Abstract
Dry eye disease (DED) is a complex condition characterized by tear film instability, inflammation, and neurosensory abnormalities. The efficacy of Botulinum toxin A (BTX-A) in treating DED is unknown. A systematic search was conducted across PubMed, the Cochrane Library, Scopus, Web of Science, and Embase databases for studies published until December 2024. Inclusion criteria encompassed randomized controlled trials (RCTs) and non-RCTs examining BTX-A’s effects on DED, with TBUT, Schirmer test scores, tear meniscus height (TMH), and OSDI as primary outcomes. Data were synthesized using fixed and random-effects models, accounting for heterogeneity. Fourteen studies (total n = 634 patients) were included. This meta-analysis evaluates the effectiveness of BTX-A in improving outcomes for DED. In 10 studies with 513 participants, BTX-A significantly improved TBUT by 1.79 s (95% CI: 1.48 to 2.10, p < 0.00001), Schirmer test scores by 3.72 mm (95% CI: 3.50 to 3.95, p < 0.00001), and OSDI scores by −7.51 (95% CI: −10.76 to −4.26, p < 0.00001). TMH increased by 0.10 mm (95% CI: 0.08 to 0.11, p < 0.00001). This meta-analysis demonstrates that BTX-A effectively improves clinical outcomes in DED. Post-treatment, TBUT increased by 1.79 s, Schirmer test scores improved by 3.72 mm, OSDI scores decreased by −7.51 points, and TMH increased by 0.10 mm, reflecting enhanced tear stability, production, and symptom relief. These findings support the use of BTX-A in clinical practice as a promising treatment for DED.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Zemanová M. Dry eye disease. A review. Cesk Slov Oftalmol. 2021;77:107–19.
The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.
Chen KY, Lee HK, Chan HC, Chan CM. Is multiwavelength photobiomodulation effective and safe for age-related macular degeneration? A systematic review and meta-analysis. Ophthalmol Ther. 2025. https://doi.org/10.1007/s40123-025-01119-w.
Sekar P, Hsiao G, Hsu SH, Huang DY, Lin WW, Chan CM. Metformin inhibits methylglyoxal-induced retinal pigment epithelial cell death and retinopathy via AMPK-dependent mechanisms: reversing mitochondrial dysfunction and upregulating glyoxalase 1. Redox Biol. 2023;64:102786.
Bron AJ, Tomlinson A, Foulks GN, Pepose JS, Baudouin C, Geerling G, et al. Rethinking dry eye disease: a perspective on clinical implications. Ocul Surf. 2014;12:S1–31.
Ablamowicz AF, Nichols JJ. Ocular surface membrane-associated mucins. Ocul Surf. 2016;14:331–41.
Vidal-Rohr M, Craig JP, Davies LN, Wolffsohn JS. Classification of dry eye disease subtypes. Cont Lens Anterior Eye. 2024;47:102257.
Sheppard J, Shen Lee B, Periman LM. Dry eye disease: identification and therapeutic strategies for primary care clinicians and clinical specialists. Ann Med. 2023;55:241–52.
Narang P, Donthineni PR, D’Souza S, Basu S. Evaporative dry eye disease due to meibomian gland dysfunction: Preferred practice pattern guidelines for diagnosis and treatment. Indian J Ophthalmol. 2023;71:1348–56.
Tsubota K, Yokoi N, Watanabe H, Dogru M, Kojima T, Yamada M, et al. A new perspective on dry eye classification: proposal by the Asia dry eye society. Eye Contact Lens. 2020;46:S2–s13.
Hodges RR, Dartt DA. Tear film mucins: front line defenders of the ocular surface; comparison with airway and gastrointestinal tract mucins. Exp Eye Res. 2013;117:62–78.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Dunn JD, Karpecki PM, Meske ME, Reissman D. Evolving knowledge of the unmet needs in dry eye disease. Am J Manag Care. 2021;27:S23–S32.
Evinger C, Bao JB, Powers AS, Kassem IS, Schicatano EJ, Henriquez VM, et al. Dry eye, blinking, and blepharospasm. Mov Disord. 2002;17:S75–78.
Shetty R, Sethu S. Newer paradigms in dry eye disease research. Indian J Ophthalmol. 2023;71:1064.
Gosal JS, Das KK, Khatri D, Attri G, Jaiswal AK. “Contralateral Dry Eye in Hemifacial Spasm:” A New Clinical Sign. Asian J Neurosurg. 2019;14:996–8.
