Abstract
Background/objectives
Patient safety is a global health priority, yet there is limited research into how ophthalmology is responding to this. There is evidence that a review of patient harm related to eye care and the associated patient safety incidents is needed. We aimed to characterise patient safety incidents involving eye care by: identifying the most frequently reported incidents involving clinical care; and characterising the nature of incidents leading to severe vision loss.
Methods
The data comprised patient safety incidents reported between 2018 and 2022 to the National Reporting and Learning System and the NHS England Learn from Patient Safety Events system. Reports were searched for eye-related terms (ICD-11) and those reports relating to implementation of care and clinical assessment were included. A descriptive analysis was undertaken to characterise the most frequent incident types and their contributory factors, followed by a thematic analysis of incidents relating to severe vision loss.
Results
Of the 836 reports identified, insufficient care (n = 416) and delayed diagnosis (n = 234) featured most. Patient harm occurred related to vision loss (n = 449), delays in treatment (n = 182), and disease progression (n = 121). Among 220 reports that resulted in severe vision loss, patients with Glaucoma and Age-related Macular Degeneration were impacted by delays in monitoring and management, loss to follow-up, disease progression due to insufficient care and system failures.
Conclusions
In this characterisation of eye-related incident reports in a national population, potential areas of interest toward safer eye care include addressing delays in patients receiving care and insufficient care such as inconsistent monitoring in glaucoma.
Similar content being viewed by others
Introduction
The improvement of patient safety is a global health priority, yet there is a paucity of evidence from research in eye care settings. Given the recent developments in eye care pathways in the UK, such as the transition of services from hospital to primary care [1,2,3,4], in addition to increasing demand on services, and the declining performance of the National Health Service (NHS [5]; it is essential that a detailed understanding of patient safety incidents in eye care is gained.
There are growing patient safety concerns in healthcare with around one in 20 patients exposed to preventable harm [6] and in primary care, greater levels of harm were associated with diagnostic and medication incidents [6,7,8]. Yet the prevalence and types of harm in eye care are not well described. Eye-related patient safety remains underrepresented in health-related policy, yet patient safety reporting was deemed a high-priority area for quality improvement related to eye disorders [9]. A limited body of literature on eye-related patient safety includes incidents in primary eye care [10], ophthalmic surgery [11,12,13,14,15], and emergency eye care [16]. The types of incidents reported in eye care resulted from delayed eye care [11, 15,16,17] and medication errors [11, 13]. For quality of care to improve, a detailed knowledge of the frequency of occurrence and nature of harm in eye care is needed to allow the development of strategies for prevention.
The Learn from Patient Safety Events (LFPSE; previously England and Wales National Reporting and Learning System, NRLS) is the largest database of patient safety incidents in the world and receives more than 2.5 million reports each year from national NHS healthcare providers. The LFPSE or NRLS database has been investigated widely in primary care in general practice [18, 19]; for medication incidents [20, 21]; in hospitals [22]; orthopaedic surgery [23]; dentistry [24]; and mental health [25]. However, the nature and severity of eye-related safety incidents reported through the NRLS and LFPSE are unknown.
The aim of this study was to understand the nature of reported patient safety incidents in eye care. The objectives were firstly to identify the most frequently reported incidents involving the implementation of care and clinical assessment. The second objective was to characterise the nature of those incidents leading to severe vision loss and identify potential areas as to where and how safer care may be delivered within eye care within the reports.
Methods
Study design
An exploratory multi-methods analysis of incident reports about eye care was undertaken. The definition of a patient safety incident is “any unintended or unexpected incidents that could have, or did, lead to harm for one or more patients receiving health care” [26]. The use of incident reports as a data source allows an understanding to be gained of the events that occurred and the reporter’s perception as to why. Data coding and exploratory data analysis can be used to identify the most frequently reported incidents [27], in addition to a thematic analysis [28, 29] to determine themes about why incidents occur.
