Abstract
Background
Lifestyle intervention is the mainstay therapy for Non-Alcoholic Fatty Liver Disease (NAFLD). We aimed to assess the efficacy of an intensive (9 contact points in 6 months) weight-loss intervention among patients with obesity (BMI 25–39.9 kg/m2) and NAFLD in north India.
Methods
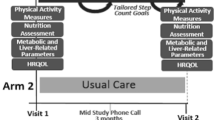
A total of 140 patients (18–60 years) with obesity and NAFLD were randomized into intervention (n = 70) and control (n = 70) groups, at a tertiary-care hospital. Weight, anthropometric parameters, Controlled Attenuation Parameter (CAP), Liver Stiffness Measurement (LSM), liver enzymes, grade of fatty liver and HOMA-IR were measured at baseline (T0) and 6 months (T6). There was a high drop-out, exacerbated by the Covid-19 pandemic. Completers comprised of 59 participants (n = 30 intervention, n = 29 control). Intention to treat analysis was done.
Results
At T6, ALT normalized in significantly higher (p = 0.03) number of cases in the intervention arm (66.7%) versus control arm (18.2%). No significant improvement was seen in other metabolic, ultrasound or anthropometric outcomes. Weight (p < 0.001), AST (p = 0.01), ALT (p = 0.02), body fat% (p < 0.001), WC (p < 0.001) and CAP (p < 0.001) significantly improved within the intervention arm along with a trend of improvement in steatosis and HOMA-IR. Control group showed significant decrease in weight (p < 0.001), WC (p < 0.001) and CAP (p = 0.02). Twice the number of patients in intervention arm (46.7%) lost ≥5% weight, compared to control arm (24.1%) (p = 0.07).
Conclusion
The intensive weight-loss intervention was not effective in improving the treatment outcomes among patients with obesity and NAFLD. However, given the potential of our intervention, we recommend larger trials with more intensive weight-loss interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Rinella ME, Sanyal AJ Management of NAFLD: a stage-based approach. Nature reviews Gastroenterology & hepatology. 2016;196–205. Available from: www.nature.com/nrgastro
Koutoukidis DA, Koshiaris C, Henry JA, Noreik M, Morris E, Manoharan I, et al. The effect of the magnitude of weight loss on non-alcoholic fatty liver disease: a systematic review and meta-analysis. Metabolism. 2021;115:154455. Available from https://pubmed.ncbi.nlm.nih.gov/33259835/
Koutoukidis DA, Jebb SA, Tomlinson JW, Cobbold JF, Aveyard P. Association of weight changes with changes in histological features and blood markers in nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2021;S1542-3565:00382–7. Available from https://pubmed.ncbi.nlm.nih.gov/33813074/
Ghaemi A, Taleban FA, Hekmatdoost A, Rafiei A, Hosseini V, Amiri Z, et al. How much weight loss is effective on nonalcoholic fatty liver disease? Hepat Mon.;13:15227. Available from:/pmc/articles/PMC3867211/?report=abstract
Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines: management of nonalcoholic fatty liver disease. Clin Mol Hepatol Korean Assoc Study Liver. 2013;19:325–48. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894432/
Yasutake K, Kohjima M, Kotoh K, Nakashima M, Nakamuta M, Enjoji M. Dietary habits and behaviors associated with nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:1756–67. Available from: /pmc/articles/PMC3930974/
Lim SL, Johal J, Ong KW, Han CY, Chan YH, Lee YM, et al. Lifestyle intervention enabled by mobile technology on weight loss in patients with nonalcoholic fatty liver disease: Randomized controlled trial. JMIR mHealth uHealth. 2020;8:e14802. Available from https://mhealth.jmir.org/2020/4/e14802
Centis E, Moscatiello S, Bugianesi E, Bellentani S, Fracanzani AL, Calugi S, et al. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J Hepatol. 2013;58:771–7.
Huang MA, Greenson JK, Chao C, Anderson L, Peterman D, Jacobson J, et al. One-year intense nutritional counseling results in histological improvement in patients with nonalcoholic steatohepatitis: a pilot study. Am J Gastroenterol. 2005;100:1072–81. Available from https://pubmed.ncbi.nlm.nih.gov/15842581/
Lazo M, Solga SF, Horska A, Bonekamp S, Diehl AM, Brancati FL, et al. Effect of a 12-month intensive lifestyle intervention on hepatic steatosis in adults with type 2 diabetes. Diabetes Care. 2010;33:2156–63. https://diabetesjournals.org/care/article/33/10/2156/28393/Effect-of-a-12-Month-Intensive-Lifestyle
Arora C, Malhotra A, Ranjan P, Vikram NK, Dwivedi SN, Singh N, et al. Perceived barriers and facilitators for adherence to lifestyle prescription: Perspective of obese patients with non alcoholic fatty liver disease from north India. Diabetes Metab Syndr Clin Res Rev. 2021;15:102138.
