Abstract
Objectives
To provide evidence for long-term outcomes for margin-controlled excision of eyelid melanoma.
Methods
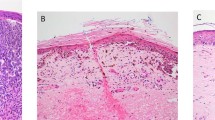
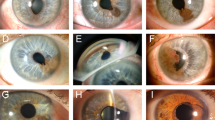
Retrospective single-centre observational case series of patients treated for eyelid melanoma between 2007 and 2016, with a minimum of 5-year follow-up. Tumour excision involved rush-paraffin en face horizontal sections and delayed repair (Slow Mohs; SM).
Results
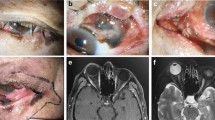
Twenty-two cases were seen with a survival of 91% (two deaths from nodular and lentigo maligna melanoma) and seven with melanoma in situ (MIS). Invasive melanoma includes eight lentigo maligna melanoma, four nodular, two amelanotic and one desmoplastic. Mean Breslow thickness was 6 mm for invasive (range 0.5–26). Mean excision margin for MIS was 3 mm (range 2–5 mm) and for invasive was 5 mm (range 2–10). Further excisions were performed in nine (41%); two went on to recur. Local recurrence was 36%; six invasive (27%) at a mean of 24 months (range 1.5–5 years) and two for MIS at a mean of 15 months (range 1–1.5 years). Imaging occurred for suspected advanced disease. Sentinel node biopsy was not performed. Advanced melanoma therapy was performed in two cases. No vitamin D testing occurred.
Conclusions
Survival rates are in line with 90% overall survival in the UK. Prescriptive excision margins are not applicable in the periocular region and margin-controlled excision with a delayed repair is recommended, but patients need to know further excision may be needed to obtain clearance. Evidence recommending vitamin D therapy needs to be put into clinical practice. In addition, upstaging of MIS occurred advocating excision rather than observation of MIS. More studies are needed to determine the best management of eyelid melanoma.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The patient data that support the findings of this study are available in Supplementary Table 1.
References
Larson DL, Larson JD. Head and neck melanoma. Clin Plast Surg. 2010;37:73–77.
Sanchez R, Ivan D, Esmaeli B. Eyelid and periorbital cutaneous malignant melanoma. Int Ophthalmol Clin. 2009;49:25–43.
Shields CL, Kels JG, Shields JA. Melanoma of the eye: revealing hidden secrets, one at a time. Clin Dermatol. 2015;33:183–96.
Saldanha G, Potter L, Daforno P, Pringle JH. Cutaneous melanoma subtypes show different BRAF and NRAS mutation frequencies. Clin Cancer Res. 2006;12:4499–505.
Chan FM, O’Donnell BA, Whitehead K, Ryman W, Sullivan TJ. Treatment and outcomes of malignant melanoma of the eyelid: a review of 29 cases in Australia. Ophthalmology. 2007;114:187–92.
Ahmed OA, Kelly C. Head and neck melanoma (excluding ocular melanoma): United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130:S133–S141.
Veronesi U, Cascinelli N, Adamus J, Balch C, Bandiera D, Barchuk A, et al. Thin stage I primary cutaneous malignant melanoma. Comparison of excision with margins of 1 or 3 cm. N Engl J Med. 1988;318:1159–62.
Esmaeli B, Youssef A, Naderi A, Ahmadi MA, Meyer DR, McNab A. Margins of excision for cutaneous melanoma of the eyelid skin: the Collaborative Eyelid Skin Melanoma Group Report. Ophthalmic Plast Reconstr Surg. 2003;19:96–101.
Zhu Z, Liu W, Gotlieb V. The rapidly evolving therapies for advanced melanoma–towards immunotherapy, molecular targeted therapy, and beyond. Crit Rev Oncol Hematol. 2016;99:91–99.
Kim A, Cohen MS. The discovery of vemurafenib for the treatment of BRAF-mutated metastatic melanoma. Expert Opin Drug Discov. 2016;11:907–16.
