesfin A, Haile D, Stoecker BJ. Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: a cross-sectional study. J BMC Public Health. 2015;15:846. https://doi.org/10.1186/s12889-015-2190-7.
Bukusuba J, Kikafunda J, Whitehead RJ. Nutritional status of children (6-59 months) among HIV-positive mothers/caregivers living in an urban setting of Uganda. African J Food Agric Nutr Dev. 2009;9.
Saaka M, Wemakor A, Abizari A-R, Aryee P. How well do WHO complementary feeding indicators relate to nutritional status of children aged 6–23 months in rural Northern Ghana? J BMC Public Health. 2015;15:1157. https://doi.org/10.1186/s12889-015-2494-7.
Sawadogo PS, Martin-Prevel Y, Savy M, Kameli Y, Traissac P, Traoré AS, et al. An infant and child feeding index is associated with the nutritional status of 6-to 23-month-old children in rural Burkina Faso. J Nutr. 2006;136:656–63. https://doi.org/10.1093/jn/136.3.656.
Ethiopia Central Statistical Agency. Demographic Health Survey 2011 Addis Ababa. Ethiopia: Ethiopia Central Statistical Agency; 2012.
UNICEF, WHO. Indicators for assessing infant and young child feeding practices, part 3. Country profiles. Geneva, Switzerland: UNICEF, WHO; 2010.
UNICEF. Improving child nutrition: the achievable imperative for global progress. New York, NY: UNICEF; 2013.
Yimer G. Malnutrition among children in Southern Ethiopia: levels and risk factors. Ethiopian J Health Dev. 2000;14. https://doi.org/10.4314/ejhd.v14i3.9901.
Amare ZY, Ahmed ME, Mehari AB. Determinants of nutritional status among children under age 5 in Ethiopia: further analysis of the 2016 Ethiopia demographic and health survey. J Globalization Health. 2019;15:62. https://doi.org/10.1186/s12992-019-0505-7.
Wamani H, Tylleskär T, Åstrøm AN, Tumwine JK, Peterson S. Mothers’ education but not fathers’ education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. Int J Equity Health. 2004;3:9. https://doi.org/10.1186/1475-9276-3-9.
Burchi F. Child nutrition in Mozambique in 2003: the role of mother’s schooling and nutrition knowledge. J Econ Hum Biol. 2010;8:331–45. https://doi.org/10.1016/j.ehb.2010.05.010.
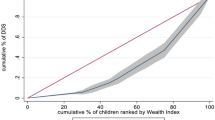
Novignon J, Aboagye E, Agyemang OS, Aryeetey G. Socioeconomic-related inequalities in child malnutrition: evidence from the Ghana multiple indicator cluster survey. J Health Econ Rev. 2015;5:34 https://doi.org/10.1186/s13561-015-0072-4.
Oyekale AS. Factors explaining acute malnutrition among under-five children in Sub-Sahara Africa (SSA). J Life Sci J. 2012;9:2101–7.
Keats A. Women’s schooling, fertility, and child health outcomes: Evidence from Uganda’s free primary education program. J Dev Econ 2018;135:142–59. https://doi.org/10.1016/j.jdeveco.2018.07.002.
Smith LC, Haddad LJ. Explaining child malnutrition in developing countries: a cross-country analysis. International Food Policy Research Institute (IFPRI). Washington, D.C. 2000.
Mukabutera A, Thomson DR, Hedt-Gauthier BL, Basinga P, Nyirazinyoye L, Murray M. Risk factors associated with underweight status in children under five: an analysis of the 2010 Rwanda Demographic Health Survey (RDHS). J BMC Nutr. 2016;2:40. https://doi.org/10.1186/s40795-016-0078-2.
Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. What works? Interventions for maternal and child undernutrition and survival. J Lancet. 2008;371:417–40. https://doi.org/10.1016/S0140-6736(07)61693-6.
