Abstract
Background
Oral diseases are a major public health concern in Low and Middle Income Countries (LMICs), where effective treatment requires multiple appointments. Despite its importance, limited research has explored appointment adherence among adults in these settings. This scoping review identifies the barriers and facilitators to attending dental care appointments in LMICs.
Methods
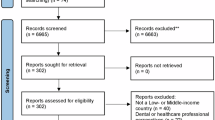
The current review followed JBI Scoping Review Methodology. The Databases of Dentistry, Oral Sciences Source (EBSCO), MEDLINE (Ovid), Embase (Ovid), Cochrane CENTRAL, Scopus and grey literature sources were searched systematically from inception till November 2024. Two independent reviewers performed data extraction using a customized JBI data extraction form. The Theoretical Domains Framework categorized barriers and facilitators of dental appointment keeping. Findings were tabulated and synthesized narratively with recommendations to improve dental attendance.
Results
Ten articles met the inclusion criteria after being screened through 5571 titles, abstracts, and 210 full texts. Knowledge, social and professional roles and identity, beliefs about capabilities, consequences, memory, attention, decision-making processes, environmental context and resources, social influence, and emotion are the main domains under which barriers and facilitators were identified. Environmental context and resource constraints were the most common barriers, while social influence was the main facilitator. The dental appointment adherence issues were determined to be comparable in public practice and university settings.
Conclusion
It is necessary to acknowledge the barriers and facilitators to dental appointment keeping to improve the effectiveness of the dental health system, ensure continuity of care, and encourage better patient-doctor relationships. Tailored interventions are required in the dental setting to effectively manage and reduce disparities in patient care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data used in this systematic review were obtained from publicly available sources, including published research articles and reports. All data sources are appropriately cited in the reference section of this review. No additional datasets or proprietary information were used in this study. Researchers interested in accessing the primary data used in the included studies should refer to the original publications and contact the respective authors or institutions for any specific data requests or inquiries.
References
Peres MA, Macpherson LMD, WeyantRJ, Venturelli R, Mathur MR, Listl S, et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249–60.
Oral health [Internet]. Who.int. 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/oral-health
Tandon S, Duhan R, Sharma M, Vasudeva S. Between the Cup and the Lip: Missed Dental Appointments. J Clin Diagn Res. 2016;10:ZC122–ZC124.
Onyejaka NK, Emele IE, Eboh OF. Appointment Failure among Dental Patients Attending a Government Dental Centre in Enugu, Nigeria. PesquisaBrasileiraemOdontopediatria e ClínicaIntegrada. 2018;18:1–7.
Petersen PE, Baez RJ, Ogawa H. Global application of oral disease prevention and health promotion as measured 10 years after the 2007 World Health Assembly statement on oral health. Community Dent Oral Epidemiol. 2020;48:338–48.
Ismail AI, Saeed MH, Al-Silwadi FM. Missed dental appointments in the United Arab Emirates. J Int Dent Med Res. 2011;4:132–8.
Anagha KA, Megha M, Karuveettil V, Vijay Kumar S. Perceptions of barriers towards dental appointment keeping among patients of a tertiary care setting: A mixed method exploration. J Oral Biol Craniofac Res. 2024;14:185–91. https://doi.org/10.1016/j.jobcr.2024.02.00247.
Khairuddeen NFI, Ahmad Nazari NHN, Ali Al-Kadhim AH, Samsudin AD, Amran N, Abdul Hamid NF, et al. Prevalence and reasons for missed dental appointments among patients treated by undergraduate dental students of Universiti Sains Islam Malaysia. IIUM J Orofacial Health Sci. 2022;3:95–101.
Listl S, Moeller J, Manski R. A multi-country comparison of reasons for dental non-attendance. Eur J Oral Sci. 2014;122:62–9.
Shabbir A, Alzahrani M, Abu Khalid A. Why Do Patients Miss Dental Appointments in Eastern Province Military Hospitals, Kingdom of Saudi Arabia?. Cureus. 2018;10:e2355.
