Abstract
Structural variants (SVs) of the nebulin gene (NEB), including intragenic duplications, deletions, and copy number variation of the triplicate region, are an established cause of recessively inherited nemaline myopathies and related neuromuscular disorders. Large deletions have been shown to cause dominantly inherited distal myopathies. Here we provide an overview of 35 families with muscle disorders caused by such SVs in NEB. Using custom Comparative Genomic Hybridization arrays, exome sequencing, short-read genome sequencing, custom Droplet Digital PCR, or Sanger sequencing, we identified pathogenic SVs in 35 families with NEB-related myopathies. In 23 families, recessive intragenic deletions and duplications or pathogenic gains of the triplicate region segregating with the disease in compound heterozygous form, together with a small variant in trans, were identified. In two families the SV was, however, homozygous. Eight of these families have not been described previously. In 12 families with a distal myopathy phenotype (of which 10 are previously unpublished), eight unique, large deletions encompassing 52–97 exons in either heterozygous (n = 10) or mosaic (n = 2) state were identified. In the families where inheritance was recessive, no correlation could be made between the types of variants and the severity of the disease. In contrast, all patients with large dominant deletions in NEB had milder, predominantly distal muscle weakness. For the first time, we establish a clear and statistically significant association between large NEB deletions and a form of distal myopathy. In addition, we provide the hitherto largest overview of the spectrum of SVs in NEB.
Similar content being viewed by others
Introduction
The nebulin gene
Nebulin (NEB, HGNC:7720, MIM ID *161650, genomic location 2q23.3) is a large protein expressed in the skeletal muscle sarcomere, integral to its structure and function. Its 183 exons span a genomic region over 250 kb, giving it a theoretical full-length mRNA of 26 kb, encoding more than 8600 amino acids with a combined molecular weight of approximately 990 kDa.
Exons 63–66, 143–144, and 167–177 of NEB undergo alternative splicing, giving rise to various nebulin isoforms [1, 2]. In addition, exons 82–105 constitute an intragenic segmental duplication region, referred to as the triplicate region (NEB TRI). This region consists of a 10 kb, eight-exon block repeated three times (exons 82–89, 90–97, 98–105), at 99% identity between the repeats; thus, the normal number of eight-exon blocks in a diploid genome is six [1].
The C-terminal end of nebulin encodes a Z-disc anchor, while the N-terminus is located in the pointed cap end of the thin filament [3, 4]. The full-length protein consists of 29 actin-binding super repeats, each composed of seven simple actin-binding motifs (SDxxYK), allowing the protein to potentially bind to more than 200 actin monomers. The super repeats closer to the Z-disc and the cap end bind actin with a stronger affinity than the super repeats in the middle of the protein [5]. Each NEB TRI eight-exon block encodes for two super repeats, resulting in six super repeats in total in the wildtype allele TRI region [6]. It was previously hypothesized that each super repeat also contains a tropomyosin-binding site (WLKGIGW) [1, 3]. However, it has recently been shown that nebulin and tropomyosin do not directly bind to each other [7]. Instead, the WLKGIGW motif and an ExxK motif in nebulin seem to interact with the linker region of troponin T [7]. The large number of nebulin isoforms is thought to contribute to the regulation of thin filament length and Z-disc structure in different fiber types and under differing physiological conditions [8,9,10].
Nebulin stiffens the thin filament and is critical for the generation of physiological force levels [11]. The thin filament can be assembled in the absence of nebulin [12, 13], but its absence results in shorter actin filaments, impaired tropomyosin/troponin movement on the thin filament, altered cross-bridge formation, and lesser force [11, 14].
Variation in nebulin
To date, more than 800 variants in NEB have been recorded in the Leiden Open Variation Database v.3.0 (LOVD, April 25 2024) [15], and of these, 385 (46%) have been classified as pathogenic or likely pathogenic. The distribution between different pathogenic variant types recorded in LOVD is highly similar to that seen in our in-house data (Fig. 1).
A shows the distribution recorded in LOVD, and B shows the distribution in our in-house data. Full LOVD data are available in Supplementary Table 1. TRI: NEB triplicate region, exons 82–89, 90–97, 98–105; CNVs: copy number variants.
The Genome Aggregation Database (gnomAD, August 14 2024) SVs 4.1.0 holds 30 records of SVs in NEB over 50 bp in size encompassing at least one exon. The full data extracted from gnomAD SVs 4.1.0 is available in Supplementary Table 2, and more details about the data can be found in Supplementary File 1.
SVs in NEB may be divided into two categories: 1. NEB TRI copy number variants (NEB TRI CNVs), which refer to gains and losses limited to the NEB TRI region, 2. deletions and duplications over 50 bp outside the NEB TRI region, referred to here as structural variants (SVs). The NEB TRI CNVs and SVs represent1.5% and 5% of pathogenic variants in NEB in LOVD, respectively (Fig. 1, Supplementary Table 1).
While the loss or gain of one of the three repeated NEB TRI blocks per allele is considered a benign copy number polymorphism, gains of two or more blocks per allele are recessive pathogenic CNVs [6]. No losses of more than one block on one allele have been recorded. CNVs of the NEB TRI region are seen in up to 14% of congenital myopathy index patient samples (either heterozygous or homozygous), [16, 17] and approximately half of these are pathogenic [18]. To our knowledge, no inversions or translocations in NEB have been recorded to date.
To date, all single nucleotide variants (SNVs), small indels, and TRI CNVs described are recessive, while SVs in NEB can be divided into recessive and dominant SVs. Recessive SVs are either frameshifting or null-alleles, while the previously described dominant deletions are in-frame, allowing the expression of stable mini-nebulin proteins [6, 19,20,21,22]. In addition, a well-characterized recessive deletion of exon 55 is a known nemaline myopathy (NM)-causing founder variant identified in people of Ashkenazi Jewish population (prevalence 1:108) [23].
