Abstract
Background
Anthropometric measurements (AMs) are cost-effective surrogates for evaluating body size. This study aimed to identify the optimal prognostic AMs, their thresholds, and their joint associations with cancer mortality.
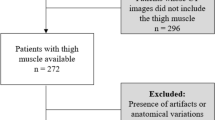
Methods
We performed an observational cohort study including 12138 patients with cancer at five institutions in China. Information on demographics, disease, nutritional status, and AMs, including the body mass index, mid-arm muscle circumference, mid-arm circumference, handgrip strength, calf circumference (CC), and triceps-skinfold thickness (TSF), was collected and screened as mortality predictors. The optimal stratification was used to determine the thresholds to categorize those prognostic AMs, and their associations with mortality were estimated independently and jointly by calculating multivariable-adjusted hazard ratios (HRs).
Results
The study included 5744 females and 6394 males with a mean age of 56.9 years. The CC and TSF were identified as better mortality predictors than other AMs. The optimal thresholds were women 30 cm and men 32.8 cm for the CC, and women 21.8 mm and men 13.6 mm for the TSF. Patients in the low CC or low TSF group had a 13% (HR = 1.13, 95% CI = 1.03–1.23) and 22% (HR = 1.22, 95% CI = 1.12–1.32) greater mortality risk compared with their normal CC/TSF counterparties, respectively. Concurrent low CC and low TSF showed potential joint effect on mortality risk (HR = 1.39, 95% CI = 1.25–1.55).
Conclusions
These findings support the importance of assessing the CC and TSF simultaneously in hospitalized cancer patients to guide interventions to optimize their long-term outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available to protect patient confidentiality, but are available from the corresponding author on reasonable request.
References
Caan BJ, Cespedes Feliciano EM, Prado CM, Alexeeff S, Kroenke CH, Bradshaw P, et al. Association of muscle and adiposity measured by computed tomography with survival in patients with nonmetastatic breast cancer. JAMA Oncol. 2018;4:798–804.
Martinez-Tapia C, Diot T, Oubaya N, Paillaud E, Poisson J, Gisselbrecht M, et al. The obesity paradox for mid- and long-term mortality in older cancer patients: a prospective multicenter cohort study. Am J Clin Nutr. 2020. https://doi.org/10.1093/ajcn/nqaa238 (Online ahead of print).
Paixao EMS, Gonzalez MC, Nakano EY, Ito MK, Pizato N. Weight loss, phase angle, and survival in cancer patients undergoing radiotherapy: a prospective study with 10-year follow-up. Eur J Clin Nutr. 2020. https://doi.org/10.1038/s41430-020-00799-w (Online ahead of print).
Yin L, Lin X, Zhao Z, Li N, He X, Zhang M, et al. Is hand grip strength a necessary supportive index in the phenotypic criteria of the GLIM-based diagnosis of malnutrition in patients with cancer? Support Care Cancer 2021. https://doi.org/10.1007/s00520-020-05975-z (Online ahead of print).
Yin L, Lin X, Liu J, Li N, He X, Zhang M, et al. Classification tree-based machine learning to visualize and validate a decision tool for identifying malnutrition in cancer patients. JPEN J Parenter Enteral Nutr. 2021. https://doi.org/10.1002/jpen.2070 (Online ahead of print).
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in a prospective cohort of US adults. N Engl J Med. 1999;341:1097–105.
Sun YQ, Burgess S, Staley JR, Wood AM, Bell S, Kaptoge SK, et al. Body mass index and all cause mortality in HUNT and UK Biobank studies: linear and non-linear mendelian randomisation analyses. BMJ. 2019;364:l1042.
Kroenke CH, Neugebauer R, Meyerhardt J, Prado CM, Weltzien E, Kwan ML, et al. Analysis of body mass index and mortality in patients with colorectal cancer using causal diagrams. JAMA Oncol. 2016;2:1137–45.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K, et al. Body fatness and cancer-viewpoint of the IARC Working Group. N Engl J Med. 2016;375:794–8.
Chan DSM, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014;25:1901–14.
Weiss L, Melchardt T, Habringer S, Boekstegers A, Hufnagl C, Neureiter D, et al. Increased body mass index is associated with improved overall survival in diffuse large B-cell lymphoma. Ann Oncol. 2014;25:171–6.
Nagai M, Kuriyama S, Kakizaki M, Ohmori-Matsuda K, Sugawara Y, Sone T, et al. Effect of age on the association between body mass index and all-cause mortality: the Ohsaki cohort study. J Epidemiol. 2010;20:398–407.