Baskaradoss JK. The association between oral health literacy and missed dental appointments. J Am Dent Assoc. 2016;147:867–74.
AlSadhan SA. Frequency of missed and cancelled appointments in King Saud University orthodontic clinic. King Saud Univ J Dent Sci. 2013;4:77–80.
Pohjola V, Lahti S, Vehkalahti MM, Tolvanen M, Hausen H. Association between dental fear and dental attendance among adults in Finland. Acta Odontol Scand. 2007;65:224–30.
Lapidos A, Shaefer HL, Gwozdek A. Toward a better understanding of dental appointment-keeping behavior. Community Dent Oral Epidemiol. 2016;44:85–91.
Syed ST, Gerber BS, Sharp LK. Traveling towards disease: Transportation barriers to health care access. J Community Health. 2013;38:976–93.
AlBarakati SF. Appointments Failure Among Female Patients at a Dental School Clinic in Saudi Arabia. J Dent Educ. 2009;73:1118–24.
Panda A, Bhatia R, Vora EC. Pediatric Dental Appointments No-show: Rates and Reasons. Int J Clin Pediatr Dent. 2018;11:171–6.
Åstrøm AN, Lie SA, Mastrovito B, Sannevik J. Avoidance of dental appointment due to cost and consequences for oral health-related quality of life: 25-yr follow-up of Swedish adults. Eur J Oral Sci. 2021;129:e12778.
Lalloo R, McDonald JM. Appointment attendance at a remote rural dental training facility in Australia. BMC Oral Health. 2013;13:36.
Åstrøm AN, Lie SA, Gülcan F. Applying the theory of planned behavior to self-report dental attendance in Norwegian adults through structural equation modelling approach. BMC Oral Health. 2018;18:95.
Gollwitzer PM. Implementation intentions: Strong effects of simple plans. Am Psychologist. 1999;54:493–503.
Kwasnicka D, Presseau J, White M, Sniehotta FF. Does planning how to cope with anticipated barriers facilitate health-related behaviour change? A systematic review. Health Psychol Rev. 2013;7:129–45.
Badri P, Saltaji H, Flores-Mir C, Amin M. Factors affecting children’s adherence to regular dental attendance: A systematic review. J Am Dent Assoc. 2014;145:817–28.
Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions. 1st ed. Great Britain: Silverback Publishing. 2014, pp. 1003–10.
Michie S, Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12:77.
Weatherson KA, Gainforth HL, Jung ME. A theoretical analysis of the barriers and facilitators to the implementation of school-based physical activity policies in Canada: a mixed methods scoping review. Implementation Sci. 2017;12:41.
Lau S, Lun P, Ang W, Tan KT, Ding YY. Barriers to effective prescribing in older adults: applying the theoretical domains framework in the ambulatory setting – a scoping review. BMC Geriatr. 2020;20:459.
Riley IL, Jackson B, Crabtree D, Riebl S, Que LG, Pleasants R, et al. A Scoping Review of International Barriers to Asthma Medication Adherence Mapped to the Theoretical Domains Framework. J Allergy Clin Immunol Pr. 2021;9:410–418.e4.
Moncion K, Biasin L, Jagroop D, Bayley M, Danells C, Mansfield A, et al. Barriers and Facilitators to Aerobic Exercise Implementation in Stroke Rehabilitation: A Scoping Review. J Neurol Phys Ther. 2020;44:179–87.
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: Scoping reviews. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. Adelaide: JBI, 2020. Available from: https://synthesismanual.jbi.global
Chang S. Scoping reviews and systematic reviews: is it an either/or question?. Ann Intern Med. 2018;169:502–3.
Karuveettil V, Sapna S, Jain P, Samad F. Barriers and facilitators to attending dental care appointments among adults in low- and middle-income countries: a scoping review protocol. JBI Evid Synth. 2022;20:2536–42.