Study population
The NRLS and LFPSE database contained fully anonymised reports from healthcare professionals, who have a responsibility to report incidents to healthcare organisations. Data held in each report included location, patient demographics, reported severity of harm, and a ‘free-text’ description of the incident and possible contributory factors.
The study population comprised all patient safety incident reports relating to eye care from incidents reported to the NRLS and LFPSE between January 2018 and May 2022. Incidents reported before September 2021 were from England and Wales, and those reported thereafter were from England only. Eye-related reports were identified at the data source through relevant search terms based on the World Health Organization International Classification of Disease codes (ICD-11), encompassing eye and visual system relevant pathology and trauma (see Table S1), and were then shared with the researchers. Codes from ICD-11 were used to encompass a broad range of relevant terminology. The search terms were applied to the free-text description of the incident.
The search results were coded using an empirically developed multi-axial framework, the ‘PatIent Safety (PISA) classification system’, which has been used to analyse over 75,000 incident reports across a range of health and social care contexts [27]. We adopted an internationally established multi-methods approach to generate learning from patient safety incidents [27, 30]. Those incidents categorised under implementation of care and clinical assessment formed the sample for analysis. Incidents relating to implementation of care and clinical assessment (pre-designated categories within the data supplied) were selected based on their encompassing nature as broadly representative of general issues which may occur in the patient journey in eye care. Four categories were chronologically coded according to: incident type, contributory factors, incident outcome and incident severity as reported [27]. Additionally, the incident severity was graded by the researchers according to a classification system aligned with the WHO classification ([31]; Table 1) and previously validated [27, 30].
Analysis
Reports were included if they met the definition of a patient safety incident [26], and contained sufficient information to determine what happened and to determine the causes of the incident. Reports were excluded if they were not related to eye care.
The analysis of the reports involved 3 stages: [27]
Firstly, familiarisation and data coding consisted of reviewing the free text within each report and applying codes systematically to describe incident type, potential contributory factors, level and type of harm. Codes were applied using a previously derived codebook [30] with the addition of new codes as needed, with consensus in the research team upon implementation. Regular meetings were held to review codes, with arbitration with trained researchers as needed to ensure uniformity of coding.
Secondly, generation of data summaries involved the use of descriptive statistical analysis. Pivot tables in Excel (Microsoft Corp., Redmond, WA, USA) were used to cross-tabulate level of harm with incident type, and contributory factor and incident type.
Thirdly, interpretation of themes and learning, in which patient safety themes were identified and explained by gaining an understanding of the events leading up to it and contributory factors, and specific contexts.
To address the second objective, incident reports were selected for thematic analysis if they included sufficient information to carry out a descriptive analysis; if the outcome for the patient resulted in vision loss; and if they were categorised under the most severe level of harm. The selection was made to gain an understanding of the perceived circumstances which may lead to an outcome that is often perceived as the worst for patients [32]. Free-text data were analysed using NVivo (version 1.7.1; QSR International) to identify and prioritise the safety problems through the identification of recurring themes and subthemes. Patterns in the coding were identified through discussion between the researchers (CYL, JF, JHA) and an iterative approach was adopted to develop the themes with input from the wider team (JM).
The researchers (CYL, JF, JHA) had undergone training in incident analysis, classification, and root cause analysis, including simulation with practice cases, as described previously [27]. One researcher conducted all coding, and a second researcher reviewed a 20% random sample of codes. Inter-rater reliability was calculated using Cohen’s kappa coefficient, with a kappa value of greater than or equal to 0.7 used to indicate moderate-high agreement. Differences in coding were resolved through discussion and arbitration with a senior investigator.
The reporting adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Table S2) and the Standards for Reporting Qualitative Research (SRQR; Table S3).
Results
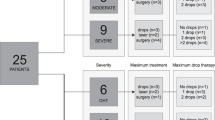
NHS England provided 5000 reports for processing (Table S4) and following filtering by incident category for implementation of care and clinical assessment, a sample of 1302 reports was identified for analysis. After initial review, 836 were included in the quantitative analysis. Incidents were excluded on the basis of lack of relevance to eye care (n = 457) or lack of sufficient detail (n = 9; Fig. 1).
