Abstract
Objective
We assessed the effectiveness of weekly iron and semestrial high-dose vitamin A supplementation on hemoglobin (Hb) concentration, and iron and vitamin A status of schoolchildren in rural Ethiopia.
Method
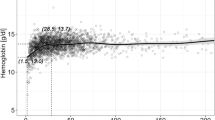
Using a 2 × 2 factorial design, 504 schoolchildren aged 7–10 years were randomly assigned to one of the four arms: control placebo; high-dose vitamin A; iron; or iron and high-dose vitamin A. Semestrial 200,000 IU vitamin A and weekly 42 mg of iron supplement were provided for 11 months. At baseline and at endline, Hb and serum concentrations of ferritin (sF), soluble transferrin receptor (sTfR), and retinol-binding protein (RBP) were measured. Serum indicators were adjusted for inflammation indicators, while Hb was adjusted for village altitude. Total body iron was calculated from sTfR and sF concentrations using an established formula.
Result
At baseline, prevalence of anemia (Hb < 11.0 g/dL), iron deficiency (sTfR > 8.3 mg/L or sF < 15 μg/L), iron-deficiency anemia, and vitamin A deficiency (RBP < 0.7 μmol/L) were 27.8%, 21.7%, 6.3% and 12.2%, respectively. Both iron and vitamin A supplementation had no significant effect on Hb, sTfR, and RBP concentrations. Supplementing iron weekly significantly increased sF (6.86 μg/L, 95%CI: 1.67, 12.05) and total body iron (0.45 mg/Kg, 95%CI: 0.17, 0.74), while semestrial vitamin A supplementation had no significant effect on both sF and total body iron.
Conclusion
Intermittent iron and vitamin A supplementation had no significant detectable effects on Hb, sTfR, and RBP concentrations of schoolchildren. Weekly iron supplementation improved sF concentrations. These findings suggest that providing iron and vitamin A supplements to populations where the extent of the deficiencies is not a major public health problem may not be beneficial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data used in this analysis are available at https://osf.io/nwh7f.
References
McLean E, Cogswell M, Egli I, Wojdyla D, De Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 2009;12:444–54.
Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615–24.
Safiri S, Kolahi A-A, Noori M, Nejadghaderi SA, Karamzad N, Bragazzi NL, et al. Burden of anemia and its underlying causes in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019. J Hematol Oncol. 2021;14:1–16.
Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian S. Anaemia in low-income and middle-income countries. Lancet. 2011;378:2123–35.
Gilles H, Williams EW, BALL PA. Hookworm infection and anaemia. An epidemiological, clinical, and laboratory Study. Q J Med. 1964;33:1–24.
Muckenthaler MU, Rivella S, Hentze MW, Galy B. A red carpet for iron metabolism. Cell. 2017;168:344–61.
Nairz M, Theurl I, Wolf D, Weiss G. Iron deficiency or anemia of inflammation? : Differential diagnosis and mechanisms of anemia of inflammation. Wien Med Wochenschr. 2016;166:411–23.
Bundy DA. Rethinking school health: a key component of education for all. World Bank Publications; 2011.
da Silva Lopes K, Yamaji N, Rahman MO, Suto M, Takemoto Y, Garcia-Casal MN, et al. Nutrition-specific interventions for preventing and controlling anaemia throughout the life cycle: an overview of systematic reviews. Cochrane Database Syst Rev. 2021;9:CD013092.
Gera T, Sachdev H, Nestel P, Sachdev SS. Effect of iron supplementation on haemoglobin response in children: systematic review of randomised controlled trials. J Pediatr Gastroenterol Nutr. 2007;44:468–86.
Stoltzfus RJ. Iron interventions for women and children in low-income countries. J Nutr. 2011;141:756s–62s.
Gross R, Angeles-Agdeppa I, Schultink WJ, Dillon D, Sastroamidjojo S. Daily versus weekly iron supplementation: programmatic and economic implications for Indonesia. Food Nutr Bull. 1997;18:64–70.