The nebulin gene and disease – a spectrum of myopathies
Pathogenic variants in NEB were first described in patients with congenital autosomal recessive (AR) NM type 2 (NEM2, MIM ID #256030) [8], but have since been found to cause other related congenital myopathies as well. Pathogenic variants in NEB are the most common cause of recessive NM [8, 23,24,25,26,27,28,29,30] and are responsible for roughly half of all cases [31, 32]. NM, in turn, is one of the most common of the rare congenital myopathies with an incidence of ~1 in 50,000 live births [31].
NMs are highly variable in severity, usually presenting as skeletal muscle weakness of early onset, predominantly present in the proximal limb, respiratory, facial, and trunk muscles, with a later distal involvement. The patients run a risk of insidious decrease in respiratory function. A hallmark identifier is ‘nemaline bodies’ in Gömöri trichrome-stained muscle biopsy sections [33]. These protein aggregates consist of accumulations of Z-disc and thin filament proteins. NEM2 can be caused by compound heterozygous or homozygous SNVs and indel variants in NEB, partial deletions or duplications of NEB, and copy number variants (CNVs) of the NEB TRI region. In addition, recessive NEB variants have been identified in patients with congenital myopathy with cap-like structures and nemaline bodies [34], core-rod myopathy [35], and lethal neonatal arthrogryposis multiplex congenita-6 (AMC6, MIM ID #619334) [36]. Distal forms of recessive myopathies with or without nemaline bodies, and core-rod myopathy have been reported. These vary in age of onset, and forms caused by biallelic NEB variants have been reported [19, 20, 37,38,39,40].
The same recessive NEB variant may in one patient be associated with NM, but in another patient, in combination with another recessive variant, cause another, related congenital myopathy [19, 20, 34, 36]. Variants in constitutional exons are most often associated with typical forms of NM, while variants in alternatively spliced exons are more common in patients with other or more unusual forms of NM [19].
Two families with distal phenotypes as a result of large dominant deletions in NEB have previously been described [21, 22]. One of these families had a dominantly inherited large deletion segregating in three generations, and in the second family, the index patient had a large de novo deletion in mosaic form. These patients with distal forms of NEB-related myopathies did not have decreased respiratory function, and in general the phenotype was milder.
In this article, we describe ten new families with distal phenotypes caused by six different large in-frame deletions, significantly expanding the number of large structural dominant variants identified in NEB. One of the new deletions presented existed in mosaic form. All these large dominant deletions were associated with a distal phenotype. We also present three new families with congenital myopathies caused by recessive SVs in NEB in combination with small variants, and five new families with pathogenic CNVs of the NEB TRI region. In addition, we review the published cases with large NEB SVs and CNVs of the NEB TRI region.
Materials & methods
Samples
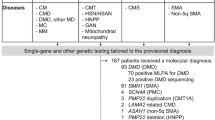
Altogether DNA samples from 35 families, and muscle biopsies from 3 families, were included in this study. The patient samples used were heterogeneous in terms of clinical diagnosis, ethnic background, and age. Altogether 22 families had a NM diagnosis: three of these classified as severe, seven as typical, one as mild, three as other/unusual forms, and in nine families the classification was unknown. In addition, the index patient of one family had core-rod myopathy. Milder distal myopathy was the primary diagnosis in 12 families.
DNA of index patients was extracted either from peripheral blood or cell lines (see Supplementary Tables 4–6), or muscle biopsy for analysis of degree of mosaicism (F24). For segregation analyses in unaffected family members, DNA was extracted from blood or saliva. DNA was eluted into TE buffer or water, and stored at −20 °C or −80 °C. The DNA concentration and quality were measured using DeNovix DS-11 FX+ Spectrophotometer/Fluorometer (DeNovix Inc., Wilmington, DE, USA). Subsequent dilutions were done in sterile water in appropriate series.
Genetic analysis methods
SVs and NEB TRI CNVs were identified and validated using different methods as described below. The samplewise methods are listed for samples with NEB TRI CNVs in Supplementary Table 4, for recessive NEB SVs in Supplementary Table 5, and for dominant NEB SVs in Supplementary Table 6. All NEB cDNA variants are identified relative to reference transcript NM_001271208.2, corresponding to protein reference sequence NP_001258137.2.
Comparative genomic hybridization array
Altogether DNA samples of 96 persons (50 healthy and 46 affected) from 33 families were run on a custom 4x180k or 8x60k comparative genomic hybridization array (NM- or NMD-CGH-array) as previously described [16, 17]. The degree of mosaicism of the patients with deletions in mosaic state (F24, F33) was determined as previously described [22].
Droplet digital PCR
For eleven samples from eight families with NEB TRI CNVs (F1, F3–F4, F7–F8, and F10–F12), custom droplet digital PCR (ddPCR) assays for the NEB TRI region were run as previously described [18].
Sequencing
The sequencing methods used included different short-read gene panels, exome sequencing (ES), short-read genome sequencing (GS), and Sanger sequencing.
Samples from families F26–F30 were subjected to a search for SNV/small indel identification protocol as previously described [41]. Subsequently, uncharacterized patient samples underwent CNV detection via a multi-method pipeline, which used cn.mops [42], clinCNV [43], and ExomeDepth [44] to explore potential CNVs. Filtration using the variant effect predictor (VEP) score [45] and control population frequencies (gnomAD and DGVgold) were used to remove known benign variants. Finally, the SARC R package [46] was used to remove detected CNVs with a low confidence score. Other SV types than CNVs were not possible to analyze from this data.