Tricco, Lillie AC, Zarin E, O’Brien W, Colquhoun KK, LevacD H, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
World Bank Country and Lending Groups – World Bank Data Help Desk. 2025. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, et al. The development of software to support multiple systematic review types: the Joanna Briggs institute system for the unified management, assessment and review of information (JBISUMARI). Int J Evid Based Health. 2019;17:36–43.
George AC, Hoshing A, Joshi NV. A study of the reasons for irregular dental attendance in a private dental college in a rural setup. Indian J Dent Res. 2007;18:78–81.
Gokulanathan S, Balan N, Aravind RJ, Thangavelu K. Patient compliance and supportive periodontal therapy: Study among young adults of Namakkal district. J Pharm Bioallied Sci. 2014;6:S171–3.
Jaju K, Nasim I, Mahalakshmi J. Patients Reporting on Appointment Date After Access Opening For Further Treatment to Dental Hospital - A Cross Sectional Study. Indian J Forensic Med Toxicol. 2020;14:5871–8.
Fenol A, Mathew S. Compliance to recall visits by patients with periodontitis - Is the practitioner responsible?. J Indian Soc Periodontol. 2010;14:106.
Appukuttan DP, Tadepalli A, Cholan PK, Subramanian S, Vinayagavel M. Prevalence of dental anxiety among patients attending a dental educational institution in Chennai, India-a questionnaire based study. Oral Health Dent Manag. 2013;12:289–94.
Pakpour AH, Gellert P, Asefzadeh S, Sniehotta FF. Planning predicts dental service attendance and the effect is moderated by dental anxiety and educational status: Findings from a one-year prospective study. ApplPsychol Health Well Being. 2014;6:214–29.
Goh EZ, Beech N, Johnson NR. Dental anxiety in adult patients treated by dental students: A systematic review. J Dent Educ. 2020;84:805–11.
Matsuoka Y, Fukai K. What is keeping appointments? Health Sci Health Care. 2010;10:28–32.
Langlois MA, Hallam JS. Integrating multiple health behavior theories into program planning: The per worksheet. Health Promotion Pract. 2008;11:282–8.
Kapoor D, Kapoor P, Kaur I, Singh A, Gill S. Oral hygiene awareness and practice amongst patients visiting the Department of Periodontology at a Dental College and Hospital in North India. Indian J Dent. 2014;5:64.
DDS RW. Patient Centricity in dentistry for better treatment outcomes [Internet]. #ColgateTalks. 2019 [cited 30 Novembermber 2022]. Available from: https://www.colgatetalks.com/patient-centricity-in-dentistry/
McQueenie R, Ellis DA, Fleming M, Wilson P, Williamson AE. Educational associations with missed GP appointments for patients under 35 years old: administrative data linkage study. BMC Med. 2021;19.
Heaton LJ, Smith TA, Raybould TP. Factors Influencing Use of Dental Services in Rural and Urban Communities: Considerations for Practitioners in Underserved Areas. J Dent Educ. 2004;68:1081–9.
Can S, Macfarlane T, O’Brien KD. The use of postal reminders to reduce non-attendance at an orthodontic clinic: A randomised controlled trial. Br Dent J. 2003;195:199–201.
Mohammed H, RizkMZ, Wafaie K, Ulhaq A, Almuzian M. Reminders improve oral hygiene and adherence to appointments in orthodontic patients: a systematic review and meta-analysis. Eur J Orthod. 2019;41:204–13.
Perry JG. A preliminary investigation into the effect of the use of the Short Message Service (SMS) on patient attendance at an NHS Dental Access Centre in Scotland. Prim Dent Care. 2011;18:145–9.
McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, et al. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016;10:479–99.
Shah SJ, Cronin P, Hong CS, Hwang AS, Ashburner JM, Bearnot BI, et al. Targeted Reminder Phone Calls to Patients at High Risk of No-Show for Primary Care Appointment: A Randomized Trial. J Gen Intern Med. 2016;31:1460–6.