Asiedu K, Kyei S, Mensah SN, Ocansey S, Abu LS, Kyere EA. Ocular surface disease index (OSDI) versus the standard patient evaluation of eye dryness (SPEED): a study of a nonclinical sample. Cornea. 2016;35:175–80.
Tagawa Y, Noda K, Ohguchi T, Ishida S, Kitaichi N. Corneal hyperalgesia in patients with short tear film break-up time dry eye. Ocul Surf. 2019;17:55–59.
Brott NR, Zeppieri M, Ronquillo Y. Schirmer Test. [Updated 2024 Feb 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559159/.
Miyake H, Kawano Y, Tanaka H, Iwata A, Imanaka T, Nakamura M. Tear volume estimation using a modified Schirmer test: a randomized, multicenter, double-blind trial comparing 3% diquafosol ophthalmic solution and artificial tears in dry eye patients. Clin Ophthalmol. 2016;10:879–86.
Baek J, Doh SH, Chung SK. Comparison of tear meniscus height measurements obtained with the keratograph and Fourier domain optical coherence tomography in dry eye. Cornea. 2015;34:1209–13.
Pena-Verdeal H, Garcia-Queiruga J, Sabucedo-Villamarin B, Garcia-Resua C, Giraldez MJ, Yebra-Pimentel E. A comprehensive study on tear meniscus height inter-eye differences in aqueous deficient dry eye diagnosis. J Clin Med. 2024;13.
Sundaram H, Signorini M, Liew S, Trindade de Almeida AR, Wu Y, Vieira Braz A, et al. Global aesthetics consensus: Botulinum toxin type A—evidence-based review, emerging concepts, and consensus recommendations for aesthetic use, including updates on complications. Plast Reconstr Surg. 2016;137:518e–529e.
Sahlin S, Linderoth R. Eyelid botulinum toxin injections for the dry eye. Dev Ophthalmol. 2008;41:187–92.
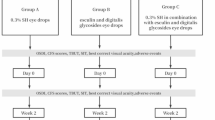
Lee AG, Lee SH, Jang M, Lee SJ, Shin HJ-. Transconjunctival versus transcutaneous injection of Botulinum toxin into the lacrimal gland to reduce lacrimal production: a randomized controlled trial. Toxins (Basel) 2021;13.
Chen KY, Chan HC, Wei LY, Chan CM. Efficacy of gabapentin and pregabalin for treatment of post refractive surgery pain: a systematic review and meta-analysis. Int Ophthalmol. 2024;44:409.
Ho RW, Fang PC, Chang CH, Liu YP, Kuo MT. A review of periocular Botulinum neurotoxin on the tear film homeostasis and the ocular surface change. Toxins (Basel) 2019;11:66.
Chen KY, Chan HC, Chan CM. Is retinal vein occlusion highly associated with an increased risk of myocardial infarction? A systematic review and meta-analysis. Int J Retin Vitreous. 2024;10. 86.
Chen KY, Chan HC, Chan CM. Is thermal pulsation therapy effective for dry eyes before and after cataract surgery? A systematic review and meta-analysis. Clin Ophthalmol. 2025;19:19–33.
NIH N. Study Quality Assessment Tools. NIH. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed October 25, 2024, 2024.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. 2019;366:14898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J. 2016;355:i4919.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12:55–61.
R Studio [computer program]. Version 2024.09.0 Build 375; 2024.
Serna-Ojeda JC, Nava-Castaneda A. Paralysis of the orbicularis muscle of the eye using botulinum toxin type A in the treatment for dry eye. Acta Ophthalmol. 2017;95:e132–e137.
Choi MG, Yeo JH, Kang JW, Chun YS, Lee JK, Kim JC. Effects of botulinum toxin type A on the treatment of dry eye disease and tear cytokines. Graefes Arch Clin Exp Ophthalmol. 2019;257:331–8.
Fouda SM, Mattout HK. Comparison between Botulinum toxin A injection and lacrimal punctal plugs for the control of post-LASIK dry eye manifestations: a prospective study. Ophthalmol Ther. 2017;6:167–74.
Choi EW, Yeom DJ, Jang SY. Botulinum Toxin A injection for the treatment of intractable dry eye disease. Medicina (Kaunas). 2021;57:247.
Ho MC, Hsu WC, Hsieh YT. Botulinum toxin type a injection for lateral canthal rhytids: effect on tear film stability and tear production. JAMA Ophthalmol. 2014;132:332–7.