For F35, CANOES [47] was used to generate CNV calls from ES data.
Of the previously unpublished families, F23, F26–F27, and F31–F34 had undergone commercial or other diagnostic short-read sequencing for which details are not available.
Protein analysis
In two families (F24, F25), muscle-derived proteins were analyzed on western blot to study nebulin isoform expression, as previously described [21]. In F35, muscle-derived proteins were analyzed on western blot as described in Warren and colleagues [48], using mouse monoclonal antibodies against the nebulin super repeat 21, clone 9C4 (provided by Prof. Glenn Morris, Oswestry, UK) at 1:300 dilution and detected by enhanced chemiluminescence (ECL) (Supplementary File 1).
Statistical methods
All statistical tests were performed in RStudio 2022.02.1 build 461. Details concerning all statistical analyses are available in Supplementary File 2.
Correlation analysis between gene length and number of recorded SVs
The genomic gene length and number of structural variants recorded in gnomAD SVs 4.1.0 were extracted for 13 known NM-causing genes (Supplementary Table 3). The gene length was plotted against the number of recorded SVs using ggplot2 to verify normal distribution. The Pearson correlation coefficient and p-value were calculated.
Correlation analysis between different types of small variants and phenotype
Families with recessive heterozygous TRI CNVs and SVs and sufficient phenotypic data were classified into three groups: mild, typical, and severe, according to established classification criteria [49]. Small variants were divided into splicing, missense, and truncating variants, of which the latter includes both nonsense and frameshift variants. Families with homozygous NEB SVs (F20) and TRI CNVs (F12), and families in which severity classification was not possible (F2, F5, F13, F17, F19) were excluded from the statistical test. The correlation between the types of variants and the severity of the phenotype was tested with Fisher’s exact test.
Correlation analysis between pathogenic NEB TRI CNV allele and phenotype
In families with pathogenic gains of the NEB TRI region, the correlation between the copy number of the NEB TRI of the pathogenic allele and the severity of phenotype was tested using Kendall’s Tau.
Difference in deletion length between families with NM and distal phenotypes
The length of all unique deletions, both in recessive NM families (n = 7) and dominant distal myopathy families (n = 8), was extracted both in terms of number of affected exons and number of base pairs deleted. For deletions in which the exact breakpoints were unknown, the average length based on the CGH-array variant call was calculated by using the longest and shortest lengths indicated by the variant call in HGVS format. Data normality was assessed using the Shapiro–Wilk test, the homogeneity of variances was assessed post hoc using Levene’s test, and the Wilcoxon rank-sum test was used to compare the number of exons deleted and the length in basepairs between the recessive and dominantly segregating deletions. The difference between the groups was also assessed by an independent samples t-test.
Results
NEB TRI CNVs
We present 14 patients from 12 families (F1–F12) in whom pathogenic CNVs in the NEB TRI region were detected (Table 1, Supplementary Table 4), five of which are presented here for the first time. In one family (F12), the index patient was homozygous for a pathogenic TRI CNV (7 copies per allele). The other index cases were compound heterozygous for a NEB TRI CNV in combination with another type of pathogenic variant. The NEB TRI CNVs were identified using the NM- or NMD-CGH array in all 12 families, and the result was confirmed using custom ddPCR in eight families. The primary diagnosis of the patients with NEB TRI CNVs was NM confirmed by histopathological analyses and the severity of the disorder varied from mild to severe.
Recessive SVs
Ten unique recessive SVs in NEB have been identified in 11 families (F13–F23, Table 2, Supplementary Table 5). In nine families the patient’s SV was in trans with pathogenic SNVs or indels, while in F20 two affected siblings had the SV in homozygous form. The SVs and the second causative variants (SNVs or small indels) of the families and their respective associated phenotypes are presented in Table 2 and the SVs are visualized in Fig. 2. An extended overview including detection and verification methods and more variant and phenotype details is provided in Supplementary Table 5. As the families with the recessive exon 55 deletion [50] have previously been thoroughly described we do not present them in this article.
The patients in all the families presented here, except one with recessive NEB SVs, had been diagnosed with NM, with disease severity classified as mild, typical, or severe. In two families the phenotype could not be classified (F17 and F19), and in one family the muscle biopsy findings were consistent with core-rod myopathy (F13). The primary diagnoses of the patients with NM were confirmed by histopathological analyses and the severity of the disorder varied from mild to severe.
The largest recessive SV in NEB characterized to date is a deletion of exons 1–24 in F15, a patient with the severe form of NM. In addition, three different in-frame deletions (deletions of exons 43–45, 53–54, and 88–105) in four families (F16–F18 and F23) ranging from 2 to 18 exons in size have been identified. Two families (F16 and F17) share the same in-frame deletion of exons 43–45, but have different truncating NEB variants on the other allele. These families are seemingly unrelated but have the same country of origin.
Frameshift deletions affecting 1–3 exons leading to premature truncation of NEB were identified in families F19, F21, and F22. The second variants in these three families were also truncating.
In three families (F13, F14, F20), in-frame duplications of 18–89 exons in size were detected. The families with heterozygous duplications of exons 1–89 (F13) and 1–51 (F14) have been previously described [19, 29]. These patients had mild forms of NM (F14) and core-rod myopathy (F13). A previously unpublished duplication of exons 72–89 (F20) was found in homozygous form in two siblings in a consanguineous family, both affected by the severe form of NM.
In 9 out of 11 families, the SV was identified using the NMD-CGH-array, and in two families the preliminary finding was made by ES. For the latter, the breakpoints were subsequently verified using the NMD-CGH-array. In seven families the exact variant breakpoints were verified by Sanger sequencing as well, and in one, the finding was verified by multiplex ligation-dependent probe amplification (MLPA).