Levine RS. Caries experience and bedtime consumption of sugar-sweetened food and drinks-a survey of 600 children. Community Dent Health. 2001;18:228–31.
Hardy KJ, O’Brien SV, Furlong NJ. Information given to patients before appointments and its effect on non-attendance rate. BMJ. 2001;323:1298–300.
Bhagat D, Khan MHA, Uddin MA. Barriers for Parental Failure in Bringing their Children to the Dental Clinic—A Questionnaire-based Study in Indian Population. Indian J Mednodent Allied Sci. 2014;2:17.
Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc. 1984;109:247–51.
Lindsay SJ, Humphris G, Barnby GJ. Expectations and preferences for routine dentistry in anxious adult patients. Br Dent J. 1987;163:120–4.
Skaret E, Raadal M, Kvale G, Berg E. Factors related to missed and cancelled dental appointments among adolescents in Norway. Eur J Oral Sci. 2000;108:175–83.
Bos A, Hoogstraten J, Prahl-Andersen B. Failed appointments in an orthodontic clinic. Am J Orthod Dentofac Orthopedics. 2005;127:355–7.
Almog DM, Devries JA, Borrelli JA, Kopycka-Kedzierawski DT. The Reduction of Broken Appointment Rates Through an Automated Appointment Confirmation System. J Dent Educ. 2003;67:1016–22.
Wegrzyniak LM, Hedderly D, Chaudry K, Bollu P. Measuring the effectiveness of patient-chosen reminder methods in a private orthodontic practice. Angle Orthod. 2018;88:314–8.
Reekie D, Devlin H. Preventing failed appointments in general dental practice: a comparison of reminder methods. Br Dent J. 1998;185:472–4.
Demetriou N, Tsami-Pandi A, Parashis A. Compliance with supportive periodontal treatment in private periodontal practice. A 14-year retrospective study. J Periodontol. 1995;66:145–9.
Liddell A, May B. Some characteristics of regular and irregular attenders for dental check-ups. Br J Clin Psychol. 1984;23:19–26.
Søgaard AJ, Aarø LE, Heløe LA. Irregular users of dental services among Norwegian adults. Acta Odontol Scand. 1987;45:371–81.
Rosing K, Leggett H, Csikar J, Vinall-Collier K, Christensen LB, Whelton H, et al. Barriers and facilitators for prevention in Danish dental care. Acta Odontol Scand. 2019;77:439–51.
Alkomos MF, Mendez D, Mazzei-Pifano D, Shafeek F, Rodriguez C, Ali F, et al. Patients’ reasons for missing scheduled clinic appointments and their solutions at a major urban-based academic medical center. J Community Hosp Intern Med Perspect. 2020;10:426–30.
Kadanakuppe S. Effective Communication and Empathy Skills in Dentistry for Better Dentist-Patient Relationships. J Dental Problems Solutions. 2015;2:58–9.
Appukuttan DP. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin CosmetInvestig Dent. 2016;8:35–50.
Gillam DG, Yusuf H. Brief Motivational Interviewing in Dental Practice. Dent J. 2019;7:51.
Dubé-Baril. Debate Charging for Missed Appointments. Vol. 75. 2009. Available from: www.cda-adc.ca/jcda/vol-75/issue-1/33.html
Acknowledgements
LearnByResearch, Pune, supported the study.
Author information
Authors and Affiliations
Contributions
VK was responsible for conceptualization, search strategy, screening, data extraction, analysis, and manuscript preparation. SS contributed to screening, data extraction, and report writing. PJ participated in screening, data extraction, and report writing. GA was involved in search updates, screening, data extraction, analysis, and report writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karuveettil, V., Sapna, S., Jain, P. et al. Barriers to and facilitators for attending dental care appointments among adults in low- and middle-income countries: a scoping review. Evid Based Dent 26, 150–151 (2025). https://doi.org/10.1038/s41432-025-01148-1
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41432-025-01148-1