Abstract
Proliferative Vitreoretinopathy (PVR) is the most common cause of surgical failure after retinal detachment (RD) repair, complicating up to 10% of spontaneous RD repairs and 50% of open globe injury-related RD. Early surgical intervention is currently the only intervention that reduces PVR incidence. An effective non-surgical intervention would be valuable in reducing PVR incidence and/or severity, particularly where access to surgery is limited or may be delayed. To define the evidence base for non-surgical management options to prevent and treat Proliferative Vitreoretinopathy (PVR) in retinal detachment and trauma, we searched PubMed, Clinicaltrials.gov, Medline and CINAHL for randomised controlled trials (RCTs) of non-surgical interventions to prevent or treat established PVR with no restriction on language or start date up until November 2024. All non-surgical interventions were considered with no restrictions. We considered outcomes of post-operative PVR (including retinal reattachment rate) and visual acuity and performed Risk of Bias (RoB) assessments using the Cochrane RoB2 tool. We identified 27 papers which included 1981 patients in studies of primary prevention and 1394 patients in studies of treatment of established PVR. While several studies of various agents individually demonstrated some improvements, the reviewers found concerns with RoB and the results were not replicated in the larger included studies. Multiple studies have investigated non-surgical interventions for PVR after RRD repair and trauma, but none have yet demonstrated clinically significant, repeatable benefits. Improved understanding of PVR pathobiology, along with larger prospective studies of existing preventative strategies may lead to the development of newer and more effective interventions.
Similar content being viewed by others
Introduction
Proliferative vitreoretinopathy (PVR) is a multifactorial fibroproliferative process involving an abnormal wound healing response characterised by the growth and contraction of cellular membranes within the vitreous cavity and on both sides of the retinal surface as well as intraretinal fibrosis [1]. PVR becomes clinically significant by causing progressive retinal detachment, reopening treated retinal breaks, creating new retinal breaks, or distorting the macula. It is common in cases of open globe injury (OGI) and is the most common cause for surgical failure after rhegmatogenous retinal detachment (RRD) repair. The incidence of PVR after repair of atraumatic RRD is 5–10% [2], and has remained largely unchanged in prospective studies despite the evolution of vitreoretinal techniques and improved understanding of clinical risk factors over the past 25 years [3]. One study reported that RRD occurred in 29% (26%–32% CI) of open globe injury (OGI) cases, of which 27% detached in the first 24 h, 47% within 1 week, and 72% within one month [4]. All such cases are at high risk of subsequently developing PVR, as demonstrated in other studies where PVR was already present in over 50% of ocular trauma cases who underwent vitrectomy within 10 days of injury [5, 6].
After RRD, the inflammatory ‘PVR cascade’ occurs with multiple steps, each representing potential therapeutic targets for pharmacological intervention. These include: retinal ischaemia with associated breakdown of the blood-retinal barriers, photoreceptor cell death and its associated inflammation, and retinal pigment epithelial (RPE) cell and retinal glial cell migration to the vitreous and inner retinal surfaces associated with the physical effects of trauma [1, 3, 7]. Blood-retinal barrier disruption, combined with retinal apoptosis, causes an increase in vitreous chemotactic and mitogenic factors [8], with influx of cytokines and growth factors from the systemic circulation and local production by infiltrating inflammatory cells that interact with retinal and RPE cells to further increase vitreous cytokine production [9]. Subsequent RPE epithelial-mesenchymal transition (EMT) to a fibroblastic phenotype generates cells with greater migratory capacity, invasiveness, contractability, resistance to apoptosis, and extracellular matrix production [10].
Severity of PVR is assessed and classified in clinical practice and research based on the ophthalmoscopic appearance, the subjective evaluation of the amount of membrane contraction and its distribution [11]. The initial classification by the Retina Society Terminology Committee subdivided PVR into four stages A, B, C and D from minimal to massive PVR [2], later modified in the updated classification to grades A, B and C, with Grade A being vitreous cells or haze, Grade B describing subclinical contraction or wrinkling and Grade C divided into Ca, anterior to the equator, and Cb, posterior to the equator [12]. Clinical outcomes may be assessed by retinal attachment status, visual acuity or by other clinical signs which act as markers or sequelae of PVR activity such as vitreous haze or epiretinal membrane formation.