Dominant deletions
Large dominant NEB deletions have previously been reported in two separate families (F24 and F25) with distal nebulin myopathy. Here, we report 10 new families (F26–35) with distal myopathy caused by dominant deletions ranging from 52 to 98 exons in size (Table 3, Supplementary Table 6), all shown or predicted to be in-frame. The deletions are visualized in Fig. 2.
In the previously reported family F25, a deletion of exons 14–89 was identified in three generations. In F24 the de novo deletion of exons 11–107 was identified in mosaic form in a patient with asymmetry in muscle strength. Using western blot of muscle biopsy material, the allele with the deletion was shown to be expressed and to result in a significantly shorter nebulin protein product [21, 22] in affected members of both of these families.
In two of the previously unreported families, the deletion identified had occurred de novo. In F32, the heterozygous deletion of exons 33–107 (75 exons) was initially identified by ES and subsequently confirmed using the NMD-CGH-array. In F33, a patient presenting with asymmetry in muscle strength, the deletion of exons 39–133 (95 exons) was initially identified through a gene panel, and the finding was confirmed using the NMD-CGH-array, showing a degree of mosaicism of 60% in DNA extracted from blood. RNA sequencing of skeletal muscle mRNA from this patient’s diagnostic biopsy confirmed splicing of exon 38–134 in roughly half the transcripts (data not shown).
In eight families, the pathogenic deletion is seen in more than one family member, segregating with the disease in a dominant fashion. In five families (F26, F27, F28, F29, F30), a deletion of exons 14–77 (64 exons) was first identified either by a gene panel analysis or ES. In three of these, the deletion was also confirmed using the NMD-CGH-array. The families are not known to be related, but likely share a common ancestor. These families will be subject for another publication.
In family F31, a deletion of exons 14–81 (68 exons) was identified by ES in two patients, but not verified on the NMD-CGH-array, as no sample was available. It thus remains unclear whether the deletion extends further into the NEB TRI region. In family F34, a deletion of exons 47–114 (68 exons) was identified by short-read sequencing in the index patient, who presented with adult-onset muscle weakness. The deletion was subsequently shown to be present in their two affected children. In family F35, a deletion of exons 55–105 (51 exons) was confirmed in five patients presenting with mainly distal myopathy, with some proximal involvement and scapular winging. The expression of a shorter protein product in muscle was subsequently shown by a western blot analysis (Supplementary File 1).
All patients with large dominant deletions in NEB presented with mild phenotypes and primarily distal involvement, with facial and proximal involvement along with scapular winging present in some patients. All of these patients were ambulatory. While no nemaline bodies were reported, muscle fiber atrophy, fiber size abnormalities, type 1 fiber predominance, and/or central core regions have been noted in the histological analyses in families F24, F25, and F35.
Statistical analyses
The Pearson correlation coefficient between the gene length of NM-causing genes and number of recorded SVs in gnomAD SVs 4.1.0 was 0.982 (p = 2.534*10−9).
In this cohort, no statistically significant correlation was found between the type of small variant (truncating, splicing, or other) and the severity of the disorder in either the NEB TRI CNV families (p = 1) or NEB SV families (p > 0.05) separately, nor together (p > 0.05). No statistically significant correlation was found between the severity of the disorder and the copy number of the NEB TRI in families with NEB TRI CNVs (p > 0.05).
In contrast, a statistical significance was found between the size of the deletions segregating in a recessive versus a dominant fashion. The inheritance also correlated directly with the phenotype, where all dominant deletions were associated with a predominantly distal phenotype. Statistical significance was reached both in terms of the number of exons deleted (p = 0.0014) and the approximated size of the deletion (p = 0.0003), when grouped by phenotype or inheritance mode.
A correlation analysis between the length and number of exons affected in the groups of recessive SVs and dominant SVs suggests that dominant deletions are significantly larger than recessive deletions both in terms of the number of exons deleted and in terms of the length in base pairs (p < 0.0001 and p < 0.0001, Table 4.
Discussion
In this study, we describe 35 families presenting with either NM, NM-related disorders, or distal myopathies caused by SVs in NEB (Fig. 2). These families constitute around 7% of the over 520 families included in our research database. The families included in this study can be divided into three groups: 12 families with recessive CNVs of the NEB TRI region, 11 families with recessive SVs (both duplications and deletions), and 12 families affected by large dominant deletions in heterozygous or mosaic form.
Of the 520 families in our research database, 150 have a conclusive diagnosis of recessive NEB myopathy, and 12 are affected by dominant NEB variants. In 72 families, a single pathogenic recessive NEB variant has been identified, while 148 families remain with no causative variants found. The remaining families carry pathogenic variants in other known myopathy genes.
CNVs of the NEB TRI region constitute the most common recurrent form of benign SV in NEB. Benign or recessive CNVs of the NEB TRI region are present in all populations represented in gnomAD SVs v4.1.0, indicating that gains and losses of the NEB TRI show an independent recurrence. To date, the lowest NEB TRI copy number identified is 5 (3 + 2 per allele), and the highest 14 (in combinations of 11 + 3 and 7 + 7 per allele). The largest number of repeats on one allele recorded in our cohort is 11 (F3, copy number inferred by segregation). Benign losses of the NEB TRI region are marginally rarer than gains [18].