Sawaed A, Friedrich SN, Farhan A, Nassar A, Hamed M, Hartstein M, et al. The effect of botulinum neurotoxin A injections on meibomian glands and dry eye. Ocul Surf. 2024;35:25–30.
Zhou Y, Wang W, Lin Z, Lin T, Gong L. Relations between nonmotor manifestations and motor disorders in patients with benign essential blepharospasm. Graefes Arch Clin Exp Ophthalmol. 2023;261:3615–23.
Isshiki Y, Ishikawa H, Mimura O. Changes in ocular higher-order aberrations following botulinum toxin treatment in patients with blepharospasm: BTX improves dry eye in patients with BEB. Jpn J Ophthalmol. 2016;60:486–91.
Yabumoto C, Osaki MH, Osaki T, Gameiro GR, Campos M, Osaki TH. Ocular surface metrics in blepharospasm patients after treatment with botulinum toxin injections. Ophthalmic Plast Reconstr Surg. 2023;39:475–8.
Jariyakosol S, Uthaithammarat L, Chatwichaikul N, Kasetsuwan N, Chongpison Y. Dry eye disease in hemifacial spasm patients treated with Botulinum toxin type A. Clin Ophthalmol. 2021;15:1775–82.
Park DI, Shin HM, Lee SY, Lew H. Tear production and drainage after botulinum toxin A injection in patients with essential blepharospasm. Acta Ophthalmol. 2013;91:e108–112.
Bayraktar Bilen N, Bilen Ş, Topçu Yılmaz P, Evren Kemer Ö. Tear meniscus, corneal topographic and aberrometric changes after botulinum toxin-a injection in patients with blepharospasm and hemifacial spasm. Int Ophthalmol. 2022;42:2625–32.
Chen KY, Chan HC, Chan CM. Do people with diabetes have a higher risk of developing postoperative endophthalmitis after cataract surgery? A systematic review and meta-analysis. J Ophthalmic Inflamm Infect. 2025;15:24.
Gunes A, Demirci S, Koyuncuoglu HR, Tok L, Tok O. Corneal and tear film changes after Botulinum toxin-a in blepharospasm or hemifacial spasm. Cornea. 2015;34:906–10.
Joonhyung Y, Kim JC. Effects of botulinum toxin type A for the treatment of dry eye syndrome and tear biomarkers. Invest Ophthalmol Vis Sci. 2017;58:5173.
Venkateswaran N, Hwang J, Rong AJ, Levitt AE, Diel RJ, Levitt RC, et al. Periorbital botulinum toxin A improves photophobia and sensations of dryness in patients without migraine: case series of four patients. Am J Ophthalmol Case Rep. 2020;19:100809.
Girard B, de Saint Sauveur G. Tear osmolarity, dry eye syndrome, blepharospasm and botulinum neurotoxin. J Fr Ophtalmol. 2021;44:1553–9.
Bukhari AA. Botulinum neurotoxin type A versus punctal plug insertion in the management of dry eye disease. Oman J Ophthalmol. 2014;7:61–65.
Chen KY, Chan HC, Chan CM. Is there an association between retinal vein occlusion and cerebrovascular accident? A systematic review and meta-analysis. BMC Ophthalmol. 2025;25:112.
Abe T, Loenneke JP. Orbicularis oculi muscle size and function: exploring the influence of aging and exercise training. Cosmetics. 2021;8:29.
Kim YS, Hong ES, Kim HS. Botulinum toxin in the field of dermatology: novel indications. Toxins (Basel). 2017;9:403.
Funding
No specific funding was received from any funding bodies in the public, commercial, or not-for-profit sectors to conduct the work described in this manuscript.
Author information
Authors and Affiliations
Contributions
K-Y C contributed to conceptualization, methodology, software, investigation, validation, writing the original draft, visualization, and formal analysis. H-C C was responsible for conceptualization, methodology and software. C-M C handled methodology, investigation, validation, supervision, and project administration. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable. This study does not involve individual data.
Ethics approval and consent to participate
Not applicable. This study does not involve human participants, human data or human tissue.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, KY., Chan, HC. & Chan, CM. Is Botulinum toxin A effective in treating dry eye disease? A systematic review and meta-analysis. Eye 39, 1457–1464 (2025). https://doi.org/10.1038/s41433-025-03790-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03790-6