Baqui AH, Walker CLF, Zaman K, El Arifeen S, Chowdhury HR, Wahed MA, et al. Weekly iron supplementation does not block increases in serum zinc due to weekly zinc supplementation in Bangladeshi infants. J Nutr. 2005;135:2187–91.
Sazawal S, Black RE, Ramsan M, Chwaya HM, Stoltzfus RJ, Dutta A, et al. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: community-based, randomised, placebo-controlled trial. Lancet. 2006;367:133–43.
Raiten DJ, Namaste S, Brabin B. Considerations for the safe and effective use of iron interventions in areas of malaria burden—executive summary. Int J Vitam Nutr Res. 2011;81:57–71.
WHO. Guideline: intermittent iron supplementation in preschool and school-age children. Geneva, Switzerland: World Health Organization; 2011.
Government of FDRE. Federal Democratic Republic of Ethiopia National Food and Nutrition Strategy. Government of the Federal Democratic Republic of Ethiopia (FDRE); 2021.
Bruins M, Kraemer K. Public health programmes for vitamin A deficiency control. Community eye health. 2013;26:69–70.
Underwood BA. Prevention of vitamin A deficiency. In: Howson C, Kennedy E, Horwitz A, Committee on Micronutrient Deficiencies Institute of Medicine, editors. Prevention of micronutrient deficiencies: tools for policymakers and public health workers. Washington, D.C. : National Academy Press; 1998.p.103-66.
Mayo-Wilson E, Imdad A, Herzer K, Yakoob MY, Bhutta ZA. Vitamin A supplements for preventing mortality, illness, and blindness in children aged under 5: systematic review and meta-analysis. Bmj. 2011;343:d5094.
Madatuwa TM, Mahawithanage ST, Chandrika UG, Jansz ER, Wickremasinghe AR. Evaluation of the effectiveness of the national vitamin A supplementation programme among school children in Sri Lanka. Br J Nutr. 2007;97:153–9.
Zimmermann MB, Biebinger R, Rohner F, Dib A, Zeder C, Hurrell RF, et al. Vitamin A supplementation in children with poor vitamin A and iron status increases erythropoietin and hemoglobin concentrations without changing total body iron. Am J Clin Nutr. 2006;84:580–6.
FMoH. Second Edition of Ethiopia National Master Plan For Neglected Tropical Diseases. Federal Democratic Republic of Ethiopia Ministry of Health. Addis Ababa, Ethiopia. Addis Ababa: Federal Democratic Republic of Ethiopia Ministry of Health; 2016.
Negussu N, Mengistu B, Kebede B, Deribe K, Ejigu E, Tadesse G, et al. Ethiopia schistosomiasis and soil-transmitted helminthes control programme: progress and prospects. Ethiop Med J. 2017;55:75.
De-Regil LM, Jefferds MED, Sylvetsky AC, Dowswell T. Intermittent iron supplementation for improving nutrition and development in children under 12 years of age. Cochrane Database Syst Rev. 2011;1–274.
Leenstra T, Kariuki S, Kurtis J, Oloo A, Kager P, Ter Kuile F. The effect of weekly iron and vitamin A supplementation on hemoglobin levels and iron status in adolescent schoolgirls in western Kenya. Eur J Clin Nutr. 2009;63:173–82.
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, Switzerland: World Health Organization; 2011.
FMHACA. Standard treatment guidelines for general hospital. Food, Medicine and Healthcare Administration and Control Authority of Ethiopia, Addis Ababa, Ethiopia; 2014.
WHO. Guideline: vitamin A supplementation in infants and children 6–59 months of age. World Health Organization; 2011.
WHO. Preventive chemotherapy in human helminthiasis: coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. Geneva, Switzerland: World Health Organization; 2006.
Gutema BT, Levecke B, Sorrie MB, Megersa ND, Zewdie TH, Yesera GE, et al. Effectiveness of intermittent iron and high-dose vitamin A supplementation on cognitive development of school children in southern Ethiopia: a randomized placebo-controlled trial. Am J Clin Nutr. 2024;119:470–84.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JGA. metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208.