PVR development involves a sequence of: retinal ischaemia, occurring immediately after detachment; photoreceptor apoptosis; and formation and subsequent contraction of fibrotic membranes [13]. Both ischaemia, apoptosis and the primary injury or retinal tear are associated with the release of pro-inflammatory, fibrogenic and mitogenic signalling molecules [14], which influence retinal pigment epithelial cells to proliferate and undergo epithelial-mesenchymal transition into fibroblasts and deposit collagen and ECM [13, 15, 16].
Pharmacologic interventions have targeted inflammation, cell proliferation, and fibrosis pathways, for instance: corticosteroid therapy targets broad inflammatory pathways; anti-VEGF therapies may be anti-inflammatory by inhibition of immune cell chemotaxis [17]; heparin modulates pro-fibrotic growth factors actions including FGF and VEGF [18]; and the various anti-metabolite and related drugs such as 5-fluorouracil (5-FU) and daunorubicin inhibit cell proliferation, and therefore fibroblast and immune cell proliferation. Nonetheless, PVR management remains challenging with no therapies in current clinical practice to prevent or reverse the disease process [3].
At present, there is only evidence to support vitrectomy (and its related procedures such as washout of vitreous haemorrhage, removal of established PVR membranes, retinopexy, and retinectomy) as an effective management for PVR [19]. A recent paper also suggests that prophylactic chorioretinectomy as part of vitrectomy may be effective in PVR prevention [20]. We will therefore attempt to define the evidence for non-surgical interventions in the primary prevention and treatment (including prevention/reduction of recurrence after surgery) of PVR after OGI and RRD which may mitigate the sight-threatening effects of PVR in situations where rapid access to vitrectomy may not be possible, such as in trauma patients who are temporarily unfit for general anaesthesia, in rural/austere environments or in conflict zones with prolonged casualty evacuation timelines.
This was accomplished by performing a systematic review of randomised controlled trial (RCT) data on non-surgical PVR treatments published in peer-reviewed journals up to the start of the review process in November 2024. The review was registered on PROSPERO (CRD42024610938).
Methods
This systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement [21].
Inclusion and exclusion criteria
Studies included were RCTs in any language or country of origin, published in an indexed medical journal up to November 2024. These studies evaluated interventions aiming either to prevent PVR in patients who had suffered OGI or RRD and undergone vitrectomy (primary prevention), or interventions used as an adjunct to improve visual outcomes or reduce PVR recurrence in patients who are undergoing vitrectomy for already established PVR (treatment). Exclusion criteria were non-RCT studies and studies of proliferative diabetic retinopathy.
Search strategy
Four scientific databases (PubMed, Clinicaltrials.gov, Medline and CINAHL) were searched using the search strings defined in the updated protocol including the MeSH term “vitreoretinopathy, proliferative” and others OR keyword PVR, as defined in the PROSPERO registration (CRD42024610938). Results were restricted to RCT as previously described [22]. The search strategy was changed from the original protocol in order to better capture the intended data. Two independent reviewers (GH and RJB) individually reviewed all titles from the initial searches, duplicates were eliminated and papers selected for full text review on the basis of the titles and abstracts using the Rayyan online tool for comparison [23]. Decisions on inclusion were made on the basis of full text review and disagreements resolved by discussion.
Data extraction
Data were extracted by two reviewers (GH and NM) working independently. Data extracted included intervention type, population targeted, primary and secondary outcomes as reported and any safety concerns. The primary outcomes that we aimed to report were anatomic success of retinal reattachment and visual acuity, without limit on duration of follow up.
Risk of bias
Risk of Bias assessment was carried independently out by two authors (GH, RJB) using the RoB2 tool [24], with disagreements resolved by discussion.
Results
Included studies
Twenty-seven studies [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52] met the inclusion criteria and were included in the review, which together included 3375 patients recruited to RCTs, separated into those aimed at the primary prevention of PVR after RRD or OGI (n = 1981) and the secondary treatment of PVR recurrence (n = 1394). These totals include numbers from one study, which included both primary prevention of PVR (n = 45) and secondary treatment (n = 45) [37]. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Fig. 1) demonstrates the study selection process.
Characteristics of included studies
Patient and study characteristics in the included studies are presented in Table 1. The mean age of included patients ranged from 9.6 to 68.53 years, however, only one paper [44] studied a population where >5% of the patients were under 18 years old. 68.3% were male (where gender information was available) and inclusion criteria varied from primary RRD to severe detachments with established PVR, both with and without a history of trauma. Some studies excluded patients for a wide range of criteria, normally related to other inflammatory processes such as autoimmune disease, diabetic retinopathy, glaucoma, chronic uveitis, or complex retinal detachments such as giant retinal tears.