We have previously hypothesized that the pathogenetic mechanism behind gains of the NEB TRI region is based on the destabilization of mRNA or its secondary structure, thus affecting the translation process. [6] The alternative hypothesis has been that each gained block would add 486 amino acids and two super repeats to the protein, affecting the protein’s function as a stabilizer of the thin filament. In a recent study, Karimi & colleagues [51] used RNA sequencing, agarose gel electrophoresis, and thin filament length measurements to show that only two gained blocks were expressed at the mRNA level in a patient with a four-copy gain of the NEB TRI region. Both hypotheses may thus hold; not all gained blocks seem to be transcribed, but a longer protein is expressed in addition to the wild-type ones [51]. Additional studies on RNA and protein level of different NEB TRI gains would be of interest, but are limited by the availability of muscle biopsies.
Recessive SVs in NEB, both those previously published and those presented in this article, are either null alleles, truncating variants, or in-frame deletions of 1–24 exons [19, 23]. We hypothesize that all SVs encompassing the first three exons of the gene are recessive null variants, as the NEB start codon lies in exon 3; this applies to the largest recessive deletion in our cohort, a deletion of the 24 first exons of NEB (F15) and the large duplications of exons 1–89 (F13) and exons 1–51 (F14). No statistically significant genotype-phenotype correlations can be made between the severity of the disorder and type of small variant, NEB TRI copy number, or the size of recessive SVs.
Previously, all NEB variants, including SVs, were believed to be recessive. The first large, dominant deletions were described in 2019 and 2021. One of them segregated in a dominant fashion, and the other one was a de novo mosaic variant [21, 22]. In this update, we present nine novel families with large heterozygous deletions and one (F33) with a large deletion in mosaic form. Both patients with mosaic deletions presented with distal asymmetric muscle weakness.
Large deletions seem to be consistently associated with predominantly distal phenotypes, clearly distinct from the NEM2 clinical presentation. Additionally, the patients with these large deletions are more likely to be mildly affected compared with the two other groups presented. Expression analyses of these large in-frame deletions show expression of a shorter nebulin product and have previously been published for F24 and F25 [21, 22], and was performed for F35 (Supplementary Fig. 1). Histological findings in families with large dominant deletions are milder than in families with recessive NM and related disorders.
Currently known large recessive pathogenic deletions range from 1 to 24 exons, and duplications from 18 up to 89 exons in NEB [19, 21, 22]. The dominant deletions in our cohort vary in size between 51 and 97 exons, and all include the NEB exons 55–77. The upper limit of recessive deletion lengths is not currently known, but can possibly be deduced from the largest recessive and smallest dominant deletions in our cohort, and by the largest deletion recorded in gnomAD SVs 4.1.0, which spans ten exons (ex 159–168). We hypothesize that the threshold between a recessive and a dominant deletion may be anywhere between 24 and 51 exons.
Nebulin acts as a molecular ruler and stabilizer of the thin filament and contributes to physiological force generation [10, 11]. As all large, disease-causing heterozygous deletions are in-frame, the most likely pathogenetic mechanism is that sufficiently large deletions disrupt sarcomere assembly and function through a dominant-negative effect due to the expression of a shorter protein product.
The N-terminal part of the protein constitutes the thin filament cap. The C-terminus differs from the other parts of the gene in coding for the Z-disc anchor. Additionally, more alternative splicing in this region has been observed in comparison with other parts of the gene. It has been hypothesized that the C-terminal part may be vital for the function of the protein and/or sarcomere structure. In our cohort, none of the SVs affect NEB exons 134–187, and all the deletions identified affect the super repeat-rich regions, including the NEB TRI region (in green and yellow in Fig. 2). However, although our cohort lacks SVs located in the last third of the gene including the C-terminus, their presence in databases such as gnomAD SVs 4.1.0. indicates they are putative recessive pathogenic alleles. Whether a deletion is dominant or recessive may also depend on whether deleted exons are alternatively spliced, how many super repeats are deleted, or the involvement of a certain exon or range thereof.
The NEB TRI region is included in six of the eight unique large dominant deletions as well, and it is believed that the NEB TRI region, as other segmental duplications and repetitive regions, may mediate the occurrence of these SVs [6, 52]. The breakpoints of the large deletions coincide mostly with long interspersed nuclear elements (LINE) and Alu elements, but also simple repeats, retrotransposon-originating DNA repeats, and long terminal repeats (LTRs) (Supplementary Tables 5, 6). Despite the repetitive nature of NEB, our analysis points in the direction that SVs in NEB are more common compared with other NM causing genes primarily due to its size.
Targeted CGH-arrays [16, 17] have been the gold standard methodology for SV detection in NEB. To date, it is one of the most robust methods by which the level of mosaicism of large deletions can be determined. Densely targeted custom CGH-arrays allow accurate copy number analysis of the entire gene, including CNVs of the NEB TRI. However, accurate copy number estimation of the NEB TRI is lost at higher copy numbers due to the method’s binary logarithmic approach [17, 18]. SVs in NEB have been detected by MLPA, panel and/or exome sequencing, and genome short-read sequencing as well [21, 22].
A targeted ddPCR-based method for NEB TRI CNV screening has previously been published [18], allowing for screening in cases where a NEB TRI CNV is suspected as a second pathogenic variant, or for segregation analysis in families in which affected individuals have already been shown to be heterozygous for pathogenic CNVs of the NEB TRI using other methods (performed for F7).
The downsides of both the published custom CGH-arrays and the ddPCR assays developed for the NEB TRI region are that the methods are unable to distinguish between alleles and are limited to analyzing the genomic copy number, i.e. analyzing the expression of gained blocks from cDNA or RNA is not possible using these methods. Secondly, the methods are based on the similarity of the repeated sequences, and they can therefore not distinguish which 8-exon-block is gained or lost, in which orientation gained blocks reside in relation to the gene, or whether duplicated sequences are located within the gene or elsewhere in the genome.
