Abstract
Background
Chrononutrition studies suggest that eating later and extending the eating window are linked to higher energy intake and obesity. However, the relationship between chrononutrition variables and dietary intake, as well as with BMI, is still little explored at a population level. This study explored how chrononutrition variables relate to dietary intake and BMI at a population level.
Methods
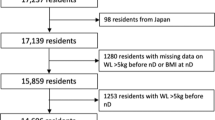
We analyzed data from the NHANES 2017–2018, including 2937 participants aged 18 years or older. Dietary intake was assessed by two 24-h dietary recalls. Caloric midpoint, eating window duration, sleep end-first meal and last meal-sleep onset intervals were determined by mealtime.
Results
The findings indicate a trend of increased total consumption of energy (kcal) (p < 0.001; p < 0.001; p < 0.001; p < 0.001), carbohydrates (g) (p = 0.001; p < 0.001; p < 0.001; p < 0.001); protein (g) (p < 0.001; p = 0.008; p < 0.001; p < 0.001), fat (g) (p < 0.001; p = 0.007; p < 0.001; p < 0.001), and sugar (g) (p < 0.001; p < 0.001; p < 0.001; p < 0.001) as the sleep end-first meal interval decreases and the last meal-sleep onset interval, eating window, and energy intake after 8 pm increases, respectively. In addition, our findings suggest a trend of increased BMI in the group with BMI ≥ 30 kg/m² (p = 0.018) as sleep end-first meal interval increases and in the group with BMI < 25 kg/m² (p = 0.006) as the eating window increases.
Conclusion
Our findings suggest that eating later and having longer eating window are associated with higher dietary intake and higher BMI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data from the study can be found on the publicly accessible NHANES website, and additional data are available from the corresponding author upon reasonable request.
References
Oike H, Oishi K, Kobori M. Nutrients clock genes, and chrononutrition. Curr Nutr Rep. 2014;3:204–12.
Oda H. Chrononutrition. J Nutr Sci Vitaminol. 2015;61:S92–S94.
Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity. 2013;21:2504–12.
Varady KA. Meal frequency and timing: impact on metabolic disease risk. Curr Opin Endocrinol Diab Obes. 2016;23:379–83.
Fong M, Caterson ID, Madigan CD. Are large dinners associated with excess weight, and does eating a smaller dinner achieve greater weight loss? A systematic review and meta-analysis. Br J Nutr. 2017;118:616–28.
Roenneberg TC, Kumar J, Merrow M. The human circadian clock entrains to sun time. Curr Biol. 2007;17:R44–R45. https://doi.org/10.1016/j.cub.2006.12.011
Crispim CA, Mota MC. New perspectives on chrononutrition. Biol Rhythm Res. 2019;50:63–77. https://doi.org/10.1080/09291016.2018.1491202
Teixeira GP, Barreto, ACF, Mota MC & Crispim CA. Caloric midpoint is associated with total calorie and macronutrient intake and body mass index in undergraduate students. Chronobiol Int. 2019. https://doi.org/10.1080/07420528.2019.1652830
Teixeira GP, Mota MC, Crispim CA. Eveningness is associated with skipping breakfast and poor nutritional intake in Brazilian undergraduate students. Chronobiol Int. 2018;35:358–67. https://doi.org/10.1080/07420528.2017.1407778
Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that canbe modulated for health benefits. Cell Metab. 2015;22:789–98. https://doi.org/10.1016/j.cmet.2015.09.005
Teixeira GP, da Cunha NB, Azeredo CM, Rinaldi AEM, Crispim CA. Eating time variation from weekdays to weekends and its association with dietary intake and BMI in different chronotypes: findings from National Health and Nutrition Examination Survey (NHANES) 2017-2018. Br J Nutr. 2024;131:1281–88. https://doi.org/10.1017/S0007114523002738.
Zerón-Rugerio MF, Hernáez A, Porras-Loaiza AP, Cambras T, Izquierdo-Pulido M. Eating Jet Lag: A Marker of the Variability in Meal Timing and Its Association with Body Mass Index. Nutrients. 2019;11:2980.
Crispim CA, Rinaldi AEM, Azeredo CM, Skene DJ, Moreno CRC. Is time of eating associated with BMI and obesity? A population-based study. Eur J Nutr. 2023;63:527–37.