Harris PA, Delacqua G, Taylor R, Pearson S, Fernandez M, Duda SN. The REDCap Mobile Application: A data collection platform for research in regions or situations with internet scarcity. JAMIA open. 2021;4:ooab078.
CSA, ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia and Rockville, Maryland, USA: Central Statistical Agency of Ethiopia and ICF International; 2016.
Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. Washington, D.C.: Food and Nutrition Technical Assistance (FANTA); 2007. Version 3 p.
Belachew T, Lindstrom D, Gebremariam A, Hogan D, Lachat C, Huybregts L, et al. Food insecurity, food based coping strategies and suboptimal dietary practices of adolescents in Jimma zone Southwest Ethiopia. PloS one. 2013;8:e57643.
WHO. Bench aids for the diagnosis of intestinal parasites. 2nd ed. Geneva, Switzerland: World Health Organization; 2019.
Erhardt JG, Estes JE, Pfeiffer CM, Biesalski HK, Craft NE. Combined measurement of ferritin, soluble transferrin receptor, retinol binding protein, and C-reactive protein by an inexpensive, sensitive, and simple sandwich enzyme-linked immunosorbent assay technique. J Nutr. 2004;134:3127–32.
Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health policy Plan. 2006;21:459–68.
FAO, FHI 360. Minimum Dietary Diversity for Women: a Guide to Measurement. Rome: Food and Agriculture Organization of the United Nations and USAID’s Food and Nutrition Technical Assistance III Project (FANTA), managed by FHI 360; 2016.
WHO. WHO AnthroPlus for Personal Computers Manual: Software for assessing growth of the world’s children and adolescents. Geneva, Switzerland: World Health Organization; 2009.
WHO. Guideline on haemoglobin cutoffs to define anaemia in individuals and populations. Geneva, Switzerland: World Health Organization; 2024.
Thurnham DI, McCabe LD, Haldar S, Wieringa FT, Northrop-Clewes CA, McCabe GP. Adjusting plasma ferritin concentrations to remove the effects of subclinical inflammation in the assessment of iron deficiency: a meta-analysis. Am J Clin Nutr. 2010;92:546–55.
Thurnham DI, McCabe G, Northrop-Clewes C, Nestel P. Effects of subclinical infection on plasma retinol concentrations and assessment of prevalence of vitamin A deficiency: meta-analysis. Lancet. 2003;362:2052–8.
Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood, J Am Soc Hematol. 2003;101:3359–63.
WHO. Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Geneva, Switzerland: World Health Organization; 2011. Report No.: 00221899 (ISSN).
Mejía LA, Chew F. Hematological effect of supplementing anemic children with vitamin A alone and in combination with iron. Am J Clin Nutr. 1988;48:595–600.
Chen K, Zhang L, Luo HY, Wang J, Li Q, Mao M. No enhancing effect of vitamin A administration on iron absorption or body total iron content in preschool children from Chengdu, China. J Nutr Sci Vitaminol. 2014;60:223–30.
Soekarjo D, De Pee S, Kusin J, Schreurs W, Schultink W, Bloem M. Effectiveness of weekly vitamin A (10 000 IU) and iron (60 mg) supplementation for adolescent boys and girls through schools in rural and urban East Java, Indonesia. Eur J Clin Nutr. 2004;58:927–37.
Sen A, Kanani S. Intermittent iron folate supplementation: impact on hematinic status and growth of school girls. Int Sch Res Not. 2012;2012:482153.
Risonar M, Tengco L, Rayco-Solon P, Solon F. The effect of a school-based weekly iron supplementation delivery system among anemic schoolchildren in the Philippines. Eur J Clin Nutr. 2008;62:991–6.
Berger J, Aguayo V, Tellez W, Lujan C, Traissac P, Miguel JS. Weekly iron supplementation is as effective as 5 day per week iron supplementation in Bolivian school children living at high altitude. Eur J Clin Nutr. 1997;51:381–6.
Hall A, Roschnik N, Ouattara F, Touré I, Maiga F, Sacko M, et al. A randomised trial in Mali of the effectiveness of weekly iron supplements given by teachers on the haemoglobin concentrations of schoolchildren. Public Health Nutr. 2002;5:413–8.