State-of-the-art genomic technologies, such as long-read sequencing (LRS) and optical genome mapping (OGM), show great promise in the detection of SVs in cases where standard-of-care approaches have failed to identify causative variants [53]. Paired with bioinformatic tools especially developed for this purpose, such as Paraphase, LRS may soon also be able to identify NEB TRI copy numbers at equal sensitivity [54], with the added advantage of allele phasing.
To date, no inversions, translocations, or larger complex rearrangements have been described in NEB. As OGM and LRS become more readily available, these types of SVs may well be identified in previously undiagnosed families.
In summary, we describe an international cohort of 12 families with recessive NEB TRI CNVs, 11 families with recessive SVs, and 12 families with dominant SVs in NEB. This study presents the largest cohort of families (n = 35) to date with pathogenic NEB SVs, both recessive and dominant. We establish a clear phenotype-genotype correlation between large dominant deletions of more than 51 exons and distal myopathy.
Data availability
All data relevant to this study can be found within the manuscript. Additional data are available from the corresponding author on reasonable request.
References
Donner K, Sandbacka M, Lehtokari VL, Wallgren-Pettersson C, Pelin K. Complete genomic structure of the human nebulin gene and identification of alternatively spliced transcripts. Eur J Hum Genet. 2004;12:744–51.
Laitila J, Hanif M, Paetau A, Hujanen S, Keto J, Somervuo P, et al. Expression of multiple nebulin isoforms in human skeletal muscle and brain. Muscle Nerve. 2012;46:730–7.
Labeit S, Kolmerer B. The complete primary structure of human nebulin and its correlation to muscle structure. J Mol Biol. 1995;248:308–15.
Wright J, Huang QQ, Wang K. Nebulin is a full-length template of actin filaments in the skeletal muscle sarcomere: an immunoelectron microscopic study of its orientation and span with site-specific monoclonal antibodies. J muscle Res Cell Motil. 1993;14:476–83.
Laitila J, Lehtonen J, Lehtokari VL, Sagath L, Wallgren-Pettersson C, Grönholm M, et al. A nebulin super-repeat panel reveals stronger actin binding toward the ends of the super-repeat region. Muscle Nerve. 2019;59:116–21.
Kiiski K, Lehtokari VL, Löytynoja A, Ahlstén L, Laitila J, Wallgren-Pettersson C, et al. A recurrent copy number variation of the NEB triplicate region: only revealed by the targeted nemaline myopathy CGH array. Eur J Hum Genet. 2016;24:574–80.
Wang Z, Grange M, Pospich S, Wagner T, Kho AL, Gautel M, et al. Structures from intact myofibrils reveal mechanism of thin filament regulation through nebulin. Science. 2022;375:eabn1934.
Pelin K, Hilpelä P, Donner K, Sewry C, Akkari PA, Wilton SD, et al. Mutations in the nebulin gene associated with autosomal recessive nemaline myopathy. Proc Natl Acad Sci USA. 1999;96:2305–10.
Millevoi S, Trombitas K, Kolmerer B, Kostin S, Schaper J, Pelin K, et al. Characterization of nebulette and nebulin and emerging concepts of their roles for vertebrate Z-discs. J Mol Biol. 1998;282:111–23.
Kiss B, Gohlke J, Tonino P, Hourani Z, Kolb J, Strom J, et al. Nebulin and Lmod2 are critical for specifying thin-filament length in skeletal muscle. Sci Adv. 2020;6:eabc1992.
Kiss B, Lee EJ, Ma W, Li FW, Tonino P, Mijailovich SM, et al. Nebulin stiffens the thin filament and augments cross-bridge interaction in skeletal muscle. Proc Natl Acad Sci USA. 2018;115:10369–74.
Bang ML, Li X, Littlefield R, Bremner S, Thor A, Knowlton KU, et al. Nebulin-deficient mice exhibit shorter thin filament lengths and reduced contractile function in skeletal muscle. J Cell Biol. 2006;173:905–16.
Witt CC, Burkart C, Labeit D, McNabb M, Wu Y, Granzier H, et al. Nebulin regulates thin filament length, contractility, and Z-disk structure in vivo. EMBO J. 2006;25:3843–55.
Ottenheijm CA, Hooijman P, DeChene ET, Stienen GJ, Beggs AH, Granzier H. Altered myofilament function depresses force generation in patients with nebulin-based nemaline myopathy (NEM2). J Struct Biol. 2010;170:334–43.
Fokkema IF, Taschner PE, Schaafsma GC, Celli J, Laros JF, den Dunnen JT. LOVD v.2.0: the next generation in gene variant databases. Hum Mutat. 2011;32:557–63.
Kiiski K, Laari L, Lehtokari VL, Lunkka-Hytönen M, Angelini C, Petty R, et al. Targeted array comparative genomic hybridization-a new diagnostic tool for the detection of large copy number variations in nemaline myopathy-causing genes. Neuromuscul Disord. 2013;23:56–65.
Sagath L, Lehtokari VL, Välipakka S, Udd B, Wallgren-Pettersson C, Pelin K, et al. An extended targeted copy number variation detection array including 187 genes for the diagnostics of neuromuscular disorders. J Neuromuscul Dis. 2018;5:307–14.
Sagath L, Lehtokari VL, Wallgren-Pettersson C, Pelin K, Kiiski K. A custom ddPCR method for the detection of copy number variations in the nebulin triplicate region. PLoS One. 2022;17:e0267793.
Lehtokari VL, Kiiski K, Sandaradura SA, Laporte J, Repo P, Frey JA, et al. Mutation update: the spectra of nebulin variants and associated myopathies. Hum Mutat. 2014;35:1418–26.
