Abstract
Background
To study the role of selective laser trabeculoplasty (SLT) in intraocular pressure (IOP) reduction in post-laser iridotomy primary angle-closure disease patients with inadequately controlled IOP.
Methods
In this prospective cross-sectional study, 34 patients with primary angle-closure disease with post-laser iridotomy open angles up to at least 180° were recruited. Following SLT, patients were examined at 1 day, 1 week, 1 and 3 months, 6 months and 1 year post SLT.
Results
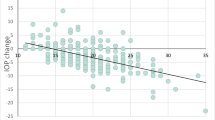
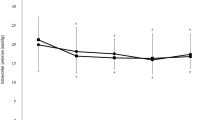
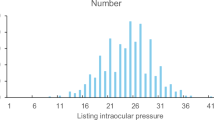
Data of 34 patients (34 eyes; 8 males and 26 females), with a mean age of 57.80 ± 6.44 years, were analysed. The reduction in IOP at each follow-up visit was significant (p < 0.001). The maximum reduction in IOP was noticed on post-laser day 1 and the least reduction was noticed 1 week post laser. Post-SLT range of IOP reduction varied from 9 to 46% at 1 year, which indicates the variability of a response to SLT. Mean IOP in both primary angle closure (PAC) and primary angle closure glaucoma (PACG) groups was comparable at all visits except at post-SLT week 1 when IOP in the PACG group was significantly higher than that in the PAC group (p = 0.035). None of the patients complained of pain and/or discomfort or had any clinically significant anterior segment inflammation on any of the follow-up visits. None of the patients underwent repeat SLT or surgery. The mean pre-SLT and post-SLT visual field index at 1-year follow-up was 95.47 ± 3.58 and 95.90 ± 4.13, respectively, which was not significant (p = 0.84).
Conclusions
High baseline IOP significantly correlated with reduction in IOP. Our results suggest that SLT is a safe, cost-effective modality for reducing IOP in primary angle-closure disease with patent laser iridotomy with a visible trabecular meshwork.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
10 July 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41433-020-1047-1
References
Quigley HA. Glaucoma. Lancet. 2011;377:1367–77.
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7.
Cheng J-W, Zong Y, Zeng Y-Y, Wei R-L. The prevalence of primary angle closure glaucoma in adult Asians: a systematic review and meta-analysis. Acott TS, ed. PLoS ONE. 2014;9:e103222.
Amoozgar B, Moghimi S, Han Y, Lin SC. An update on therapeutic modalities for the prevention of angle closure glaucoma. Curr Opin Ophthalmol. 2017 Mar;28(2):175–180.
Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, et al. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet. 2016;388:1389–97. https://doi.org/10.1016/S0140-6736(16)30956-4.
Peng PH, Nguyen H, Lin HS, Nguyen N, Lin S. Long-term outcomes of laser iridotomy in Vietnamese patients with primary angle closure. Br J Ophthalmol. 2011;95:1207–11.
Quek DT, Ong GT, Perera SA, Lamoureux EL, Aung T. Persistence of patients receiving topical glaucoma monotherapy in an Asian population. Arch Ophthalmol. 2011;129:643–8.
De Keyser M, De Belder M, De Belder S, De Groot V. Where does selective laser trabeculoplasty stand now? A review. Eye Vis (Lond). 2016;3:10.
Olthoff CM, Schouten JS, van de Borne BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112:953–61.
Ho CL, Lai JS, Aquino MV, Rojanapongpun P, Wong HT, Aquino MC, et al. Selective laser trabeculoplasty for primary angle closure with persistently elevated intraocular pressure after iridotomy. J Glaucoma. 2009;18:563–6.
Narayanaswamy A, Leung CK, Istiantoro DV, Perera SA, Ho CL, Nongpiur ME, et al. Efficacy of selective laser trabeculoplasty in primary angle-closure glaucoma: a randomized clinical trial. JAMA Ophthalmol. 2015;133:206–12.
Ali Aljasim L, Owaidhah O, Edward DP. Selective laser trabeculoplasty in primary angle-closure glaucoma after laser peripheral iridotomy: a case–control study. J Glaucoma. 2016;25:e253–8.
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–4.
Hodapp E, Parrish RK II, Anderson DR. Clinical decisions in glaucoma. St. Louis, MO: Mosby Year Book Inc; 1993. p. 52–9.
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
South East Asia Glaucoma Interest Group. Appendix 6A. Gonioscopy. Asia Pacific Glaucoma Guidelines. 2nd ed. South East Asia Glaucoma Interest Group; Kugler Publications, Amsterdam, The Netherlands 2008.
Matos AG, Asrani SG, Paula JS. Feasibility of laser trabeculoplasty in angle closure glaucoma: a review of favorable histopathological findings in narrow angles. Clin Exp Ophthalmol. 2017;45:632–9.
Johnson PB, Katz LJ, Rhee DJ. Selective laser trabeculoplasty: predictive value of early intraocular pressure measurements for success at 3 months. Br J Ophthalmol. 2006;90:741–3.
McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006;15:124–30.
Kagan DB, Gorfinkel NS, Hutnik CM, Mechanisms of selective laser trabeculoplasty: a review. Clin Exp Ophthalmol. 2014;42:675–81.
Nagar M, Ogunyomade A, O’Brart DP, Howes F, Marshall J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005;89:1413–7.
Stein JD, Challa P. Mechanisms of action and efficacy of argon laser trabeculoplasty and selective laser trabeculoplasty. Curr Opin Ophthalmol. 2007;18:140–5.
Alvarado JA, Yeh RF, Franse-Carman L, Marcellino G, Brownstein MJ. Interactions between endothelia of the trabecular meshwork and of Schlemm’s canal: a new insight into the regulation of aqueous outflow in the eye. Trans Am Ophthalmol Soc. 2005;103:148–62. discussion 62–3
Leahy KE, White AJ, Selective laser trabeculoplasty: current perspectives. Clin Ophthalmol. 2015;9:833–41.
Martinez-de-la-Casa JM, Garcia-Feijoo J, Castillo A, et al. Selective vs argon laser trabeculoplasty: hypotensive efficacy, anterior chamber inflammation, and postoperative pain. Eye (Lond). 2004;18:498–502.
Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G. Q-switched 532-nm Nd:YAG laser trabeculoplasty (selective laser trabeculoplasty): a multicenter, pilot, clinical study. Ophthalmology. 1998;105:2082–90. discussion 9–90
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Raj, S., Tigari, B., Faisal, T.T. et al. Efficacy of selective laser trabeculoplasty in primary angle closure disease. Eye 32, 1710–1716 (2018). https://doi.org/10.1038/s41433-018-0165-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-018-0165-5
This article is cited by
-
Micropulse laser trabeculoplasty on Chinese patients with glaucoma or ocular hypertension: average 35 months follow-up results
BMC Ophthalmology (2022)
-
Angle Closure Glaucoma—Update on Treatment Paradigms
Current Ophthalmology Reports (2022)
-
Selective laser trabeculoplasty is safe and effective in patients previously treated with prostaglandin analogs: An evidence-based review
International Ophthalmology (2022)