Table 1 shows the definitions of harm and the number of reports that describe the level of harm.
A Cohen’s kappa coefficient of 0.85 for inclusion or exclusion of incident reports between two coders, indicated high inter-rater reliability.
Most frequently reported incident types and outcomes
Insufficient treatment/care/monitoring given (n = 416, 50%), delayed diagnosis (n = 234, 28%), wrong diagnosis (n = 46, 6%), insufficient assessment (n = 46, 6%), and implementation issues conducting the correctly chosen process or procedure were most frequently observed among the reports (n = 43, 5%; Table 2). The most frequent outcomes reported for patients included vision loss (n = 449, 54%), delays in management assessment or treatment (n = 182, 22%), and general deterioration/ progression of condition (n = 121, 14%). These three outcomes also represented the outcomes with the greatest level of harm (severe harm) reported. Of all the incidents, 41% resulted in either no harm or low harm (n = 344), and 59% were assigned a code from low to severe harm (n = 492). Incidents with the outcome of vision loss, coded as moderate or severe harm (n = 372) were mainly due to insufficient treatment/care/monitoring given (n = 194, 52%) or delayed diagnoses (n = 122, 33%).
Relationship between incident type and contributory factors
The most frequent contributory factors reported involved poor continuity of care, seen frequently with appointments being cancelled by the hospital without patient’s knowing (n = 365, 44%); inadequate skillsets or knowledge related to incidents, such as patients being referred to the wrong clinics (n = 222, 27%); and long waits for service, such as delayed appointments (n = 51, 6%). The relationships incident type and contributory factors are shown in Table 3.
Reported issues with continuity of care featured the most when insufficient treatment/care/monitoring occurred (n = 274, 66%). Whilst an inadequate skill set or knowledge, and continuity of care, contributed the most to delayed diagnoses (n = 95, 41% and n = 64, 27%, respectively) within reports.
Interestingly, among incidents reported involving insufficient treatment/care/monitoring, only 26 (6%) incidents were perceived to be related to the COVID-19 pandemic.
Themes from incidents resulting in the most serious harm in which vision loss occurred
Of the 836 incident reports, 220 incident reports were selected for thematic analysis on the basis of those with the greatest severity of harm in which vision loss occurred.
Three key themes were identified (Table 4, additional themes in Table S5).
Theme 1: delay or loss to follow up resulting in severe sight loss in individuals with glaucoma or AMD
Progression from delayed care featured in reports describing patients with glaucoma and AMD, in which severe vision loss occurred in 71.0% and 72.7% of incidents, respectively (n = 76 and n = 24). Of those with AMD, nearly half of the patients (n = 15, 45.4%) experienced loss of vision due to delayed care. For example, a patient with glaucoma was transferred to another clinic and a failure to detect visual field loss led to disease progression.
Delays in care, diagnosis or follow up resulted in a decrease in visual function or other worsening of their condition and were considered within this theme. The importance of disease progression due to patients being lost to follow up is highlighted by the impact on the patient, given that many eye conditions can result in irreversible loss of vision if left untreated. In one case where AMD was left untreated, loss of vision resulted (Table 4, quote T1.1).
In another example, a patient with glaucoma experienced a delayed follow up of years (rather than months) resulting in a dramatic vision loss, with severe consequences on the patient’s quality of life and their ability to maintain independence (Table 4, quote T1.2).
In many cases reported, visual acuity (VA) deteriorated to the most extreme levels of sight impairment at “count fingers”, “hand motion”, “light perception”, or “no light perception”, with permanent and complete loss of vision in extreme cases. Several incident reports described the progression of an eye condition when left untreated, and further conditions included diabetic retinopathy, and retinal detachment (Table 4, quote T1.3-4).
Several reports described patients being lost to follow up and causing a delay in accessing eye care for management, assessment or treatment. No further appointment was booked until they contacted the hospital and frequently patients suffered from this long wait (Table 4, quote T1.5).