Risk of bias of included studies
A risk of bias (RoB) assessment using the Cochrane RoB2 tool for each study is presented in Table 2. Concerns with reviewers relating to selection of reported results was the most common potential source of bias identified [26, 30, 32, 34, 35, 37, 39, 43, 45, 49,50,51,52], followed by deviation from the intended interventions [26, 29, 35,36,37, 39, 40, 43, 44, 51], both of which normally related to the lack of a pre-trial investigation and reporting plan. A common characteristic of studies that passed RoB screening with no concerns was studies that explicitly stated their aims and outcome measures prior to data collection and demonstrated adherence to their analysis plan [25, 27, 28, 31, 33, 41, 42, 46,47,48]. The selection of secondary outcomes with significant (or near-significant) differences between groups for reporting despite unclear clinical significance was a recurring concern [37, 39, 40, 45, 47, 48, 51].
Primary prevention of PVR after RRD
A summary of findings of the included RCT for primary prevention of PVR after RRD is presented in Table 3. Asaria et al. [27]. found a beneficial effect of 5-Fluorouracil (5-FU), an antimetabolite that inhibits synthesis and fibroblast proliferation, and Low Molecular Weight Heparin (LMWH), an anticoagulant that binds many growth factors, in 87 patients in the intervention group, who had lower rates of post-operative PVR and better visual acuity after detachment surgery, but no differences in the rates of reoperation. However, these results were not replicated in larger studies conducted by Wickham et al. [46]. or Schaub et al. [41].
Primary prevention of PVR after OGI
A summary of findings of the included RCT for primary prevention of PVR after OGI is presented in Table 4. Guo et al. [36]. demonstrated promising results utilising intravitreal corticosteroids at the time of primary repair of OGI in 34 patients although both reviewers had concerns regarding the masking of surgeons (a common issue when using identifiable intravitreal interventions such as triamcinolone) as well as a high drop-out rate combined with the lack of a sensitivity analysis which undermined the analysis of results from a very heterogenous group of trauma patients [36]. No interventions demonstrated effectiveness without concerns of bias.
Treatment of established PVR
Corticosteroids
A summary of findings of the included RCT for secondary treatment of PVR is presented in Table 5 [53]. A study investigating the efficacy of slow-release 0.7 mg dexamethasone intravitreal implant as a secondary preventative adjunct for PVR grade C treatment found less cystoid macular oedema at 6 months post-op, but no difference in the anatomic or functional success compared to vitrectomy with SiO placement without the dexamethasone implant [28].
Trenado-Luna at al. studied intravitreal dexamethasone implant in 18 patients with grade B or higher PVR, finding greater reattachment rates and better visual acuity in patients treated with dexamethasone implant at the time of vitrectomy, but had several issues concerning the randomisation and masking processes which may have led to the small patient numbers (with significant differences between control and test group demographics) giving a falsely significant result [45].
Antimetabolites and heparin
A combination therapy of steroids or the anti-metabolite 5-FU with LMWH was also studied in 73 patients, which did not reveal any improvement in anatomical or visual outcomes in macular-involving PVR detachments and resulted in worse visual outcomes for patients with macula-sparing PVR retinal detachments [46]. Williams et al. [48]. studied patients with grade C3 or D PVR, finding that intraoperative heparin and dexamethasone in the infusion fluid of 25 patients had no effect on retinal reattachment rate or visual acuity, but was associated with increased rates of post-operative vitreous haemorrhage (20% vs 0%; p = 0.01) and improved (lower) rates of the secondary outcomes of patients requiring retinotomy. Nasr et al. [50]. examined paediatric populations with complex detachment and established PVR, noting slightly improved visual acuity with 5-FU and LMWH but no significant difference in anatomical outcomes. Kumar et al. [40]. studied intraoperative LMWH 15 patients with grade D1-3 PVR, finding improved media clarity (vitreous haze), a subjective grading scale outcome of doubtful clinical significance in a probably unmasked assessor, while demonstrating no significant benefit in objectively measurable outcomes [40].
