Abstract
Purpose
To identify the potential biometric associations in patients with early-onset primary angle closure disease (EOPACD), and the relevant biometric cut-offs for distinguishing them.
Design
A prospective cross-sectional observational study.
Participants
The study included 190 eyes with EOPACD of 128 patients, aged 20–40 years (mean age 34.2 ± 6.0 years).
Methods
EOPACD (defined as primary angle closure presenting before 40 years of age) was classified into early-onset primary angle closure suspect (EOPACS), early-onset primary angle closure (EOPAC), and early-onset primary angle closure glaucoma (EOPACG) groups. The participants underwent a baseline clinical examination, including gonioscopy, ultrasound biomicroscopy, anterior segment ocular coherent tomography (ASOCT) and optical biometry (IOL Master). Statistical analysis was performed to identify risk factors associated with EOPACG such as axial length (AL), lens thickness (LT), lens vault (LV), anterior chamber depth (ACD), anterior chamber area (ACA) and other parameters on ASOCT.
Main outcome measures
To identify ocular biometric associations and potential cut-offs for distinguishing glaucoma eyes from suspects.
Results
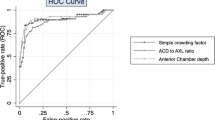
Biometric measurements showed that the AL was the shortest, while ACD, ACA and ASOCT angle parameters were narrowest in eyes with EOPACG, as compared to EOPACS and EOPAC (p < 0.001; Bonferroni/Dunn test). Similarly, LV and LT were highest in eyes with EOPACG (p < 0.001). Logistic regression analysis revealed that ACD exhibited the highest predictive ability (ACD ≤ 2.73 mm, OR 4.36, AUC 0.72), followed by LT (LT ≥ 4.22 mm, OR 4.2, AUC 0.71) and ACA (ACA ≤ 17.24mm2, OR 3.04, AUC 0.7) for EOPACG.
Conclusions
This study highlights the significance of ocular biometric measurements, especially ACD and LT, which can assist in stratifying individuals with EOPACD for early detection of glaucoma. Thickening of the lens with the resultant crowded anterior chamber seemed to be the most prevalent biometric characteristic in eyes with frank glaucoma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All the dataset generated in this study is available with the corresponding author (SG) on request.
References
Bourne RRA, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1:e339–49.
Zhang N, Wang J, Chen B, Li Y, Jiang B. Prevalence of primary angle closure glaucoma in the last 20 years: a meta-analysis and systematic review. Front Med. 2020;7:624179.
Zhang X, Guo PY, Lin C, Li F, Nguyen A, Sakata R, et al. Assessment of iris trabecular contact in eyes with gonioscopic angle-closure. Ophthalmology. 2023;130:111–9.
Appleby RS, Kinder RSL. Bilateral angle-closure glaucoma in a 14-year-old boy. Arch Ophthalmol. 1971;86:449–50.
Badlani VK, Quinones R, Wilensky JT, Hawkins A, Edward DP. Angle-closure glaucoma in teenagers. J Glaucoma. 2003;12:198–203.
Brosnan JD. Primary chronic angle-closure glaucoma in a young woman of 19 years-case repot. Trans Ophthalmol Soc NZ. 1973;25:130–2.
Sharma S. Bilateral angle closure glaucoma in a teenage girl. Paripex Indian J Res. 202;15;16–7.
Alzuhairy S. Bilateral angle closure glaucoma in a teenage girl - a rare presentation in Arab population - a case report. Int J Health Sci. 2019;13:56–8.
Gao F, Wang J, Chen J, Wang X, Chen Y, Sun X. Etiologies and clinical characteristics of young patients with angle-closure glaucoma: a 15-year single-center retrospective study. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2021;259:2379–87.
Ritch R, Chang BM, Liebmann JM. Angle closure in younger patients. Ophthalmology. 2003;110:1880–9.
Xu Y, Tan Q, Li C, Liu D. The ocular biometry characteristics of young patients with primary angle-closure glaucoma. BMC Ophthalmol. 2022;22:150.
Xu BY, Friedman DS, Foster PJ, Jiang Y, Porporato N, Pardeshi AA, et al. Ocular biometric risk factors for progression of primary angle closure disease: the Zhongshan angle closure prevention trial. Ophthalmology. 2022;129:267–75.
Chen YY, Chen YY, Sheu SJ, Chou P. The biometric study in different stages of primary angle-closure glaucoma. Eye Lond Engl. 2013;27:1070–6.