Cunha NB, Teixeira GP, Rinaldi AEM, Azeredo CM, Crispim CA. Late meal intake is associated with abdominal obesity and metabolic disorders related to metabolic syndrome: A chrononutrition approach using data from NHANES 2015–2018. Clin Nutr. 2023;42:1798–805. https://doi.org/10.1016/j.clnu.2023.08.005.
Vujović N, Piron MJ, Qian J, Chellappa SL, Nedeltcheva A, Barr D, et al. Late isocaloric eating increases hunger, decreases energy expenditure, and modifies metabolic pathways in adults with overweight and obesity. Cell Metab. 2022;34:1486–1498.e7. https://doi.org/10.1016/j.cmet.2022.09.007.
Silva CM, Teixeira BS, Wright KP Jr, Maia YCDP, Crispim CA. Time-related eating patterns are associated with the total daily intake of calories and macronutrients in day and night shift workers. Nutrients. 2022;14:2202.
Farsijani S, Mao Z, Cauley JA, Newman AB. Comprehensive assessment of chrononutrition behaviors among nationally representative adults: Insights from National Health and Nutrition Examination Survey (NHANES) data. Clin Nutr. 2023;42:1910–21.
WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Tech Rep Ser 894, World Health Organ; 2000, pp. 1–253.
Togo P, Osler M, Sørensen TIA, Heitmann BL. Food intake patterns and body mass index in observational studies. Int J Obes Relat Metab Disord. 2001;25:1741–51. https://doi.org/10.1038/sj.ijo.0801819
Willett WC, Howe GR, Kushi LW. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–8S.
Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL. The relationship between breakfast skipping, chronotype, and glycemic control in type 2 diabetes. Chronobiol Int. 2014;31:64–71. https://doi.org/10.3109/07420528.2013.821614
McHill AW, Phillips AJK, Czeisler CA, Keating L, Yee K, Barger LK, et al. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr. 2017;106:1213–9. https://doi.org/10.3945/ajcn.117.161588.
Gontijo CA, Balieiro LCT, Teixeira GP, Fahmy WM, Crispim CA, Maia YCP. Higher energy intake at night effects daily energy distribution and contributes to excessive weight gain during pregnancy. Nutrition. 2020;74:110756. https://doi.org/10.1016/j.nut.2020.110756. Jun
De Castro JM. The time of day of food intake influences overall intake in humans. J Nutr. 2004;134:104–11. https://doi.org/10.1093/jn/134.1.104
Bui C, Lin L-Y, Wu C-Y, Chiu Y-W, Chiou H-Y. Association between Emotional Eating and Frequency of Unhealthy Food Consumption among Taiwanese Adolescents. Nutrients. 2021;13:2739. https://doi.org/10.3390/nu13082739
Jabs J, Devine CM. Time scarcity and food choices: an overview. Appetite. 2006;47:196–204. https://doi.org/10.1016/j.appet.2006.02.014.
Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14:21–8. https://doi.org/10.1111/obr.12107.
Mills S, White M, Brown H, Wrieden W, Kwasnicka D, Halligan J, et al. Health and social determinants and outcomes of home cooking: A systematic review of observational studies. Appetite. 2017;111:116–34. https://doi.org/10.1016/j.appet.2016.12.022
Marot LP, Rosa DE, Lopes TVC, Moreno CRC & Crispim CA. Eating Duration throughout a Rotating Shift Schedule: A Case Study. J Am Coll Nutr. 2020;1–8. https://doi.org/10.1080/07315724.2020.1814899
Garaulet M, Lopez-Minguez J, Dashti HS, Vetter C, Hernández-Martínez AM, Pérez-Ayala M, et al. Interplay of Dinner Timing and MTNR1B Type 2 Diabetes Risk Variant on Glucose Tolerance and Insulin Secretion: A Randomized Crossover Trial. Diab Care. 2022;45:512–9. https://doi.org/10.2337/dc21-1314.
Jakubowicz D, Wainstein J, Tsameret S, Landau Z. Role of High Energy Breakfast “Big Breakfast Diet” in Clock Gene Regulation of Postprandial Hyperglycemia and Weight Loss in Type 2 Diabetes. Nutrients. 2021;13:1558 10.3390/nu13051558.