Theme 2: progression of glaucoma and AMD due to insufficient care
This theme describes incidents that report any form of insufficient care, such as staff not acting on progression of a disease or not assessing the patient adequately and includes both inappropriate monitoring as well as inappropriate management. Inappropriate monitoring occurred in more than half of the reports concerning patients with glaucoma (n = 27, 56.3%).
Inappropriate monitoring Key assessments (n = 8, 29.6%) and tests not being performed (n = 9, 33.3%) accounted for the majority of the cases involving insufficient monitoring resulting in glaucomatous progression. In 77.8% of cases, longitudinal monitoring was not appropriately undertaken and led to severe vision loss (Table 4, quote T2.1).
In one unusual report involving a misdiagnosis, which appeared to be an extreme combination of incidents. The patient presented with glaucoma and was prescribed topical treatment. On subsequent visits, it was thought that the glaucoma had progressed, and the patient was given additional eye drops to control intraocular pressure. The patient’s vision later deteriorated and attributed to the formation of cataract at first, and later a choroidal melanoma (Table 4, quote T2.2).
Other examples of insufficient care of patients with AMD included, for example, tests which were not performed or was interpreted incorrectly, resulting in progression of AMD, and inappropriate management was described in six cases (28.6%). In one example of a test not being performed for a patient with AMD, there was a delay in detecting loss of vision (Table 4, quote T2.3).
Inappropriate management Inappropriate management of patients with glaucoma and AMD was described in 21 and 12 cases, respectively, with a half and two-thirds, respectively, of these patients experiencing severe loss in vision. In some instances, no treatment was administered by staff, which occurred in 23.8% of glaucoma cases involving inappropriate management (Table 4, quote T2.4.). Treatment of glaucoma was stopped by staff in five reports, with two cases of severe vision loss (Table 4, quote T2.5).
Theme 3: system failures
System failures included any incidents that resulted from staffing issues, protocol incidents or any infrastructure and integration issues, for example, staff capacity, a lack of clinical guidelines or problems with scheduling.
Infrastructure and integration issues
Glaucoma appointments being cancelled by the hospital (n = 10, 17.9%) and lack of capacity (n = 10, 17.9%) in hospitals were frequent causes (Table 4, quote T3.1.). Of the 10 cancellations made by hospitals, only three reports provided a reason about why the appointment was cancelled; one was due to staff on annual leave and two being COVID-19 related. Further, a patient with AMD was lost to follow up due to inadequate protocols, as well as a lack of training (Table 4, quote T3.2).
Accessing healthcare staff
Seven cases (7.7%) involved patients with glaucoma attempting to contact the hospital, with some informing the hospital of their symptoms, yet were still not seen in a timely manner. For example, a patient sought help for their deteriorating vision but was unable to secure an appointment (Table 4, quote T3.3).
Referral incidents
Reports describing referral incidents for patients with glaucoma occurred in 6.0% (n = 5) of cases, in which either no referral was made, or an incorrect referral time frame resulted in disease progression. In one example, a patient’s intraocular pressures became dangerously high due to a lack of proper referral at the appropriate time (Table 4, quote T3.4.):
For patients with AMD, reports describing referral incidents accounted for 20.5% (n = 8) of incidents describing disease progression due to system failures. All reports describing incidents in referrals resulted in patients experiencing severe vision loss (Table 4, quote T3.5.). Referrals not being made despite progression of the AMD also occurred (Table 4, quote T3.6).
Protocol incidents
Absent glaucoma management protocols were described frequently (n = 8, 42.1%), followed by inadequate protocols (n = 5, 26.3%), and changes in protocol (n = 4, 21.1%). Change in protocol referred to incidents in which changes to pre-existing protocols led to a patient safety incident (Table 4, quote T3.7).
Discussion
The findings present a characterisation of eye-related incident reports occurring in a national population and include a qualitative analysis of the incidents resulting in severe harm and vision loss. Given the lack of research in patient safety in eye care, the results highlight the importance of and the need for an evidence base to underpin the learning from incidents that must be recognised in order to improve systems in eye care.