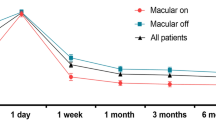
Repeated intravitreal Methotrexate injection was used by Rajan et al. [51] to prevent recurrent RRD in patients with established PVR Grade C, reporting no difference in overall redetachment rate or BCVA, but a significant difference in favour of treatment in the rate of macula on vs macula off detachments under oil. However, RoB reviewers were concerned that anatomical outcomes were assessed by same unmasked assessors who also decided timing of oil removal. Younes et al. [52]. assessed intravitreal infliximab before silicone oil insertion, demonstrating no difference in final anatomical success or single operation success rate 6 months after oil removal, but did find a modest improvement in final BCVA in favour of the intervention group.
The Daunorubicin Study Group investigated the safety and efficacy of daunorubicin, an anthracycline antibiotic that arrests cell proliferation and cell migration, during vitrectomy in 145 eyes with grade C2 or higher PVR. They found that daunorubicin use resulted in a small reduction in the reoperation rate in PVR patients undergoing retinal surgery. There was no difference in visual acuity and reattachment rate at one year [47]. There were some concerns with potential for bias regarding the reoperation rate, as it was unclear how many analyses were performed and limited baseline data were available.
A small RCT utilising prolonged dosing of oral retinoic acid [32] showed positive results in both retinal reattachment rates and visual acuity in 16 patients with primary RRD associated with established PVR.
Discussion
This systematic review found a lack of high-quality evidence to support any one of the wide variety of potential non-surgical interventions aiming to improve the outcomes of patients with OGI or RRD with respect to PVR. To date, 27 RCTs, including 3375 patients, have examined the efficacy and safety of non-surgical primary and secondary interventions for PVR after OGI and RRD, examining a range of interventions, including corticosteroids, anti-metabolites, anti-VEGF, heparin, infliximab, methotrexate, and retinoic acid, without clear benefit compared to control groups. Potentially positive results were reported in two small studies: of intravitreal triamcinolone at the time of primary repair [36], and of oral retinoic acid in secondary treatment of established PVR [32], although these results require confirmation.
The varied and relatively uncommon nature of OGI in post-industrial nations, combined with decentralised ophthalmic trauma services, means that individual surgeons deal with post-OGI PVR rarely and may be unfamiliar with managing primary OGI and subsequent PVR. A relative paucity of cases means that many trauma studies included relatively few patients. In contrast, RRD is common, but the relatively low rate of PVR after RRD (compared to OGI) means that studies of primary prevention must be very large to achieve adequate statistical power. Studies of secondary treatment may require fewer patients, but the challenge facing candidate therapies is to reverse an established disease process, which is potentially more difficult than preventing its occurrence in the first place.
Despite positive results in pre-clinical models, for instance, of corticosteroid treatment and anti-metabolites [54], all therapies have failed to show efficacy in large, well-designed prospective human clinical trials, such as those reported by Wickham et al. [46] or Schaub et al. [41] of 5-FU, or Wiedemann et al. [47] of daunorubicin, or Banerjee et al. [28] and Casswell et al. [31] of corticosteroids.
Corticosteroid therapy has been the most investigated adjunct and remains the most commonly used in clinical practice. Clinical trials evaluating intravitreal triamcinolone acetonide showed a poor efficacy in treating established PVR [25, 55]. A RCT of intravitreal triamcinolone acetonide injection at the time of pars plana vitrectomy with SiO tamponade for secondary treatment in grade C PVR showed no improvement in anatomic success, visual acuity, or PVR development [55]. Triamcinolone acetonide is sometimes employed in retinal detachment repair for vitreous visualisation, but a large prospective multicentre study showed no difference in outcomes between patient undergoing vitrectomy with triamcinolone assisted visualisation and those without (although a confounding factor in this case may be that at the conclusion of vitrectomy there may be minimal amounts of triamcinolone remaining in the vitreous cavity) [25]. A 1-year RCT examining patient outcomes after different vitreoretinal surgeries found that intraoperative use of triamcinolone did not improve visual outcomes in the RRD cohort or reduce the rate of post-operative retinal detachment after vitrectomy [49]. Subconjunctival corticosteroid followed by extended courses of topical corticosteroid is routine after most vitreoretinal surgeries, especially in cases of trauma or cases thought to be high risk for PVR, which may confound the findings of studies and alter the impact of any intervention. There is therefore no evidence that corticosteroid therapy in any form reduces the occurrence of PVR, but it may reduce cystoid macular oedema [28], and is commonly used to manage inflammation.