Michielin O, Hoeller C. Gaining momentum: new options and opportunities for the treatment of advanced melanoma. Cancer Treat Rev. 2015;41:660–70.
Saranga-Perry V, Ambe C, Zager JS, Kudchadkar RR. Recent developments in the medical and surgical treatment of melanoma. CA Cancer J Clin. 2014;64:171–85.
National Institute for Health and Care Excellence. Melanoma: assessment and management. https://www.nice.org.uk/guidance/ng14.
Malhotra R, Chen C, Huilgol SC, Hill DC, Selva D. Mapped serial excision for periocular lentigo maligna and lentigo maligna melanoma. Ophthalmology. 2003;110:2011–8.
Huilgol SC, Selva D, Chen C, Hill DC, James CL, Gramp A, et al. Surgical margins for lentigo maligna and lentigo maligna melanoma: the technique of mapped serial excision. Arch Dermatol. 2004;140:1087–92.
Then S-Y, Malhotra R, Barlow R, Kurwa H, Huilgol S, Joshi N, et al. Early cure rates with narrow-margin slow-Mohs surgery for periocular malignant melanoma. Dermatol Surg. 2009;35:17–23.
Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Long GV, Ross MI, et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:472–92.
Higgins HW II, Lee KC, Galan A, Leffell DJ. Melanoma in situ: Part I. Epidemiology, screening, and clinical features. J Am Acad Dermatol. 2015;73:181–90.
Kurtansky NR, Dusza SW, Halpern AC, Hartman RI, Geller AC, Marghoob AA, et al. An epidemiologic analysis of melanoma overdiagnosis in the United States, 1975-2017. J invest Dermatol. 2021;142:1804–11.e6.
Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004;54:8–29.
Chen ST, Geller AC, Tsao H. Update on the epidemiology of melanoma. Curr Dermatol Rep. 2013;2:24–34.
CRUK. Melanoma skin cancer mortality. 2021.
Downing A, Newton-Bishop JA, Forman D. Recent trends in cutaneous malignant melanoma in the Yorkshire region of England; incidence, mortality and survival in relation to stage of disease, 1993-2003. Br J Cancer. 2006;95:91–5.
Go CC, Kim DH, Go BC, McGeehan B, Briceño CA. Clinicopathologic characteristics and prognostic factors impacting survival in melanoma of the eyelid. Am J Ophthalmol. 2022;234:71–80.
Yin VT, Warneke CL, Merritt HA, Esmaeli B. Number of excisions required to obtain clear surgical margins and prognostic value of AJCC T category for patients with eyelid melanoma. Br J Ophthalmol. 2014;98:1681–5.
Jung S-K, Lim J, Yang S-W, Jee D, Won Y-J. Nationwide trends in the incidence and survival of eyelid skin cancers in Korea. Ophthalmic Epidemiol. 2020;27:438–48.
Garbe C, Amaral T, Peris K, Hauschild A, Arenberger P, Bastholt L, et al. European consensus-based interdisciplinary guideline for melanoma. Part 1: diagnostics - Update 2019. Eur J Cancer. 2020;126:141–58.
Karakousis CP, Balch CM, Urist MM, Ross MM, Smith TJ, Bartolucci AA. Local recurrence in malignant melanoma: long-term results of the multiinstitutional randomized surgical trial. Ann Surg Oncol. 1996;3:446–52.
Balch CM, Soong SJ, Smith T, Ross MI, Urist MM, Karakousis CP, et al. Long-term results of a prospective surgical trial comparing 2 cm vs. 4 cm excision margins for 740 patients with 1-4 mm melanomas. Ann Surg Oncol. 2001;8:101–8.
Gregory McKinnon J, Starritt EC, Scolyer RA, McCarthy WH, Thompson JF. Histopathologic excision margin affects local recurrence rate: analysis of 2681 patients with melanomas. Ann Surg. 2005;241:326–33.