Iannotti LL, Dulience SJL, Green J, Joseph S, François J, Antenor M-L, et al. Linear growth increased in young children in an urban slum of Haiti: a randomized controlled trial of a lipid-based nutrient supplement. Am J Clin Nutr. 2014;99:198–208. https://doi.org/10.3945/ajcn.113.063883.
Sunguya BF, Poudel KC, Mlunde LB, Urassa DP, Yasuoka J, Jimba M. Poor nutrition status and associated feeding practices among HIV-positive children in a food secure region in Tanzania: a call for tailored nutrition training. J PloS ONE. 2014;9:e98308. https://doi.org/10.1371/journal.pone.0098308.
Beyene M, Worku AG, Wassie MM. Dietary diversity, meal frequency and associated factors among infant and young children in Northwest Ethiopia: a cross-sectional study. J BMC Public Health. 2015;15:1007. https://doi.org/10.1186/s12889-015-2333-x.
Tegegne M, Sileshi S, Benti T, Teshome M, Woldie H. Factors associated with minimal meal frequency and dietary diversity practices among infants and young children in the predominantly agrarian society of Bale zone, Southeast Ethiopia: a community based cross sectional study. J Arch Public Health. 2017;75:53. https://doi.org/10.1186/s13690-017-0216-6.
Temesgen H, Negesse A, Woyraw W, Mekonnen N. Dietary diversity feeding practice and its associated factors among children age 6–23 months in Ethiopia from 2011 up to 2018: a systematic review and meta-analysis. Ital J Pediatrics. 2018;44:1–10. https://doi.org/10.1186/s13052-018-0567-9.
Victor R, Baines SK, Agho KE, Dibley MJ. Factors associated with inappropriate complementary feeding practices among children aged 6–23 months in T anzania. J Matern child Nutr. 2014;10:545–61. https://doi.org/10.1111/j.1740-8709.2012.00435.x.
Bhandari N, Mazumder S, Bahl R, Martines J, Black RE, Bhan MK, et al. Use of multiple opportunities for improving feeding practices in under-twos within child health programmes. J Health Policy Plan. 2005;20:328–36. https://doi.org/10.1093/heapol/czi039.
Shi L, Zhang J. Recent evidence of the effectiveness of educational interventions for improving complementary feeding practices in developing countries. J Tropical Pediatrics. 2011;57:91–8. https://doi.org/10.1093/tropej/fmq053.
Aemro M, Mesele M, Birhanu Z, Atenafu A. Dietary diversity and meal frequency practices among infant and young children aged 6–23 months in Ethiopia: a secondary analysis of Ethiopian demographic and health survey 2011. J Nutr Metabol. 2013, https://doi.org/10.1155/2013/782931.
Korir JK. Determinants of complementary feeding practices and nutritional status of children 6-23 months old in Korogocho slum, Nairobi County, Kenya. Nairobi: Kenyatta University; 2013.
Tessema M, Belachew T, Ersino G. Feeding patterns and stunting during early childhood in rural communities of Sidama, South Ethiopia. Pan African Med J. 2013;14, https://doi.org/10.11604/pamj.2013.14.75.1630.
Miah R, Apanga P, Abdul-Haq Z. Risk factors for undernutrition in children under five years old: evidence from the 2011 Ghana multiple indicator cluster Survey. J AIDS Clin Res. 2016;7:2.
Belay E, Endrias A, Alem B, Endris K. Hematological responses to iron-folate supplementation and its determinants in pregnant women attending antenatal cares in Mekelle City, Ethiopia. J PloS ONE. 2018;13:e0204791. https://doi.org/10.1371/journal.pone.0204791.
Habte D, Asrat K, Magafu MG, Ali IM, Benti T, Abtew W, et al. Maternal risk factors for childhood anaemia in Ethiopia. Afr J Reprod Health. 2013;17:110–8.
Roba KT, O’Connor TP, Belachew T, O’Brien NM. Anemia and undernutrition among children aged 6–23 months in two agroecological zones of rural Ethiopia. J Pediatr Health Med Ther. 2016;7:131. https://doi.org/10.2147/PHMT.S109574.