Guo et al. reported positive findings utilising intravitreal corticosteroids at the time of primary repair (which is distinct from the negative ASCOT findings, where corticosteroids were given at the time of vitrectomy) [31], representing an intervention as early as possible in the PVR development cycle [36]. If these findings could be replicated in larger studies, they may represent a potential, simple, effective intervention. Crucially, post-operative endophthalmitis rates were not increased in patients receiving intravitreal steroids at the time of primary repair, which may be one argument against intravitreal corticosteroids in this cohort. All trials investigating OGI suffer from similar problems of relatively low patient numbers and heterogeneity of injury, which further complicates detailed analysis and comparison [31, 36].
One retrospective study evaluating patients with severe recurrent PVR and tractional retinal detachment or severe intraocular inflammation at high risk for PVR found that these patients had a lower incidence of PVR when treated with intravitreal methotrexate infusion during vitrectomy [56], and Rajan et al. [51]. reported positive subgroup analysis results in a small trial of methotrexate in patients with established PVR. While RoB assessment raised concerns with these studies, the large, multicentre GUARD trial of intravitreal Methotrexate (ADX-2191) is ongoing and results are awaited [57].
A small (n = 35) RCT of oral retinoic acid use in patients with PVR grade C undergoing vitrectomy demonstrated significantly lower rates of retinal re-detachment, macular pucker formation and improved vision in patients being treated with oral retinoic acid [32]. However, a larger prospective cohort study (DELIVER study) found that Isotretinoin may reduce the rate of PVR-related re-detachment in high-risk patients but did not alter the course of disease in patients with established PVR [58]. The positive results of the initial small study do not, therefore, seem to have been replicated. However, some variance between the two studies may warrant a larger investigation to attempt to more closely replicate the original RCT with more patients.
Safety concerns attributable to the intervention were noted in three studies: Wickham et al. [46], who reported worse visual outcomes after 5-FU treatment, and Williams et al. [48], who reported greater rates of post-operative vitreous haemorrhage with heparin treatment. Casswell et al. noted an increased frequency of raised IOP in the corticosteroid group, which is a well-recognised side effect [31].
Limitations of this review include the small number of RCTs included per intervention; for example, only corticosteroids and 5-FU with Heparin had more than two RCTs, although overall, our review included a large number of patients (n = 3255). A greater number of studies of each intervention may be available were non-RCT designs were included, but when RCTs are possible and available, treatment decisions should not be based on non-RCT data. Not all studies that examined interventions in conjunction with vitrectomy specified the extent to which vitrectomy was performed (core vs peripheral vs shave of vitreous base), which may also introduce surgical variation into the comparison of non-surgical interventions.
Conclusion
This review did not identify any evidence of a proven effective non-surgical intervention for the treatment or prophylaxis of PVR. At present, the current techniques of surgical intervention for established PVR remain the only effective option.
Until an effective preventive strategy with minimal adverse effects is identified, the use of potential pharmacological agents for primary prevention of PVR is best targeted at high-risk patients to increase the power of studies to detect an effect. Identification of risk factors for PVR, and detailed assessment, such as utilising the revised Retina Society Classification, is therefore crucial for developing a pharmacologic prophylaxis.
Future investigation may be warranted of intravitreal steroids at the time of primary globe repair of OGI and for prolonged (>8 weeks) oral retinoid administration in patients with established PVR, as both interventions demonstrated potentially positive results in well-designed small studies. There may be benefits to trialling Methotrexate and Infliximab in cases of RRD where PVR has not yet established itself or become severe in order to better assess their efficacy.
References
Pastor JC. Proliferative vitreoretinopathy: an overview. Surv Ophthalmol. 1998;43:3–18.
Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A. The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1983;90:121–5.
Pastor J. Pathogenesis, histopathology, and classification of PVR. In: Retinal detachment surgery and proliferative vitreoretinopathy: from scleral buckling to small-gauge vitrectomy. Cham: Springer; 2023. p. 189–202.
Stryjewski TP, Andreoli CM, Eliott D. Retinal detachment after open globe injury. Ophthalmology. 2014;121:327–33.
Han L, Jia J, Fan Y, Yang L, Yue Z, Zhang W, et al. The Vitrectomy Timing Individualization System for Ocular Trauma (VTISOT). Sci Rep. 2019;9:12612.