Sungthong R, Mo-Suwan L, Chongsuvivatwong V, Geater AF. Once weekly is superior to daily iron supplementation on height gain but not on hematological improvement among schoolchildren in Thailand. J Nutr. 2002;132:418–22.
Roschnik N, Parawan A, Baylon MAB, Chua T, Hall A. Weekly iron supplements given by teachers sustain the haemoglobin concentration of schoolchildren in the Philippines. Trop Med Int Health. 2004;9:904–9.
Aguayo V. School-administered weekly iron supplementation—effect on the growth and hemoglobin status of non-anemic Bolivian school-age children A randomized placebo-controlled trial. Eur J Nutr. 2000;39:263–9.
Taylor M, Jinabhai C, Couper I, Kleinschmidt I, Jogessar V. The effect of different anthelmintic treatment regimens combined with iron supplementation on the nutritional status of schoolchildren in KwaZulu-Natal, South Africa: a randomized controlled trial. Trans R Soc Trop Med Hyg. 2001;95:211–6.
Olsen A, Nawiri J, Magnussen P, Krarup H, Friis H. Failure of twice-weekly iron supplementation to increase blood haemoglobin and serum ferritin concentrations: results of a randomized controlled trial. Ann Trop Med Parasitol. 2006;100:251–63.
da Cunha MdSB, Hankins NAC, Arruda SF. Effect of vitamin A supplementation on iron status in humans: A systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2019;59:1767–81.
Al-Mekhlafi HM, Al-Zabedi EM, Al-Maktari MT, Atroosh WM, Al-Delaimy AK, Moktar N, et al. Effects of vitamin A supplementation on iron status indices and iron deficiency anaemia: a randomized controlled trial. Nutrients. 2013;6:190–206.
Silva-Neto RibeiroLG, Neto JEdS, Florêncio. TMdMT. Association between vitamin A supplementation and stunting and anemia in socially vulnerable Brazilian children. Eur J Nutr. 2024;63:3281–8.
Bloem MW, Wedel M, van Agtmaal EJ, Speek AJ, Saowakontha S, Schreurs WH. Vitamin A intervention: short-term effects of a single, oral, massive dose on iron metabolism. Am J Clin Nutr. 1990;51:76–9.
Khan I, Baseer A. Hematologic effect of vitamin A supplementation in anemic Pakistani children. J Pak Med Assoc. 1996;46:34–8.
Mahawithanage ST, Kannangara KK, Wickremasinghe R, Chandrika UG, Jansz ER, Karunaweera ND, et al. Impact of vitamin A supplementation on health status and absenteeism of school children in Sri Lanka. Asia Pac J Clin Nutr. 2007;16:94–102.
Awasthi S, Peto R, Read S, Clark S, Pande V, Bundy D, et al. Vitamin A supplementation every 6 months with retinol in 1 million pre-school children in north India: DEVTA, a cluster-randomised trial. Lancet. 2013;381:1469–77.
Cusick SE, Tielsch JM, Ramsan M, Jape JK, Sazawal S, Black RE, et al. Short-term effects of vitamin A and antimalarial treatment on erythropoiesis in severely anemic Zanzibari preschool children. Am J Clin Nutr. 2005;82:406–12.
Gholizadeh M, Basafa Roodi P, Abaj F, Shab-Bidar S, Saedisomeolia A, Asbaghi O, et al. Influence of Vitamin A supplementation on inflammatory biomarkers in adults: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2022;12:21384.
Citelli M, Bittencourt LL, Da Silva SV, Pierucci APT, Pedrosa C. Vitamin A modulates the expression of genes involved in iron bioavailability. Biol trace Elem Res. 2012;149:64–70.
Schroeder SE, Reddy MB, Schalinske KL. Retinoic acid modulates hepatic iron homeostasis in rats by attenuating the RNA-binding activity of iron regulatory proteins. J Nutr. 2007;137:2686–90.
Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372:1832–43.