Thomas EA, Zaman A, Cornier MA, Catenacci VA, Tussey EJ, Grau L, et al. Later Meal and Sleep Timing Predicts Higher Percent Body Fat. Nutrients. 2021;13:73 https://doi.org/10.3390/nu13010073
Croezen S, Visscher TL, Ter Bogt NC, Veling ML, Haveman-Nies A. Skipping breakfast, alcohol consumption and physical inactivity as risk factors for overweight and obesity in adolescents: Results of the E-MOVO project. Eur JClin Nutr. 2009;63:405–12. https://doi.org/10.1038/sj.ejcn.1602950
Garaulet M, Gómez-Abellán P, Alburquerque-Béjar JJ, Lee YC, Ordovás JM, Scheer FA. Timing of food intake predicts weight loss effectiveness. Int J Obes. 2013;37:604–611. https://doi.org/10.1038/ijo.2012.229.
Crispim CA, Rinaldi AE, Azeredo CM, Skene DJ, Moreno CR. Is time of eating associated with BMI and obesity? A population-based study. Eur J Nutr. 2024;63:527–37.
Dashti HS, Gómez-Abellán P, Qian J, Esteban A, Morales E, Scheer F, et al. Late eating is associated with cardiometabolic risk traits, obesogenic behaviors, and impaired weight loss. Am J Clin Nutr. 2021;113:154–61. https://doi.org/10.1093/ajcn/nqaa264.
Hatamoto Y, Tanoue Y, Yoshimura E, Matsumoto M, Hayashi T, Ogata H, et al. Delayed eating schedule raises mean glucose levels in young adult males: a randomized controlled cross-over trial. J Nutr. 2023;153:1029–37.
Davis C, Bonham MP, Kleve S, Dorrian J, Huggins CE. Evaluation of the “Shifting Weight using Intermittent Fasting in night-shift workers” weight loss interventions: a mixed-methods protocol. Front Public Health. 2023;11:1228628.
Abdulla NK, Obaid RR, Qureshi MN, Asraiti AA, Janahi MA, Qiyas SJA et al. Relationship between hedonic hunger and subjectively assessed sleep quality and perceived stress among university students: A cross-sectional study. Heliyon. 2023:9:e14987.
Vidafar P, SW Cain, Shechter A. Relationship between sleep and hedonic appetite in shift workers. Nutrients. 2020;12:2835.
Kakinami L, O’Loughlin EK, Brunet J, Dugas EN, Constantin E, Sabiston CM, et al. Associations between physical activity and sedentary behavior with sleep quality and quantity in young adults. Sleep Health. 2017;3:56–61.
Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26.
Guimarães KC, Silva CM, Latorraca COC, Oliveira RÁ, Crispim CA. Is self-reported short sleep duration associated with obesity? A systematic review and meta-analysis of cohort studies. Nutr Rev. 2022;80:983–1000. https://doi.org/10.1093/nutrit/nuab064.
Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. https://doi.org/10.7326/0003-4819-141-11-200412070-00008.
Funding
This work was supported by the CAPES/CNPq. CAC is CNPq fellow: #401761/2022-3. CMA receives support from CNPq grant: 313491/2021-6.
Author information
Authors and Affiliations
Contributions
CAC and GPT participated in the planning, interpretation of results and writing of the manuscript. GPT and NBC extracted the data. GPT performed the statistical analysis. AEMR, CMA, and NBC participated in the interpretation of results, support on the statistical analysis and writing of the manuscript. All authors provided feedback and approved the final version of the manuscript submitted for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
NHANES is a public dataset and all participants provided a written informed consent, consistent with approval from the National Center for Health Statistics Research Ethics Review Board (NCHS ERB) (protocol #2018-01 for NHANES cycle 2017–2018).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Teixeira, G.P., da Cunha, N.B., Azeredo, C.M. et al. Association of meal time patterns with dietary intake and body mass index: a chrononutrition approach from NHANES 2017-2018. Eur J Clin Nutr 79, 748–755 (2025). https://doi.org/10.1038/s41430-025-01603-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01603-3