Gensheimer WG, Kerber MT, Blanch RJ. The epidemiology and outcomes of combat ocular trauma among local nationals managed at a deployed military hospital in Afghanistan. Eye. 2021;35:2155–63.
Nagasaki H, Shinagawa K, Mochizuki M. Risk factors for proliferative vitreoretinopathy. Prog Retinal Eye Res. 1998;17:77–98.
Pastor JC, de la Rúa ER, Martin F. Proliferative vitreoretinopathy: risk factors and pathobiology. Prog Retinal Eye Res. 2002;21:127–44.
Mudhar HS. A brief review of the histopathology of proliferative vitreoretinopathy (PVR). Eye. 2020;34:246–50.
Wu F, Eliott D. Molecular targets for proliferative vitreoretinopathy. Semin Ophthalmol. 2021;36:218–23.
Chaudhary R, Dretzke J, Scott R, Logan A, Blanch R. Clinical and surgical risk factors in the development of proliferative vitreoretinopathy following retinal detachment surgery: a systematic review protocol. Syst Rev. 2016;5:1–5.
Machemer R, m, Aaberg T, Freeman HM, Alexander RI, John SL, et al. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112:159–65.
Di Lauro S, Kadhim MR, Charteris DG, Pastor JC. Classifications for Proliferative Vitreoretinopathy (PVR): an analysis of their use in publications over the last 15 years. J Ophthalmol. 2016;2016:7807596.
Chaudhary R, Scott RAH, Wallace G, Berry M, Logan A, Blanch RJ. Inflammatory and fibrogenic factors in proliferative vitreoretinopathy development. Transl Vis Sci Technol. 2020;9:23.
Yang S, Li H, Li M, Wang F. Mechanisms of epithelial-mesenchymal transition in proliferative vitreoretinopathy. Discov Med. 2015;20:207–17.
Ricker LJ, Kijlstra A, Kessels AG, De Jager W, Liem AT, Hendrikse F, et al. Interleukin and growth factor levels in subretinal fluid in rhegmatogenous retinal detachment: a case-control study. PLoS ONE. 2011;6:e19141.
Nakao S, Arima M, Ishikawa K, Kohno R, Kawahara S, Miyazaki M, et al. Intravitreal anti-VEGF therapy blocks inflammatory cell infiltration and re-entry into the circulation in retinal angiogenesis. Investig Ophthalmol Vis Sci. 2012;53:4323–8.
Elfenbein A, Simons M. Syndecan-4 signaling at a glance. J Cell Sci. 2013;126:3799–804.
Quiroz-Reyes MA, Quiroz-Gonzalez EA, Quiroz-Gonzalez MA, Lima-Gomez V. Early versus delayed vitrectomy for open globe injuries: a systematic review and meta-analysis. Clin Ophthalmol. 2024;18:1889–1900.
Kuhn F, Schrader W. Prophylactic chorioretinectomy for eye injuries with high proliferative-vitreoretinopathy risk. Clin Anat. 2018;31:28–38.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Glanville J, Kotas E, Featherstone R, Dooley G. Which are the most sensitive search filters to identify randomized controlled trials in MEDLINE? J Med Libr Assoc. 2020;108:556–63.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Ahmadieh H, Feghhi M, Tabatabaei H, Shoeibi N, Ramezani A, Mohebbi MR. Triamcinolone acetonide in silicone-filled eyes as adjunctive treatment for proliferative vitreoretinopathy: a randomized clinical trial. Ophthalmology. 2008;115:1938–43.
Ahmadieh H, Nourinia R, Ragati Haghi A, Ramezani A, Entezari M, Rahmani G, et al. Oral colchicine for prevention of proliferative vitreoretinopathy: a randomized clinical trial. Acta Ophthalmol. 2015;93:e171–2.
Asaria RH, Kon CH, Bunce C, Charteris DG, Wong D, Khaw PT, et al. Adjuvant 5-fluorouracil and heparin prevents proliferative vitreoretinopathy: results from a randomized, double-blind, controlled clinical trial. Ophthalmology. 2001;108:1179–83.
Banerjee PJ, Quartilho A, Bunce C, Xing W, Zvobgo TM, Harris N, et al. Slow-release dexamethasone in proliferative vitreoretinopathy: a prospective, randomized controlled clinical trial. Ophthalmology. 2017;124:757–67.