The key findings indicated that insufficient care was the most frequently reported type of incident, and such incidents caused the most severe harm to the patients. The most common contributory factor reported was continuity of care. Of the themes identified in those reports resulting in the most serious harm in which vision loss occurred, patients with glaucoma and AMD were impacted by delays or loss to follow up, insufficient care, and system failures. For example, unacceptably long delays in issuing follow up appointments, due to scheduling issues, resulted in significant and in some cases, potentially avoidable, disease progression. The findings highlight insufficient care, continuity of care, system failures and delayed diagnosis as priority areas for detailed evaluation and for the development of patient safety interventions, with a focus on patients with glaucoma and age-related macular degeneration.
The most frequently reported incident types included those from insufficient care and delayed diagnosis. For example, missed medications provided to patients with eye infections due to low staffing was categorised as insufficient care and delayed diagnosis were linked to lack of monitoring in some cases. Delays in eye care are evident in previous findings in patients experiencing sight loss, with lack of capacity cited as a major reason for delay [33]. Furthermore, delays and loss to follow up were identified in a study involving clinical record review in a hospital eye care setting, in which over half of incidents were a result of incomplete administrative processes [17]. Consistent with a review of safety incidents relating to ocular anti-vascular endothelial growth factor injections, delays were among the severe causes of harm identified, alongside intraocular inflammation or infection, with recommendations put forward involving system level planning, checklists and electronic records [34].
In the present study, a frequently reported contributory factor included issues with continuity of care, in which patients suffered vision loss due to appointment scheduling issues. Also, many patients suffered vision loss from appointments not being booked when requested, or appointments being cancelled and not rebooked. Consistent with previous findings, loss of medical records, failure to plan procedures, or transfer of care through paper referrals contributed to harmful outcomes [35]. Previous research has identified contributing factors to loss to follow up including patient non-attendance, hospital cancellation, and rescheduling and capacity issues [17]. Loss to follow up is a major problem in chronic diseases such as glaucoma when irreversible progression occurs before a patient becomes symptomatic, resulting in significant vision loss. Previous studies showed that 8% of glaucoma patients experience disease progression that could have been prevented with prompt follow-up [36]. A mixture of waiting list audits, triage guidelines, non-medical led clinics, a clear non-attendance policy, a specialist lead nurse role and a patient-focussed booking system was found to be effective in reducing loss to follow-up [37].
The findings from the reports included demonstrated that the severest level of harm most often affected patients with glaucoma and age-related macular degeneration. Given the high prevalence of these conditions, it is unsurprising that these findings mirror those in a similar population of patients [33]. In the present study, delays in management, assessment or treatment were a frequent outcome but mostly resulted in low or no harm. In other research, difficulties around delays due to appointment rescheduling in glaucoma services were associated with more serious harm [36] and the severity of unnecessary delays in urgent eye care settings has been highlighted [38].
System failures were evidenced in the data and included protocol errors, and staffing and infrastructure issues. Such challenges are mirrored by Davis et al. [17], but are not unique to eye care and have been demonstrated in other areas e.g. anaesthetic practice [39], endoscopic procedures [40] and medications safety [41]. Interventions addressing system failures, including implementation of protocol changes or standard operating procedures, were reported to reduce the number of incidents [12, 42, 43].
It is acknowledged that incidents are under-reported and may represent only a small proportion of the true problems in a system and can be limited in narrative content [30]. Like any incident reporting system, the NRLS and LFPSE are subject to potential reporting biases. The findings are essentially hypothesis-generating, and inductive, requiring testing and development in further studies and serve as potential areas of interest for improvement efforts in clinical practice.