Wallgren-Pettersson C, Lehtokari VL, Kalimo H, Paetau A, Nuutinen E, Hackman P, et al. Distal myopathy caused by homozygous missense mutations in the nebulin gene. Brain J Neurol. 2007;130:1465–76.
Kiiski K, Lehtokari VL, Vihola AK, Laitila JM, Huovinen S, Sagath LJ, et al. Dominantly inherited distal nemaline/cap myopathy caused by a large deletion in the nebulin gene. Neuromuscul Disord. 2019;29:97–107.
Sagath L, Lehtokari VL, Välipakka S, Vihola A, Gardberg M, Hackman P, et al. Congenital asymmetric distal myopathy with hemifacial weakness caused by a heterozygous large de novo mosaic deletion in nebulin. Neuromuscul Disord. 2021;31:539–45.
Anderson SL, Ekstein J, Donnelly MC, Keefe EM, Toto NR, LeVoci LA, et al. Nemaline myopathy in the Ashkenazi Jewish population is caused by a deletion in the nebulin gene. Hum Genet. 2004;115:185–90.
Pelin K, Donner K, Holmberg M, Jungbluth H, Muntoni F, Wallgren-Pettersson C. Nebulin mutations in autosomal recessive nemaline myopathy: an update. Neuromuscul Disord. 2002;12:680–6.
Lehtokari VL, Pelin K, Sandbacka M, Ranta S, Donner K, Muntoni F, et al. Identification of 45 novel mutations in the nebulin gene associated with autosomal recessive nemaline myopathy. Hum Mutat. 2006;27:946–56.
Lawlor MW, Ottenheijm CA, Lehtokari VL, Cho K, Pelin K, Wallgren-Pettersson C, et al. Novel mutations in NEB cause abnormal nebulin expression and markedly impaired muscle force generation in severe nemaline myopathy. Skelet Muscle. 2011;1:23.
Ochala J, Lehtokari VL, Iwamoto H, Li M, Feng HZ, Jin JP, et al. Disrupted myosin cross-bridge cycling kinetics triggers muscle weakness in nebulin-related myopathy. FASEB J. 2011;25:1903–13.
Kapoor S, Singh A, Lehtokari VL, Wallgren-Pettersson C, Batra VV. Mutations in the nebulin gene in a child with nemaline (rod) myopathy. Indian J Pediatr. 2013;80:691–3.
Malfatti E, Lehtokari VL, Böhm J, De Winter JM, Schäffer U, Estournet B, et al. Muscle histopathology in nebulin-related nemaline myopathy: ultrastrastructural findings correlated to disease severity and genotype. Acta Neuropathol Commun. 2014;2:44.
Christophers B, Lopez MA, Gupta VA, Vogel H, Baylies M. Pediatric nemaline myopathy: a systematic review using individual patient data. J Child Neurol. 2022;37:652–63.
Wallgren-Pettersson C. Congenital nemaline myopathy: a longitudinal study. Finnish Society of Sciences and Letters. 1990.
Maggi L, Scoto M, Cirak S, Robb SA, Klein A, Lillis S, et al. Congenital myopathies-clinical features and frequency of individual subtypes diagnosed over a 5-year period in the United Kingdom. Neuromuscul Disord. 2013;23:195–205.
Shy GM, Engel WK, Somers JE, Wanko T. Nemaline myopathy. A new congenital myopathy. Brain J Neurol. 1963;86:793–810.
Piteau SJ, Rossiter JP, Smith RG, MacKenzie JJ. Congenital myopathy with cap-like structures and nemaline rods: case report and literature review. Pediatr Neurol. 2014;51:192–7.
Romero NB, Lehtokari VL, Quijano-Roy S, Monnier N, Claeys KG, Carlier RY, et al. Core-rod myopathy caused by mutations in the nebulin gene. Neurology. 2009;73:1159–61.
Feingold-Zadok M, Chitayat D, Chong K, Injeyan M, Shannon P, Chapmann D, et al. Mutations in the NEB gene cause fetal akinesia/arthrogryposis multiplex congenita. Prenat Diagn. 2017;37:144–50.
Lehtokari VL, Pelin K, Herczegfalvi A, Karcagi V, Pouget J, Franques J, et al. Nemaline myopathy caused by mutations in the nebulin gene may present as a distal myopathy. Neuromuscul Disord. 2011;21:556–62.
Scoto M, Cullup T, Cirak S, Yau S, Manzur AY, Feng L, et al. Nebulin (NEB) mutations in a childhood onset distal myopathy with rods and cores uncovered by next generation sequencing. Eur J Hum Genet. 2013;21:1249–52.
Park YE, Shin JH, Kang B, Lee CH, Kim DS. NEB-related core-rod myopathy with distinct clinical and pathological features. Muscle Nerve. 2016;53:479–84.
Mizuno Y, Mori-Yoshimura M, Oya Y, Nishikawa A, Nishino I, Takahashi Y. Two cases of nemaline myopathy presenting with hypertrophy of distal limbs with prominent asymmetry. Clin Neurol. 2017;57:691–7.
Wilson LA, Macken WL, Perry LD, Record CJ, Schon KR, Frezatti RSS, et al. Neuromuscular disease genetics in under-represented populations: increasing data diversity. Brain J Neurol. 2023;146:5098–109.
Klambauer G, Schwarzbauer K, Mayr A, Clevert DA, Mitterecker A, Bodenhofer U, et al. cn.MOPS: mixture of Poissons for discovering copy number variations in next-generation sequencing data with a low false discovery rate. Nucleic Acids Res. 2012;40:e69.
Demidov G, Ossowski S. ClinCNV: novel method for allele-specific somatic copy-number alterations detection. bioRxiv. 2019. https://www.biorxiv.org/content/10.1101/837971v1.