Sheean P, Gonzalez MC, Prado CM, McKeever L, Hall AM, Braunschweig CA. American Society for Parenteral and Enteral Nutrition Clinical Guidelines: the validity of body composition assessment in clinical populations. JPEN J Parenter Enter Nutr. 2020;44:12–43.
Oh H, Kwak SY, Jo G, Lee J, Park D, Lee DH, et al. Adiposity and mortality in Korean adults: a population-based prospective cohort study. Am J Clin Nutr. 2020. https://doi.org/10.1093/ajcn/nqaa258 (Online ahead of print).
van der Werf A, Langius JAE, de van der Schueren MAE, Nurmohamed SA, van der Pant K, Blauwhoff-Buskermolen S, et al. Percentiles for skeletal muscle index, area and radiation attenuation based on computed tomography imaging in a healthy Caucasian population. Eur J Clin Nutr. 2018;72:288–96.
Ueno A, Yamaguchi K, Sudo M, Imai S. Sarcopenia as a risk factor of severe laboratory adverse events in breast cancer patients receiving perioperative epirubicin plus cyclophosphamide therapy. Support Care Cancer. 2020;28:4249–54.
Ulmann G, Kai J, Durand JP, Neveux N, Jouinot A, De Bandt JP, et al. Creatinine-to-cystatin C ratio and bioelectrical impedance analysis for the assessement of low lean body mass in cancer patients: Comparison to L3-computed tomography scan. Nutrition. 2020;81:110895.
Hurt RT, Ebbert JO, Croghan I, Nanda S, Schroeder DR, Teigen LM, et al. The comparison of segmental multifrequency bioelectrical impedance analysis and dual-energy X-ray absorptiometry for estimating fat free mass and percentage body fat in an ambulatory population. JPEN J Parenter Enteral Nutr. 2020;45:1231–8.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300–7 e2.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:601.
Jensen GL, Cederholm T, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. JPEN J Parenter Enter Nutr. 2019;43:32–40.
Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, et al. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. BMJ. 2018;362:k2575.
Braganza MZ, Kitahara CM, Berrington de Gonzalez A, Inskip PD, Johnson KJ, Rajaraman P. Ionizing radiation and the risk of brain and central nervous system tumors: a systematic review. Neuro Oncol. 2012;14:1316–24.
Meulepas JM, Ronckers CM, Smets A, Nievelstein RAJ, Gradowska P, Lee C, et al. Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst. 2019;111:256–63.
Ferrao B, Neves PM, Santos T, Capelas ML, Makitie A, Ravasco P. Body composition changes in patients with head and neck cancer under active treatment: a scoping review. Support Care Cancer. 2020;28:4613–25.
Cao J, Xu H, Li W, Guo Z, Lin Y, Shi Y, et al. Nutritional assessment and risk factors associated to malnutrition in patients with esophageal cancer. Curr Probl Cancer. 2020;45:100638.
Yin L, Lin X, Li N, Zhang M, He X, Liu J, et al. Evaluation of the global leadership initiative on malnutrition criteria using different muscle mass indices for diagnosing malnutrition and predicting survival in lung cancer patients. JPEN J Parenter Enteral Nutr. 2020. https://doi.org/10.1002/jpen.1873 (Online ahead of print).
Wang N, Khankari NK, Cai H, Li HL, Yang G, Gao YT, et al. Prediagnosis body mass index and waist-hip circumference ratio in association with colorectal cancer survival. Int J Cancer. 2017;140:292–301.
Ho SY, Guo HR, Chen HH, Peng CJ. Nutritional predictors of survival in terminally ill cancer patients. J Formos Med Assoc. 2003;102:544–50.
Sousa IM, Bielemann RM, Gonzalez MC, da Rocha IMG, Barbalho ER, de Carvalho ALM, et al. Low calf circumference is an independent predictor of mortality in cancer patients: a prospective cohort study. Nutrition. 2020;79-80:110816.
Yin L, Liu J, Lin X, Li N, Guo J, Fan Y, et al. Nutritional features-based clustering analysis as a feasible approach for early identification of malnutrition in patients with cancer. Eur J Clin Nutr 2021. https://doi.org/10.1038/s41430-020-00844-8 (Online ahead of print).