Luo Q, Xue W, Yuan Y, Fu C, He J, Zou H, et al. Peripheral anterior chamber depth and screening techniques for primary angle closure disease in community elderly Chinese. BMC Ophthalmol. 2020;20:353.
Zhou S, Pardeshi AA, Burkemper B, Apolo G, Cho A, Jiang X, et al. Refractive error and anterior chamber depth as risk factors in primary angle closure disease: the Chinese American eye study. J Glaucoma. 2023;32:257–64.
Zhang Y, Thomas R, Zhang Q, Li SZ, Wang NL. Progression of primary angle closure suspect to primary angle closure and associated risk factors: the Handan eye study. Invest Ophthalmol Vis Sci. 2021;62:2.
Razeghinejad MR, Banifatemi M. Ocular biometry in angle closure. J Ophthalmic Vis Res. 2013;8:17–24.
Sihota R, Lakshmaiah NC, Agarwal HC, Pandey RM, Titiyal JS. Ocular parameters in the subgroups of angle closure glaucoma. Clin Exp Ophthalmol. 2000;28:253–8.
Moghimi S, Vahedian Z, Zandvakil N, Mohammdi M, Fakhraie G, Nassiri N, et al. Role of lens vault in subtypes of angle closure in Iranian subjects. Eye. 2014;28:337–43.
Wu RY, Nongpiur ME, He MG, Sakata LM, Friedman DS, Chan YH, et al. Association of narrow angles with anterior chamber area and volume measured with anterior-segment optical coherence tomography. Arch Ophthalmol Chic Ill 1960. 2011;129:569–74.
Jiang Y, Wang D, Wang W, Chen F, Wang L, Scheetz J, et al. Five-year changes in anterior segment parameters in an older population in urban southern China: the Liwan Eye Study. Br J Ophthalmol. 2020;104:582–7.
Baskaran M, Iyer JV, Narayanaswamy AK, He Y, Sakata LM, Wu R, et al. Anterior segment imaging predicts incident gonioscopic angle closure. Ophthalmology. 2015;122:2380–4.
Nongpiur ME, Aboobakar IF, Baskaran M, Narayanaswamy A, Sakata LM, Wu R, et al. Association of baseline anterior segment parameters with the development of incident gonioscopic angle closure. JAMA Ophthalmol. 2017;135:252.
Markowitz SN, Donald Morin J. The ratio of lens thickness to axial length for biometric standardization in angle-closure glaucoma. Am J Ophthalmol. 1985;99:400–2.
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–42.
Hodapp EP, Parrish RK, Anderson DR. Clinical decisions in glaucoma. Mosby. 1993.
Kumar G, Bali SJ, Panda A, Sobti A, Dada T. Prevalence of plateau iris configuration in primary angle closure glaucoma using ultrasound biomicroscopy in the Indian population. Indian J Ophthalmol. 2012;60:175–8.
Habibzadeh F, Habibzadeh P, Yadollahie M. On determining the most appropriate test cut-off value: the case of tests with continuous results. Biochem Medica. 2016;26:297–307.
Zhang XL, Li A, Teng LL, Du SL, Zhu YY, Ge J. Primary chronic angle-closure glaucoma in younger patients. Int J Ophthalmol. 2007;7:613–7.
Kocak I, Altintas AG, Yalvac IS, Nurozler A, Kasim R, Duman S. Treatment of glaucoma in young nanophthalmic patients. Int Ophthalmol. 1997;20:107–11.
Sun JH, Sung KR, Yun SC, Cheon MH, Tchah HW, Kim MJ, et al. Factors associated with anterior chamber narrowing with age: an optical coherence tomography study. Investig Opthalmol Vis Sci. 2012;53:2607.
Shabana N, Aquino MC, See J, Ce Z, Tan AM, Nolan WP, et al. Quantitative evaluation of anterior chamber parameters using anterior segment optical coherence tomography in primary angle closure mechanisms. Clin Exp Ophthalmol. 2012;40:792–801.
Yadav SK, Panigrahi A, Gupta D, Gupta S, Gupta V. Potential utility of anterior segment optical coherence tomography and biometry in differentiating plateau iris configuration from pupillary block. Clin Exp Optom. 2024;1–7. https://doi.org/10.1080/08164622.2024.2428304.
Aung T. Anterior chamber depth and the risk of primary angle closure in 2 East Asian Populations. Arch Ophthalmol. 2005;123:527.
Alsbirk PH. Anterior chamber depth and primary angle-closure glaucoma: I. An epidemiologic study in Greenland Eskimos. Acta Ophthalmol. 1975;53:89–104.