Kadalayil L, Rafiq S, Rose-Zerilli MJ, Pengelly RJ, Parker H, Oscier D, et al. Exome sequence read depth methods for identifying copy number changes. Brief Bioinform. 2015;16:380–92.
McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, Thormann A, et al. The ensembl variant effect predictor. Genome Biol. 2016;17:122.
Patel, K. Statistical analysis of regions with CNVs. Bioconductor. 2024. https://doi.org/10.18129/B9.bioc.SARC.
Backenroth D, Homsy J, Murillo LR, Glessner J, Lin E, Brueckner M, et al. CANOES: detecting rare copy number variants from whole exome sequencing data. Nucleic Acids Res. 2014;42:e97.
Warren CM, Krzesinski PR, Greaser ML. Vertical agarose gel electrophoresis and electroblotting of high-molecular-weight proteins. Electrophoresis. 2003;24:1695–702.
Wallgren-Pettersson C, Laing NG. Report of the 70th ENMC International Workshop: nemaline myopathy, 11-13 June 1999, Naarden, The Netherlands. Neuromuscul Disord: Nmd. 2000;10:299–306.
Dubowitz V. Nemaline myopathy: a tale of two cultures. Neuromuscul Disord. 2009;19:177–8.
Karimi E, van der Borgh M, Lindqvist J, Gohlke J, Hourani Z, Kolb J, et al. Characterization of NEB mutations in patients reveals novel nemaline myopathy disease mechanisms and omecamtiv mecarbil force effects. bioRxiv. 2023. https://www.biorxiv.org/content/10.1101/2023.12.20.572678v1.full.
Sharp AJ, Locke DP, McGrath SD, Cheng Z, Bailey JA, Vallente RU, et al. Segmental duplications and copy-number variation in the human genome. Am J Hum Genet. 2005;77:78–88.
Steyaert W, Sagath L, Demidov G, Yépez VA, Esteve-Codina A, Gagneur J, et al. Unravelling undiagnosed rare disease cases by HiFi long-read genome sequencing. Genome Res. 2025;35:1–14.
Chen X, Harting J, Farrow E, Thiffault I, Kasperaviciute D, Hoischen A, et al. Comprehensive SMN1 and SMN2 profiling for spinal muscular atrophy analysis using long-read PacBio HiFi sequencing. Am J Hum Genet. 2023;110:240–50.
Acknowledgements
We thank Marilotta Turunen and Nicolas Dondaine for excellent technical assistance, and MSc Nick Zomer for valuable comments on the manuscript.
Funding
This study was supported by the Folkhälsan Research Foundation, the Sigrid Jusélius Foundation, the Medicinska understödsföreningen Liv och Hälsa r.f., Finska Läkaresällskapet, Stiftelsen Perkléns Minne, the Jane and Aatos Erkko Foundation, Muscular Dystrophy UK, and the Waldemar von Frenckells stiftelse. LS was supported by a Sigrid Jusélius fellowship (220540). FH and KN were supported by an MRC strategic award to establish an International Centre for Genomic Medicine in Neuromuscular Diseases (ICGNMD) MR/S005021/1. KN received additional Fellowship support from the Guarantors of Brain (UK Charity 1197319). MS was supported by the Academy of Finland. The work in C.G.B.’s laboratory is supported by intramural funds from the NIH National Institute of Neurological Disorders and Stroke. Analysis of families F22, F23 and F33 was supported in part by A Foundation Building Strength for Nemaline Myopathy, Boston Children’s Hospital IDDRC Molecular Genetics Core Facility funded by P50HD105351 from the National Institutes of Health of USA, and the Boston Children’s Hospital CRDC Initiative. Open Access funding provided by University of Helsinki (including Helsinki University Central Hospital).
Author information
Authors and Affiliations
Contributions
Conceptualization: LS, V-LL; Data Curation: LS, KK, V-LL; Formal analysis: LS, KK, KP, V-LL; Funding acquisition: LS, FH, MS, CGB, CW-P, KP; Investigation: LS, KK, KN, PHJ, KP, ML, DD, GY, AC, CR, MKG, KS, EKu, EKo, DH, MD, PJ, AZ, RO, SD, CHB, MS, AE-L, VB, CAG, AHB, FH, V-LL; Methodology: LS, KK, KP, V-LL; Resources: KN, DD, GY, AC, CR, MKG, KS, EKu, EKo, DH, MD, PJ, AZ, SD, CHB, AE-L, VB, CAG, AHB, CW-P, FH, KP; Supervision: FH, V-LL; Validation: LS, KK, PHJ, V-LL; Visualization: LS; Writing – original draft: LS, V-LL; Writing – Review & Editing: LS, KK, KN, PHJ, KP, ML, DD, GY, AC, CR, MKG, KS, EKu, EKo, DH, MD, PJ, AZ, RO, SD, CHB, MS, AE-L, VB, CAG, AHB, CW-P, FH, KP, V-LL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
All subjects or legal guardians provided written informed consent for publication of this manuscript. The study was conducted in accordance with the 1984 Declaration of Helsinki and its subsequent revisions.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sagath, L., Kiiski, K., Naidu, K. et al. Structural variation in nebulin and its impact on phenotype and inheritance: establishing a dominant distal phenotype caused by large deletions. Eur J Hum Genet 33, 1153–1162 (2025). https://doi.org/10.1038/s41431-025-01891-0
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41431-025-01891-0
This article is cited by
-
The utility of next generation sequencing targeted multigene panels in the Adult Neurogenetic Clinic at Tygerberg Hospital, South Africa
European Journal of Human Genetics (2025)
-
What’s new in EJHG this autumn
European Journal of Human Genetics (2025)