Gutema BT, Levecke B, Henauw SD, Abbeddou S. Burden of undernutrition and factors associated with nutritional status among schoolchildren in Southern Ethiopia: a school-based cross-sectional study. Manuscript under preparation. 2025.
Andersen CT, Tadesse AW, Bromage S, Fekadu H, Hemler EC, Passarelli S, et al. Anemia etiology in Ethiopia: assessment of nutritional, infectious disease, and other risk factors in a population-based cross-sectional survey of women, men, and children. J Nutr. 2022;152:501–12.
Amare B, Moges B, Fantahun B, Tafess K, Woldeyohannes D, Yismaw G, et al. Micronutrient levels and nutritional status of school children living in Northwest Ethiopia. Nutr J. 2012;11:108.
Desalegn A, Mossie A, Gedefaw L. Nutritional iron deficiency anemia: magnitude and its predictors among school age children, southwest Ethiopia: a community based cross-sectional study. PloS one. 2014;9:e114059.
Semba RD, Muhilal M, West KP Jr, Winget M, Natadisastra G, Scott A, et al. Impact of vitamin A supplementation on hematological indicators of iron metabolism and protein status in children. Nutr Res. 1992;12:469–78.
Semba R, Bloem M. The anemia of vitamin A deficiency: epidemiology and pathogenesis. Eur J Clin Nutr. 2002;56:271–81.
Palmer AC, West KP Jr., Dalmiya N, Schultink W. The use and interpretation of serum retinol distributions in evaluating the public health impact of vitamin A programmes. Public Health Nutr. 2012;15:1201–15.
Luo H, Geng J, Zeiler M, Nieckula E, Sandalinas F, Williams A, et al. A practical guide to adjust micronutrient biomarkers for inflammation using the BRINDA method. J Nutr. 2023;153:1265–72.
Acknowledgements
We would like to thank the children who participated in this study, their parents/guardians, school teachers, health extension workers of the village, district health and education offices, and the research team who made this study possible.
Funding
This work was conducted under the PhD studies of BTG, whose scholarship was partially funded by the Flemish Interuniversity Council (VLIR-UOS) in the context of the Institutional University Cooperation Program (IUC) with Arba Minch University https://www.vliruos.be/en/projects/project/22?pid=3604. Iron and iron-placebo supplements were produced and donated by Metagenics (Belgium, https://www.metagenics.eu/en_EU/). Vitamin A supplements and RDT kits were obtained from the Arba Minch town and Arba Minch Zuria district health offices. The funders had no role in the study design, data collection and analysis, decision to publish, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
The authors’ contributions were as follows—SA, SDH, and BTG were responsible for the design of the study. BL trained the staff at Arba Minch University on the Kato Katz technique. BTG, MBS, SBB, EZT, WGB, THZ, and TY conducted the research and SA, BL, and BTG supervised data collection. BTG completed the statistical analyses and drafted the manuscript. SA contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki, and all procedures were approved by the Commission on Medical Ethics of Ghent University Hospital, Ghent, Belgium (EC/2019/1289) and by the National Research Ethics Review Committee of the Ministry of Science and Higher Education, Ethiopia (P.S.M/14.1/505/20). The study is registered on clinicaltrials.gov with the reference number NCT04137354 (https://clinicaltrials.gov/study/NCT04137354). Letters of permission were written for district administrations, district health and education offices, kebele leaders, and school directors. Following contact with school directors, a sensitization workshop was organized for directors, teachers, and parents. Informed written consent for the children’s participation was obtained from their parents, and assent was obtained from the children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41430_2025_1678_MOESM1_ESM.docx
Supplemental tables for subgroup analysis using baseline characteristics of the study participants to investigate the effectiveness of the supplementation intervention on outcomes
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gutema, B.T., Sorrie, M.B., Belayneh, S.B. et al. Effectiveness of intermittent iron and high-dose vitamin A supplementation on hemoglobin, iron and vitamin A status of schoolchildren in southern Ethiopia: a randomized placebo controlled trial. Eur J Clin Nutr (2025). https://doi.org/10.1038/s41430-025-01678-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41430-025-01678-y