Abstract
Aims
To investigate the ocular symptoms and characteristics exhibited by extranodal NK/T-cell lymphoma (ENKTL) patients.
Methods
One hundred sixty-eight patients with mature T/Natural Killer-cell Lymphoma (MTNKL) were recruited in this study, among whom 107 cases were ENKTL patients. A retrospective analysis was conducted on 12 of these ENKTL patients who had ocular symptoms. Results of ophthalmic and systemic auxiliary examinations, disease progression, and prognosis were documented.
Results
Ocular symptoms occurred in bilateral eyes (n = 4) and unilateral eyes (n = 8). The average interval from the diagnosis of ENKTL to the onset of ocular symptoms was 18.1 (±20.8) months. According to the ocular symptoms and auxiliary examinations, eight patients had ocular adnexal symptoms only, and four patients had intraocular symptoms only. All patients exhibited impaired vision. After receiving combined treatment with systemic chemotherapy, radiotherapy, and local ocular therapy, six patients died during the follow-up, and the median survival time from diagnosis was 17 (range: 2–45) months. Among the surviving six patients, five out of seven eyes had poor visual prognoses lower than hand motion (HM), while two maintained a visual acuity of 20/25.
Conclusion
In this study, the ocular presentations can be easily confounded with conditions such as uveitis or orbital cellulitis, necessitating vigilant clinical differentiation. To date, the visual prognoses of ENKTL patients with ocular symptoms remain regrettably poor.
Similar content being viewed by others
Background
Mature T-cell and NK-cell lymphoma (MTNKL) is a group of rare, heterogeneous, and high-mortality malignancies, comprising over 20 distinct disease entities according to the WHO classification system [1, 2]. Extranodal NK/T-cell lymphoma (ENKTL) is the most common subtype [3], which accounts for approximately 2.9% and 13.7% of the non-Hodgkin lymphoma cases in the United States and Northwest China, respectively [4, 5]. While the incidence of most ENKTL tends to rise with age and they frequently result in unfavourable clinical outcomes, survival rates have improved with new therapeutic approaches.
ENKTL can have devastating consequences for the ocular adnexa and eye. The nasal cavity, paranasal sinuses and nasopharynx are most commonly involved initially in ENKTL patients [6], while patients with orbital involvement are relatively rare [7]. Notably, most ocular manifestations are secondary, with primary intraocular lymphoma being less commonly reported [8, 9]. The low incidence of ocular involvement in ENKTL makes it difficult to comprehensively analyse its prevalence, progression, and prognosis. As such, our study aims to assess the characteristics and outcomes of patients with ENKTL who exhibit ocular manifestations.
Methods
Participants
Patients diagnosed with MTNKL between April 2019 and April 2022 at Xinhua Hospital were identified via the patient registry. The case inclusion criteria included: (1) a pathologically confirmed MTNKL diagnosis according to the WHO classification and (2) proven subtype classification. Diagnostic procedures included pathological biopsy and immunohistochemical staining. If required, in situ stains for Epstein–Barr virus (EBV)-encoded small RNA (EBER) and T-cell receptor gene rearrangement were detected using PCR. The diagnostic and classification criteria adhered to the latest WHO classification for tumours of hematopoietic and lymphoid tissues [1]. Positron emission tomography-computed tomography (PET-CT) and orbital magnetic resonance imaging (MRI) were used to monitor general and ocular metastasis. Comprehensive ophthalmic examinations for ocular manifestations included assessments of best-corrected visual acuity (BCVA), intraocular pressure, B-scan ultrasound, ultrasound biomicroscopy, Optos 200Tx and optical coherence tomography. The study was approved by the Ethics Committee of Xinhua Hospital, and informed consent was obtained from all participants.
Treatment
The initial systemic therapeutic modalities for tumours varied widely, as a portion of the study cohort had received treatment at other institutions prior to referral. All patients received conventional chemotherapy, and early-stage patients with localised lesions received a combination of radiotherapy and chemotherapy. For patients presenting with ocular symptoms, treatment was tailored based on the specific local manifestations:
-
Orbital infiltration cases: both systemic and local steroids were utilised for their anti-inflammatory effects. Patients with orbital mass received a systemic chemotherapy regimen, some also combined with radiotherapy, and when necessary, resection surgery was performed.