Conclusion
The findings highlight delays in patients receiving eye care as well as insufficient care, with severe levels of harm particularly impacting on patients with glaucoma and age-related macular degeneration. This study marks an important step in identifying priority issues for quality improvement and serves as a starting point for determining the areas of development. Given the restructuring of eye care services in the UK and increased clinical responsibility for some eye care clinicians, it is essential to promote a patient safety culture, such that everyone involved adheres to the safety guidelines toward improving the efficiency and effectiveness of patient pathways.
Summary
What was known before
-
Despite patient safety being a global health priority for over two decades, there has been little focus on eye health safety.
What this study adds
-
The study represents the largest characterisation of eye-related incident reports from the National Reporting and Learning System and the NHS England Learn from Patient Safety Events system specifically focused on clinical assessment.
-
Delays in patients receiving eye care as well as insufficient care, with severe levels of harm particularly impacting on patients with glaucoma and age-related macular degeneration are apparent potential priority issues for safety improvement.
-
Care systems are complex and routine safety data can provide a critical steer to where and how they can be improved.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to the nature of the data, and data sharing agreement with NHS England.
References
Baker H, Ratnarajan G, Harper RA, Edgar DF, Lawrenson JG. Effectiveness of UK optometric enhanced eye care services: a realist review of the literature. Ophthalmic Physiol Opt. 2016;36:545–57.
El-Abiary M, Loffler G, Young D, Strang N, Lockington D. Assessing the effect of independent prescribing for community optometrists and referral rates to hospital eye services in Scotland. Eye. 2021;35:1496–503.
Jonuscheit S, Geue C, Laidlaw R, Fischbacher C, Melia B, Lewsey J, et al. Towards transforming community eye care: an observational study and time-series analysis of optometrists’ prescribing for eye disorders. Public Health. 2021;196:107–13.
Roberts HW, Rughani K, Syam P, Dhingra S, Ramirez-Florez S. The Peterborough scheme for community specialist optometrists in glaucoma: results of 4 years of a two-tiered community-based assessment and follow-up service. Curr Eye Res. 2015;40:690–6.
Darzi A. Department of Health and Social Care. Independent investigation of the NHS in England. 2024. https://www.gov.uk/government/publications/independent-investigation-of-the-nhs-in-england [accessed 25 Nov 2024].
Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ. 2019;366:l4185. https://doi.org/10.1136/bmj.l4185.
Hodkinson A, Tyler N, Ashcroft DM, Keers RN, Khan K, Phipps D, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC Med. 2020;18:313. https://doi.org/10.1186/s12916-020-01774-9.
Singh H, Meyer AN, Thomas EJ. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. BMJ Qual Saf. 2014;23:727–31.
NICE 2018 https://www.nice.org.uk/guidance/QS180/history accessed 16 May 2024
MacFarlane E, Carson-Stevens A, North R, Ryan B, Acton J. A mixed-methods characterisation of patient safety incidents by primary eye care practitioners. Ophthalmic Physiol Opt. 2022;42:1304–15. https://doi.org/10.1111/opo.13030.
Kelly S, Jalil A. Wrong intraocular lens implant; learning from reported patient safety incidents. Eye. 2011;25:730–4. https://doi.org/10.1038/eye.2011.22.
Loh H, de Korne D, Chee S, Mathur R. Reducing wrong intraocular lens implants in cataract surgery: 3 years of experience with the SEIPS framework in Singapore. Int J Health Care Qual Assur. 2017;30:492–505. https://doi.org/10.1108/IJHCQA-06-2016-0095.
Mak S. Sentinel events in ophthalmology: experience from Hong Kong. J Ophthalmol. 2015;2015:1–6. https://doi.org/10.1155/2015/454096.
Steeples L, Hingorani M, Flanagan D, Kelly S. Wrong intraocular lens events—what lessons have we learned? A review of incidents reported to the National Reporting and Learning System: 2010–2014 versus 2003–2010. Eye. 2016;30:1049–55. https://doi.org/10.1038/eye.2016.87.
Wong S, Kelly S, Sullivan P. Patient safety in vitreoretinal surgery: quality improvements following a patient safety reporting system. Br J Ophthalmol. 2012;97:302–7. https://doi.org/10.1136/bjophthalmol-2012-301988.