Fisseha T, Sarkar D, D’Agostino A, Moorthy D, Namaste S, Harvey P. Making every move count. Multisectoral tools to guide national and district anemia programming. 91, Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) project, Arlington, Virginia, USA.
Adu-Afarwuah S, Lartey A, Brown KH, Zlotkin S, Briend A, Dewey KG. Home fortification of complementary foods with micronutrient supplements is well accepted and has positive effects on infant iron status in Ghana. Am J Clin Nutr. 2008;87:929–38. https://doi.org/10.1093/ajcn/87.4.929.
Siekmans K, Receveur O, Haddad S. Can an integrated approach reduce child vulnerability to anaemia? Evidence from three African countries. J PloS ONE. 2014;9:e90108. https://doi.org/10.1371/journal.pone.0090108.
Steyn NP, Nel JH, Nantel G, Kennedy G, Labadarios D. Food variety and dietary diversity scores in children: are they good indicators of dietary adequacy? J Public health Nutr. 2006;9:644–50. https://doi.org/10.1079/PHN2005912.
Forsido SF. Upgrading starchy staples for tackling malnutrition in South-West Ethiopia. Ethiopia: Kassel, University of Kassel, Department of Organic Agricultural Sciences; 2018. https://doi.org/10.17170/kobra-2019010888.
Jabbar M, Ehui S, Staal SJ. Handbook of livestock statistics for developing countries. Socio-economics Policy Research Working Paper-International Livestock Research Institute. 2000.
Temesgen M. Nutritional status of Ethiopian weaning and complementary foods: a review. J Open Access Sci Rep. 2013;2:1–9.
Shadan MR, Waghray K, Khoushabi F. Formulation, preparation and evaluation of low-cost extrude products based on cereals and pulses. J Food Nutr Sci. 2014, https://doi.org/10.4236/fns.2014.514145.
Gebretsadikan TM, Bultosa G, Forsido SF, Astatkie T. Nutritional quality and acceptability of sweet potato–soybean–moringa composite porridge. J Nutr Food Sci. 2015. https://doi.org/10.1108/NFS-05-2015-0048.
Krasevec J, An X, Kumapley R, Bégin F, Frongillo EA. Diet quality and risk of stunting among infants and young children in low‐and middle‐income countries. J Matern Child Nutr. 2017;13:e12430. https://doi.org/10.1111/mcn.12430.
Acknowledgements
We acknowledge the USAID-DHS Program for providing access to the 2005–2016 Ethiopian Demographic and Health Survey. We thank Rahel Abebe and Dr. Asfaw Negero for their contribution to the manuscript.
Author information
Authors and Affiliations
Contributions
AFH and CY conception and design of the study. AFH acquisition, analysis and/or interpretation of data. AAT and YTD were revising the manuscript. XZ, SH, and EGA critical revision. AFH had primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41430_2020_828_MOESM2_ESM.docx
Percent distribution of children aged 6-23 months by socio-demographic & maternal, and child characteristics, (2005-2016 demographic and health survey)
Rights and permissions
About this article
Cite this article
Hiruy, A.F., Teshome, A.A., Desta, Y.T. et al. Dietary condition and feeding practices of children aged 6–23 months in Ethiopia: analysis of 2005–2016 demographic and health survey. Eur J Clin Nutr 75, 1047–1059 (2021). https://doi.org/10.1038/s41430-020-00828-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-020-00828-8
This article is cited by
-
Access to child-feeding counseling service and determinant factors among breastfeeding mothers in Ethiopia: a multilevel complex data analysis of 2019 Ethiopian mini demographic and health survey
BMC Health Services Research (2025)
-
Association of dietary diversity and odds of anemia in children and adolescents: a systematic review and meta-analysis of observational studies
BMC Nutrition (2025)
-
Determinants of undernutrition among young children in Ethiopia
Scientific Reports (2022)