Banerjee PJ, Xing W, Bunce C, Woodcock M, Chandra A, Scott RA, et al. Triamcinolone during pars plana vitrectomy for open globe trauma: a pilot randomised controlled clinical trial. Br J Ophthalmol. 2016;100:949–55.
Binder S, Bonnet M, Velikay M, Gerard JP, Stolba U, Wedrich A, et al. Radiation therapy in proliferative vitreoretinopathy: a prospective randomized study. Graefe’s Arch Clin Exp Ophthalmol. 1994;232:211–4.
Casswell EJ, Cro S, Cornelius VR, Banerjee PJ, Zvobgo TM, Edwards RT, et al. Randomised controlled trial of adjunctive triamcinolone acetonide in eyes undergoing vitreoretinal surgery following open globe trauma: the ASCOT study. Br J Ophthalmol. 2024;108:440–8.
Chang Y-C, Hu D-N, Wu W-C. Effect of oral 13-cis-retinoic acid treatment on postoperative clinical outcome of eyes with proliferative vitreoretinopathy. Am J Ophthalmol. 2008;146:440–446.e441.
Charteris DG, Aylward GW, Wong D, Groenewald C, Asaria RH, Bunce C, et al. A randomized controlled trial of combined 5-fluorouracil and low-molecular-weight heparin in management of established proliferative vitreoretinopathy. Ophthalmology. 2004;111:2240–5.
Dehghan MH, Ahmadieh H, Soheilian M, Azarmina M, Moradian S, Ramezani AR, et al. Effect of oral prednisolone on visual outcomes and complications after scleral buckling. Eur J Ophthalmol. 2010;20:419–23.
Ganekal S, Dorairaj S. Effect of intraoperative 5-fluorouracil and low molecular weight heparin on the outcome of high-risk proliferative vitreoretinopathy. Saudi J Ophthalmol. 2014;28:257–61.
Guo H, Yu J, He T, Chen S, Sun Z, Zhang J, et al. Early use of intravitreal triamcinolone to inhibit traumatic proliferative vitreoretinopathy: a randomised clinical trial. Br J Ophthalmol. 2024;108:1161–7.
Koerner F, Koerner-Stiefbold U, Garweg JG. Systemic corticosteroids reduce the risk of cellophane membranes after retinal detachment surgery: a prospective randomized placebo-controlled double-blind clinical trial. Graefe’s Arch Clin Exp Ophthalmol. 2012;250:981–7.
Kralinger MT, Stolba U, Velikay M, Egger S, Binder S, Wedrich A, et al. Safety and feasibility of a novel intravitreal tamponade using a silicone oil/acetyl-salicylic acid suspension for proliferative vitreoretinopathy: first results of the Austrian Clinical Multicenter Study. Graefe’s Arch Clin Exp Ophthalmol. 2010;248:1193–8.
Kumar A, Nainiwal S, Choudhary I, Tewari HK, Verma LK. Role of daunorubicin in inhibiting proliferative vitreoretinopathy after retinal detachment surgery. Clin Exp Ophthalmol. 2002;30:348–51.
Kumar A, Nainiwal S, Sreenivas B. Intravitreal low molecular weight heparin in PVR surgery. Indian J Ophthalmol. 2003;51:67–70.
Schaub F, Schiller P, Hoerster R, Kraus D, Holz FG, Guthoff R, et al. Intravitreal 5-fluorouracil and heparin to prevent proliferative vitreoretinopathy: results from a randomized clinical trial. Ophthalmology. 2022;129:1129–41.
Schiff WM, Hwang JC, Ober MD, Olson JL, Dhrami-Gavazi E, Barile GR, et al. Safety and efficacy assessment of chimeric ribozyme to proliferating cell nuclear antigen to prevent recurrence of proliferative vitreoretinopathy. Arch Ophthalmol. 2007;125:1161–7.
Tewari H, Sharma YR, Azad R, Kumar A, Seth M. Topical atropine and timolol therapy in failed retinal detachment surgery. Ophthalmologica. 1994;208:207–9.
Tousi A, Hasanpour H, Soheilian M. Intravitreal injection of bevacizumab in primary vitrectomy to decrease the rate of retinal redetachment: a randomized pilot study. J Ophthalmic Vis Res. 2016;11:271.