Bhat G, Baba CS, Pandey A, Kumari N, Choudhuri G. Life style modification improves insulin resistance and liver histology in patients with non-alcoholic fatty liver disease. World J Hepatol. 2012;4:209–17. Available from: /pmc/articles/PMC3409355/?report=abstract
Paul J, Venugopal RV, Peter L, Hussain S, Naresh Kumar Shetty K, Shetti MP. Effects of lifestyle modification on liver enzyme and Fibroscan in Indian patients with non-alcoholic fatty liver disease. Gastroenterol Rep. 2018;6:49–53. Available from https://academic.oup.com/gastro/article/6/1/49/3829870
Arora C, Malhotra A, Ranjan P, Vikram NK, Shalimar, Singh N, et al. Lifestyle intervention framework for obese patients with non-alcoholic fatty liver disease—a tool for health professionals in resource constraint settings. Cureus. 2019;11:e5999. Available from: /pmc/articles/PMC6876900/?report=abstract
Shalimar, Kumar R, Rout G, Kumar R, Yadav R, Das P, et al. Body mass index–based controlled attenuation parameter cutoffs for assessment of hepatic steatosis in non-alcoholic fatty liver disease. Indian J Gastroenterol. 2020;39:32–41. Available from https://link.springer.com/article/10.1007/s12664-019-00991-2
Dong F, Zhang Y, Huang Y, Wang Y, Zhang G, Hu X, et al. Long-term lifestyle interventions in middle-aged and elderly men with nonalcoholic fatty liver disease: a randomized controlled trial. Sci Rep. 2016;6:1–8. Available from www.nature.com/scientificreports/
Mundi MS, Velapati S, Patel J, Kellogg TA, Abu Dayyeh BK, Hurt RT. Evolution of NAFLD and Its Management [Internet]. Nutr Clin Pract. 2020;35:72–84. Available from https://aspenjournals.onlinelibrary.wiley.com/doi/full/10.1002/ncp.10449
Konerman MA, Walden P, Joseph M, Jackson EA, Lok AS, Rubenfire M. Impact of a structured lifestyle programme on patients with metabolic syndrome complicated by non-alcoholic fatty liver disease. Aliment Pharm Ther. 2019;49:296–307. Available from https://onlinelibrary.wiley.com/doi/full/10.1111/apt.15063
Thomas EL, Brynes AE, Hamilton G, Patel N, Spong A, Goldin RD, et al. Effect of nutritional counselling on hepatic, muscle and adipose tissue fat content and distribution in non-alcoholic fatty liver disease. World J Gastroenterol. 2006;12:5813–9. Available from: /pmc/articles/PMC4100662/
Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–9. Available from https://aasldpubs.onlinelibrary.wiley.com/doi/full/10.1002/hep.23276
Kim WR, Flamm SL, Di Bisceglie AM, Bodenheimer HC. Serum activity of alanine aminotransferase (ALT) as an indicator of health and disease. Hepatology. 2008;47:1363–70. Available from www.interscience.wiley.com
Eddowes PJ, Sasso M, Allison M, Tsochatzis E, Anstee QM, Sheridan D, et al. Accuracy of fibroscan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease.Gastroenterology. 2019;156:1717–30. Available from https://doi.org/10.1053/j.gastro.2019.01.042.
Armandi A, Schattenberg JM. Beyond the paradigm of weight loss in non-alcoholic fatty liver disease: from pathophysiology to novel dietary approaches. Nutrients. 2021;13:1977. Available from https://www.mdpi.com/2072-6643/13/6/1977
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, et al. Clinical-liver weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. 2015; Available from: https://doi.org/10.1053/j.gastro.2015.04.005
Hallsworth K, Avery L, Trenell MI. Targeting lifestyle behavior change in adults with nafld during a 20-min consultation: summary of the dietary and exercise literature. Curr Gastroenterol Rep. 2016;18:11.
Bellentani S, Dalle Grave R, Suppini A, Marchesini G, Bedogni G, Bugianesi E, et al. Behavior therapy for nonalcoholic fatty liver disease: The need for a multidisciplinary approach. Hepatology. 47;746–54. Available from: https://aasldpubs.onlinelibrary.wiley.com/doi/full/10.1002/hep.22009
Mazzotti A, Caletti MT, Brodosi L, Di Domizio S, Forchielli ML, Petta S, et al. An internet-based approach for lifestyle changes in patients with NAFLD: two-year effects on weight loss and surrogate markers. J Hepatol. 2018;69:1155–63.
Scragg J, Avery L, Cassidy S, Taylor G, Haigh L, Boyle M, et al. Feasibility of a very low calorie diet to achieve a sustainable 10% weight loss in patients with nonalcoholic fatty liver disease. Clin Transl Gastroenterol. 2020;11:e00231. Available from https://pubmed.ncbi.nlm.nih.gov/33094956/
Acknowledgements
We acknowledge University Grants Commission for providing Junior Research fellowship to Mrs. Charu Arora. [(UGC Reference number- 1332 (NET-DEC 2014))].
Author information
Authors and Affiliations
Contributions
CA: Data collection, data analysis, writing of the manuscript; AM: concept and design of the paper, data analysis and interpretation, critically reviewing and finalizing the manuscript; PR: Corresponding author, concept and design of the paper, finalization of the paper; VS: Statistical analysis and data interpretation, critically revising the manuscript; NS: Data collection, analysis and interpretation of dietary data; Shalimar: Data collection, critical review of paper; SND: Critical review of paper; NKV: Revising and reviewing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Institute Ethics Committee (IEC- 434/04.08.2017).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Arora, C., Malhotra, A., Ranjan, P. et al. Effect of intensive weight-loss intervention on metabolic, ultrasound and anthropometric parameters among patients with obesity and non-alcoholic fatty liver disease: an RCT. Eur J Clin Nutr 76, 1332–1338 (2022). https://doi.org/10.1038/s41430-022-01111-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-022-01111-8
This article is cited by
-
A comprehensive approach to lifestyle intervention based on a calorie-restricted diet ameliorates liver fat in overweight/obese patients with NAFLD: a multicenter randomized controlled trial in China
Nutrition Journal (2024)
-
Asian Perspective of Nutrition in Liver Disease
Current Hepatology Reports (2022)