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Xu H, Song C, Wang C, Fu Z, Guo Z, Lin Y, et al. Investigation on nutrition status and clinical outcome of patients with common cancers in Chinese patients: a multicenter prospective study protocol. Int J Clin Trials. 2020;7:94–102.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M, Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
Murri R, Scoppettuolo G, Damiano F, Ammassari A, Fantoni M, Antinori A. Karnofsky performance status and assessment of global health status. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;13:294–5.
Wan C, Meng Q, Yang Z, Tu X, Feng C, Tang X, et al. Validation of the simplified Chinese version of EORTC QLQ-C30 from the measurements of five types of inpatients with cancer. Ann Oncol. 2008;19:2053–60.
Giesinger JM, Kieffer JM, Fayers PM, Groenvold M, Petersen MA, Scott NW, et al. Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. J Clin Epidemiol. 2016;69:79–88.
Chen C, Lu FC, Department of Disease Control Ministry of Health PRC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17:1–36. Suppl
Sauerbrei W, Royston P, Binder H. Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med. 2007;26:5512–28.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31:1539–47.
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9:629–35.
Xu MC, Huelster HL, Hatcher JB, Avulova S, Stocks BT, Glaser ZA, et al. Obesity is associated with longer survival independent of sarcopenia and myosteatosis in metastatic and/or castrate-resistant prostate cancer. J Urol. 2020;101097JU0000000000001428.
Pan YP, Kuo HC, Hsu TY, Lin JY, Chou WC, Lai CH, et al. Body mass index-adjusted body weight loss grading predicts overall survival in esophageal squamous cell carcinoma patients. Nutr Cancer. 2020;73:1130–7.
Gonzalez MC, Pastore CA, Orlandi SP, Heymsfield SB. Obesity paradox in cancer: new insights provided by body composition. Am J Clin Nutr. 2014;99:999–1005.
Souza NC, Gonzalez MC, Martucci RB, Rodrigues VD, de Pinho NB, Qureshi AR, et al. Comparative analysis between computed tomography and surrogate methods to detect low muscle mass among colorectal cancer patients. JPEN J Parenter Enteral Nutr. 2020;44:1328–37.
Xu JY, Zhu MW, Zhang H, Li L, Tang PX, Chen W, et al. A cross-sectional study of GLIM-defined malnutrition based on new validated calf circumference cut-off values and different screening tools in hospitalised patients over 70 years old. J Nutr Health Aging. 2020;24:832–8.
Ottery FD. Rethinking nutritional support of the cancer patient: the new field of nutritional oncology. Semin Oncol. 1994;21:770–8.
Fu X, Tian Z, Wen S, Sun H, Thapa S, Xiong H, et al. A new index based on serum creatinine and cystatin C is useful for assessing sarcopenia in patients with advanced cancer. Nutrition. 2020;82:111032.
Gonzalez MC, Mehrnezhad A, Razaviarab N, Barbosa-Silva TG, Heymsfield SB. Calf circumference: cutoff values from the NHANES 1999–2006. Am J Clin Nutr. 2021;113:1679–87.
Funding
This work was funded by the National Key Research and Development Program (2017YFC1309200) and the National Natural Science Foundation of China (81673167).
Author information
Authors and Affiliations
Contributions
Conceptualization and study design: LYY, SYL, ZQG, HPS and HXX; investigation: LYY and HXX; data interpretation: LYY, LZ, NL, JG, LJL, XL, YF, JL, MYZ, FFC, XC, CW, XW, TTL, XLL, LD, WL, MY, JMY, XJW, XL, SMY, ZZ, KTY, MY, CHS, JWC, SYL, ZQG, HPS and HXX; statistical analysis: LYY; paper preparation: LYY. All authors have read and approved the final paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yin, L., Zhang, L., Li, N. et al. Several anthropometric measurements and cancer mortality: predictor screening, threshold determination, and joint analysis in a multicenter cohort of 12138 adults. Eur J Clin Nutr 76, 756–764 (2022). https://doi.org/10.1038/s41430-021-01009-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-021-01009-x
This article is cited by
-
Predicting intra-abdominal hypertension using anthropometric measurements and machine learning
Scientific Reports (2025)
-
The L-shaped association of mid-upper arm circumference with all-cause and cause-specific mortality in US adults: a population-based prospective cohort study
BMC Public Health (2023)
-
Comments on the methodology and completeness of a meta-analysis on the association between low calf circumference and mortality
European Geriatric Medicine (2022)
-
Calf Circumference and All-Cause Mortality: A Systematic Review and Meta-Analysis Based on Trend Estimation Approaches
The Journal of nutrition, health and aging (2022)