Romano E, Scordo M, Dusza SW, Coit DG, Chapman PB. Site and timing of first relapse in stage III melanoma patients: implications for follow-up guidelines. J Clin Oncol. 2010;28:3042–7.
Friedman EB, Scolyer RA, Williams GJ, Thompson JF. Melanoma in situ: a critical review and re-evaluation of current excision margin recommendations. Adv Ther. 2021;38:3506–30.
Tzellos T, Kyrgidis A, Mocellin S, Chan A-W, Pilati P, Apalla Z. Interventions for melanoma in situ, including lentigo maligna. Cochrane Database Syst Rev. 2014:CD010308.
Hendrickx A, Cozzio A, Plasswilm L, Panje CM. Radiotherapy for lentigo maligna and lentigo maligna melanoma – a systematic review. Radiat Oncol. 2020;15:174.
Garbe C, Amaral T, Peris K, Hauschild A, Arenberger P, Bastholt L, et al. European consensus-based interdisciplinary guideline for melanoma. Part 2: treatment - update 2019. Eur J Cancer. 2020;126:159–77.
Hayes AJ, Maynard L, Coombes G, Newton-Bishop J, Timmons M, Cook M, et al. Wide versus narrow excision margins for high-risk, primary cutaneous melanomas: long-term follow-up of survival in a randomised trial. Lancet Oncol. 2016;17:184–92.
Secinti IE, Gursoy D, Erturk T, Dede I, Ozgur T, Dogan E. Should we report Breslow density, a new concept in cutaneous melanoma? Malays J Pathol. 2021;43:397–404.
Guhan S, Klebanov N, Tsao H. Melanoma genomics: a state-of-the-art review of practical clinical applications. Br J Dermatol. 2021;185:272–81.
Peach H, Board R, Cook M, Corrie P, Ellis S, Geh J, et al. Current role of sentinel lymph node biopsy in the management of cutaneous melanoma: a UK consensus statement. J Plast Reconstr Aesthet Surg. 2020;73:36–42.
Martin-Gorgojo A, Gilaberte Y, Nagore E. Vitamin D and skin cancer: an epidemiological, patient-centered update and review. Nutrients. 2021;13:4292.
De Smedt J, Van Kelst S, Boecxstaens V, Stas M, Bogaerts K, Vanderschueren D, et al. Vitamin D supplementation in cutaneous malignant melanoma outcome (ViDMe): a randomized controlled trial. BMC Cancer. 2017;17:562.
Cunha N, Campos S, Serrao V. Vitamin D levels in a cohort of Portuguese melanoma patients relate to time of follow-up from diagnosis, sun-exposure behaviour, and use of photoprotection. Eur J Dermatol. 2018;28:93–94.
Skobowiat C, Oak ASW, Kim T-K, Yang CH, Pfeffer LM, Tuckey RC, et al. Noncalcemic 20-hydroxyvitamin D3 inhibits human melanoma growth in in vitro and in vivo models. Oncotarget. 2017;8:9823–34.
Tang JY, Fu T, Leblanc E, Manson JE, Feldman D, Linos E, et al. Calcium plus vitamin D supplementation and the risk of nonmelanoma and melanoma skin cancer: post hoc analyses of the women’s health initiative randomized controlled trial. J Clin Oncol. 2011;29:3078–84.
Author information
Authors and Affiliations
Contributions
Design of study: JCB, AL, RM. Conduct of study, collection, management, analysis and interpretation of data: JCB, AL, RM. Manuscript preparation and final approval: JCB, AL, RM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bladen, J.C., Malhotra, R. & Litwin, A. Long-term outcomes of margin-controlled excision for eyelid melanoma. Eye 37, 1009–1013 (2023). https://doi.org/10.1038/s41433-023-02428-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-023-02428-9
This article is cited by
-
Surgical margins and outcomes for eyelid melanoma: a systematic review and meta-analysis
Archives of Dermatological Research (2024)