Trenado-Luna J, Rivera-Arroyo G, Baqués-Guillén E, Ramos-Roldán C, Arroyo-González JM, García-Chávez L, et al. Transoperative intravitreal dexamethasone implantation in patients with proliferative vitreoretinopathy. Cir Cir. 2023;91:664–71.
Wickham L, Bunce C, Wong D, McGurn D, Charteris D. Randomized controlled trial of combined 5-Fluorouracil and low-molecular-weight heparin in the management of unselected rhegmatogenous retinal detachments undergoing primary vitrectomy. Ophthalmology. 2007;114:698–704.
Wiedemann P, Hilgers R, Bauer P, Heimann K. Group DS. Adjunctive daunorubicin in the treatment of proliferative vitreoretinopathy: results of a multicenter clinical trial. Am J Ophthalmol. 1998;126:550–9.
Williams RG, Chang S, Comaratta MR, Simoni G. Does the presence of heparin and dexamethasone in the vitrectomy infusate reduce reproliferation in proliferative vitreoretinopathy? Graefe’s Arch Clin Exp Ophthalmol. 1996;234:496–503.
Yamakiri K, Sakamoto T, Noda Y, Nakahara M, Ogino N, Kubota T, et al. One-year results of a multicenter controlled clinical trial of triamcinolone in pars plana vitrectomy. Graefe’s Arch Clin Exp Ophthalmol. 2008;246:959–66.
Nasr M, Abdelhadi A, Bessa A, Ibrahim TM. Efficacy of 5-fluorouracil (5-FU) and low molecular weight heparin (LMWH) in high-risk pediatric retinal detachment; randomized clinical trial. BMC Ophthalmol. 2024;24:97.
Rajan RP, Babu KN, Arumugam KK, Muraleedharan S, Ramachandran O, Jena S, et al. Intravitreal methotrexate as an adjuvant in vitrectomy in cases of retinal detachment with proliferative vitreoretinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2024;263:1-5.
Younes AM, Hamza HS, Omar HA, Abdel-Kader AA, Abdelbaki AM, Elnahry AG. Intravitreal infliximab for the treatment of proliferative vitreoretinopathy (FIXER): a randomized controlled phase II trial. Ophthalmol Retin. 2024;8:1044–51.
Nussenblatt R. Uveitis—A Clinical Approach to Diagnosis and Management. Mayo Clin Proc. 1989;64:737–8.
Ferro Desideri L, Artemiev D, Zandi S, Zinkernagel MS, Anguita R. Proliferative vitreoretinopathy: an update on the current and emerging treatment options. Graefes Arch Clin Exp Ophthalmol. 2024;262:679–87.
Munir WM, Pulido JS, Sharma MC, Buerk BM. Intravitreal triamcinolone for treatment of complicated proliferative diabetic retinopathy and proliferative vitreoretinopathy. Can J Ophthalmol. 2005;40:598–604.
Sadaka A, Sisk RA, Osher JM, Toygar O, Duncan MK, Riemann CD. Intravitreal methotrexate infusion for proliferative vitreoretinopathy. Clin Ophthalmol. 2016;54:1811–7.
Aldeyra Therapeutics, Inc, The GUARD Trial — Part 1: A Phase 3 Clinical Trial of Repeated Intravitreal Injections of ADX-2191 Versus Standard-of-Care for Prevention of Proliferative Vitreoretinopathy.: clinicaltrials.gov; 2021.
London NJ, Kaiser RS, Khan MA, Alshareef RA, Khuthaila M, Shahlaee A, et al. Determining the effect of low-dose isotretinoin on proliferative vitreoretinopathy: the DELIVER trial. Br J Ophthalmol. 2019;103:1306–13.
Acknowledgements
External support for this study was provided by the UK Ministry of Defence and BRAVO VICTOR.
Author information
Authors and Affiliations
Contributions
GH performed searches, paper screening, data extraction, risk of bias assessment and wrote the report. RB designed the study, performed paper screening, risk of bias assessment and edited the report. NM performed data extraction and edits. All other named authors contributed via pre-publication review and suggested edits and formed the expert group responsible for initiating and overseeing the study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hunter, G., Maclean, N., Watson, S. et al. Non-surgical interventions for proliferative vitreoretinopathy—a systematic review. Eye 39, 2124–2142 (2025). https://doi.org/10.1038/s41433-025-03846-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03846-7