Congdon NG, Quigley HA, Hung PT, Wang TH, Ho TC. Screening techniques for angle-closure glaucoma in rural Taiwan. Acta Ophthalmol Scand. 1996;74:113–9.
Devereux JG. Anterior chamber depth measurement as a screening tool for primary angle-closure glaucoma in an East Asian Population. Arch Ophthalmol. 2000;118:257.
Nongpiur ME, Sakata LM, Friedman DS, He M, Chan YH, Lavanya R, et al. Novel association of smaller anterior chamber width with angle closure in Singaporeans. Ophthalmology. 2010;117:1967–73.
Marchini G, Pagliarusco A, Toscano A, Tosi R, Brunelli C, Bonomi L. Ultrasound biomicroscopic and conventional ultrasonographic study of ocular dimensions in primary angle-closure glaucoma. Ophthalmology. 1998;105:2091–8.
Thomas R, George R, Parikh R, Muliyil J, Jacob A. Five year risk of progression of primary angle closure suspects to primary angle closure: a population based study. Br J Ophthalmol. 2003;87:450–4.
George R, Paul PG, Baskaran M, Ramesh SV, Raju P, Arvind H, et al. Ocular biometry in occludable angles and angle closure glaucoma: a population based survey. Br J Ophthalmol. 2003;87:399–402.
Nongpiur ME, He M, Amerasinghe N, Friedman DS, Tay WT, Baskaran M, et al. Lens vault, thickness, and position in Chinese subjects with angle closure. Ophthalmology. 2011;118:474–9.
Ozaki M, Nongpiur ME, Aung T, He M, Mizoguchi T. Increased lens vault as a risk factor for angle closure: confirmation in a Japanese population. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2012;250:1863–8.
Kim YK, Yoo BW, Kim HC, Aung T, Park KH. Relative lens vault in subjects with angle closure. BMC Ophthalmol. 2014;14:93.
Lowe RF. Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol. 1970;54:161–9.
Lan YW, Hsieh JW, Hung PT. Ocular biometry in acute and chronic angle-closure glaucoma. Ophthalmol J Int Ophtalmol Int J Ophthalmol Z Augenheilkd. 2007;221:388–94.
Moghimi S, Ramezani F, He M, Coleman AL, Lin SC. Comparison of anterior segment-optical coherence tomography parameters in phacomorphic angle closure and acute angle closure eyes. Invest Ophthalmol Vis Sci. 2015;56:7611–7. Dec.
Chakrabarti K, Samant S, Mohapatra R, Mishra S, Das S, Chakrabarti M. A comparison of lens parameters in patients with various subtypes of primary angle-closure disease and the normal population: a prospective study. Indian J Ophthalmol. 2022;70:2889.
Li M, Chen Y, Jiang Z, Chen X, Chen J, Sun X. What are the characteristics of primary angle closure with longer axial length?. Investig Opthalmol Vis Sci. 2018;59:1354.
Sherpa D, Badhu B. Association between axial length of the eye and primary angle closure glaucoma. Kathmandu Univ Med J. 1970;6:361–3.
Van Romunde SHM, Thepass G, Lemij HG. Is hyperopia an important risk factor for PACG in the Dutch population? A case control study. J Ophthalmol. 2013;2013:1–6.
Sihota R, Ghate D, Mohan S, Gupta V, Pandey RM, Dada T. Study of biometric parameters in family members of primary angle closure glaucoma patients. Eye. 2008;22:521–7.
Wang D, Huang W, Li Y, Zheng Y, Foster PJ, Congdon N, et al. Intraocular pressure, central corneal thickness, and glaucoma in Chinese adults: the Liwan eye study. Am J Ophthalmol. 2011;152:454–62.e1.
Pang CE, Lee KY, Su DH, Htoon HM, Ng JY, Kumar RS, et al. Central corneal thickness in chinese subjects with primary angle closure glaucoma. J Glaucoma. 2011;20:401–4.
Author information
Authors and Affiliations
Contributions
SG, SY, VG had substantial contribution to the conception and design of the study. SG, SY, AP, SS, TV, AKP, SoS, and RS had substantial contribution to the acquisition and collection of data. SG, SY and AP contributed to the analysis and interpretation of data. SG, SY, and AP contributed to the drafting of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, S., Yadav, S.K., Panigrahi, A. et al. Risk factor stratification in early-onset primary angle closure disease. Eye 39, 2604–2611 (2025). https://doi.org/10.1038/s41433-025-03884-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03884-1