Buchan JC, Ashiq A, Kitson N, Dixon J, Cassels-Brown A, Bradbury JA. Nurse specialist treatment of eye emergencies: five year follow up study of quality and effectiveness. Int Emerg Nurs. 2009;17:149–54. https://doi.org/10.1016/j.ienj.2008.12.002.
Davis A, Baldwin A, Hingorani M, Dwyer A, Flanagan D. A review of 145 234 ophthalmic patient episodes lost to follow-up. Eye. 2016;31:422–9. https://doi.org/10.1038/eye.2016.225.
Bell BG, Campbell S, Carson-Stevens A, Evans HP, Cooper A, Sheehan C, et al. Understanding the epidemiology of avoidable significant harm in primary care: protocol for a retrospective cross-sectional study. BMJ open. 2017;7:e013786.
Cooper A, Carson-Stevens A, Cooke M, Hibbert P, Hughes T, Hussain F, et al. Learning from diagnostic errors to improve patient safety when GPs work in or alongside emergency departments: incorporating realist methodology into patient safety incident report analysis. BMC Emerg Med. 2021;21:139. https://doi.org/10.1186/s12873-021-00537-w.
Cousins DH, Gerrett D, Warner B. A review of medication incidents reported to the National Reporting and Learning System in England and Wales over 6 years (2005-2010). Br J Clin Pharmacol. 2012;74:597–604.
Alqenae FA, Steinke D, Carson-Stevens A, Keers RN. Analysis of the nature and contributory factors of medication safety incidents following hospital discharge using National Reporting and Learning System (NRLS) data from England and Wales: a multi-method study. Ther Adv Drug Saf. 2023;14:20420986231154365. https://doi.org/10.1177/20420986231154365.
Howell AM, Burns EM, Bouras G, Donaldson LJ, Athanasiou T, Darzi A. Can patient safety incident reports be used to compare hospital safety? Results from a quantitative analysis of the English National Reporting and Learning System Data. PLoS One. 2015;10:e0144107.
Panesar SS, Carson-Stevens A, Salvilla SA, Patel B, Mirza SB, Mann B. Patient safety in orthopedic surgery: prioritizing key areas of iatrogenic harm through an analysis of 48,095 incidents reported to a national database of errors. Drug, Healthc Patient Saf. 2013;5:57–65.
Ensaldo-Carrasco E, Carson-Stevens A, Cresswell K, Bedi R, Sheikh A. Developing agreement on never events in primary care dentistry: an international eDelphi study. Br Dent J. 2018;224:733–40.
D’Lima D, Archer S, Thibaut BI, Ramtale SC, Dewa LH, Darzi A. A systematic review of patient safety in mental health: a protocol based on the inpatient setting. Syst Rev. 2016;5:203. https://doi.org/10.1186/s13643-016-0365-7.
NHS England, https://www.england.nhs.uk/patient-safety/patient-safety-insight/learning-from-patient-safety-events/report-patient-safety-incident/ accessed 16 May 2024
Carson-Stevens A, Hibbert P, Avery A, Butlin A, Carter B, Cooper A, et al. A cross-sectional mixed methods study protocol to generate learning from patient safety incidents reported from general practice. BMJ Open. 2015;5:e009079. 10.1136/bmjopen-2015-009079
Boyatzis RE Transforming qualitative information: thematic analysis and code development. 1998;1st edn. Sage Publications, Inc
Leinhardt G, Leinhardt S. Exploratory data analysis: new tools for the analysis of empirical data. Rev Res Educ. 1980;8:85–157
Carson-Stevens A, P Hibbert, H Williams, HP Evans, A Cooper, P Rees, et al. Characterising the nature of primary care patient safety incident reports in the England and Wales National Reporting and Learning System: a mixed-methods agenda-setting study for general practice. Southampton (UK): NIHR Journals Library; 2016. PMID: 27656729.
World Health Organization. Conceptual Framework for The International Classification for Patient Safety, Version 1.1. Geneva: World Health Organization; 2009.
Gualandi R, Masella C, Piredda M, Ercoli M, Tartaglini D. What does the patient have to say? Valuing the patient experience to improve the patient journey. BMC Health Serv Res. 2021;21:347.
Foot B, MacEwen C. Surveillance of sight loss due to delay in ophthalmic treatment or review: frequency, cause and outcome. Eye. 2017;31:771–5.
Kelly SP, Barua A. A review of safety incidents in England and Wales for vascular endothelial growth factor inhibitor medications. Eye. 2011;25:710–6.
Callen JL, Alderton M, McIntosh J. Evaluation of electronic discharge summaries: a comparison of documentation in electronic and handwritten discharge summaries. Int J Med Inform. 2008;77:613–20. https://doi.org/10.1016/j.ijmedinf.2007.12.002.
Tatham A, Murdoch I. The effect of appointment rescheduling on monitoring interval and patient attendance in the glaucoma outpatient clinic. Eye. 2012;26:729–33. https://doi.org/10.1038/eye.2012.22.
Schoch PA, Adair L. Successfully reforming orthopaedic outpatients. Aust Health Rev. 2012;36:233–7. https://doi.org/10.1071/ah11040.
Swystun AG, Davey CJ. A prospective evaluation of the clinical safety and effectiveness of a COVID‐19 urgent eyecare service across five areas in England. Ophthalmic Physiol Opt. 2022;42:94–109.
Cassidy CJ, Smith A, Arnot‐Smith J. Critical incident reports concerning anaesthetic equipment: analysis of the UK National Reporting and Learning System (NRLS) data from 2006–2008. Anaesthesia. 2011;66:879–88.
Ravindran S, Matharoo M, Rutter MD, Ashrafian H, Darzi A, Healey C, et al. Patient safety incidents in endoscopy: a human factors analysis of nonprocedural significant harm incidents from the National Reporting and Learning System (NRLS). Endoscopy. 2024;56:89–99.
Alrowily A, Alfaraidy K, Almutairi S, Alamri A, Alrowily W, Abutaleb M, et al. Investigating safety incidents with high-risk medications: insights from the National Reporting and Learning System (NRLS) on opioids, insulins, and anticoagulants. 2024. https://doi.org/10.21203/rs.3.rs-4115984/v1.
Patel SV, Olsen TW, Hinchley RL, Whipple DC, Kor TM. Improving patient safety in a high-volume intravitreal injection clinic. Ophthalmol Retin. 2022;6:495–500.
John DA, Hansemann B, Lieu P, Weizer J. Reducing injection-related safety events in retina clinics. Clin Ophthalmol. 2022;16:1255–9.
Acknowledgements
The authors wish to thank Mr Stuart Hellard, funded by PRIME Centre Wales, for data services.
Funding
Professor Andrew Carson-Stevens is supported by PRIME Centre Wales, funded by Health and Care Research Wales, Welsh Government.
Author information
Authors and Affiliations
Contributions
JHA was responsible for study conception, design, literature review, interpretation of results, and preparation of manuscript. JHA, CYL and JWF were responsible for data analysis. JM and ACS contributed to conception, design, analysis and interpretation of results. All authors contributed to manuscript preparation, reviewing of results and approving the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
All incident reports were screened to remove all identifiable data prior to receipt by the researchers. Given the anonymised nature of the dataset, no formal ethical approval was required for this study. There was no patient involvement. The study protocol was reviewed by NHS Improvement as part of the data-sharing agreement (ref. 5250). Incident reports used for the study are available, by application, from the NRLS and LFPSE. The ID’s of all reports used for the study can be provided upon reasonable request.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Acton, J.H., McFadzean, J., Lau, C.Y. et al. Patient safety in eye care: a multi-method analysis of reported incidents involving implementation of care and clinical assessment in England and Wales. Eye 39, 1486–1494 (2025). https://doi.org/10.1038/s41433-025-03669-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03669-6