-
Intraocular involvement cases: for manifestations like vitreous opacity, vitreous haemorrhage, or retinal detachment, interventions such as diagnostic vitrectomy and vitreous tap were recommended. If intraocular tumour metastasis was identified, intravitreal injections of methotrexate (400 μg/0.1 ml) were administered if accessible.
Statistical analysis
Patients’ clinical data, including demographic information, clinical symptoms, ophthalmic findings, treatment modalities and outcomes, were recorded and summarised using descriptive statistics. Quantitative data were presented as median, and categorical data were expressed in terms of absolute and relative frequencies. All statistical analyses were conducted using SAS (version 9.4), and a p value < 0.05 was considered statistically significant.
Results
Patient characteristics
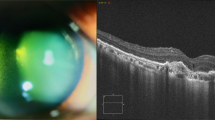
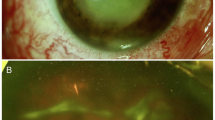
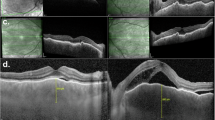
This study included a total of 168 patients with MTNKL, among whom 107 were ENKTL patients (Fig. S1). The median age of ENKTL patients was 46 (range: 11–84) years, and the male–female ratio was 1.82. The pathology for 14 patients with ocular symptoms was ENKTL (12 cases) and peripheral T-cell lymphoma, not otherwise specified (2 cases). Among these 12 ENKTL patients, 10 were male and 2 were female, resulting in a male-to-female ratio of 5. The median age for this group was 47 (range: 25–74) years. Demographic information and clinical characteristics such as age, gender, lymphoma subtype, initial tumour location, systemic involvement, treatment modalities and outcomes of ENKTL patients were recorded (Table 1). All ENKTL patients presented with nasal involvement, with 80% exhibiting the nasal cavity as the primary site, while one case manifested initial orbital symptoms. Among the 12 patients, 8 cases had unilateral eye involvement, with 3 cases affecting the right eye and 5 cases affecting the left eye; the remaining 4 patients had bilateral eye involvement. The average duration from ENKTL diagnosis to the onset of ocular symptoms was 18.1 (±20.8) months. Comprehensive systemic and ophthalmic examinations, including orbital or intraocular tissue biopsies, cranial and orbital MRI, PET/CT, and fundus examinations, classified patients into distinct categories, including ocular adnexal manifestations only (8, 66.7%) and intraocular manifestations only (4, 33.3%) (Figs. 1 and 2). Among the 16 eyes of the 12 patients studied, vision impairment was universally observed. Common signs for patients with orbital infiltration included orbital swelling, diplopia, ptosis, and either abduction or infraduction deficits. Patients with intraocular metastases exhibited clinical findings including keratic precipitates, vitreous opacity, vitreous haemorrhage, and subretinal yellowish-white tumour nodules. Detailed information is summarised in Table 2.
A–C Orbital MRI: A poorly demarcated mass lesion is demonstrated in the left orbit involving the eyelids and periorbital tissues. The lesion exhibits an isointense signal on T1-weighted imaging and a hypointense signal on T2-weighted imaging, with marked contrast enhancement. The mass encases the globe with ill-defined margins between the lesion and both the optic nerve and extraocular muscles. D PET-CT: the left periorbital region shows patchy soft tissue density with mildly increased FDG uptake. The boundaries between the left extraocular muscles, optic nerve and surrounding soft tissues are indistinct. The orbital fat planes are obscured.
A, B Initial presentation: Ophthalmic examination revealed vitreous haze in the left eye, predominantly in the peripheral vitreous. The fundus showed a flat retina with a normal cup-to-disc ratio. Anterior segment photography demonstrated subtle corneal oedema and fine stellate keratic precipitates distributed diffusely over the inferior cornea. Tyndall (+), and no other remarkable abnormalities were noted. C Post-operation presentation: The vitreous cavity appeared clear following diagnostic pars plana vitrectomy, with flat retina and no detectable pathological changes. D Vitreous pathological analysis: Histopathological examination of the vitreous specimen by haematoxylin and eosin staining revealed scattered lymphoid cells without significant atypia, accompanied by occasional hyalocytes. The specimen contained sparse histiocytes with necrotic debris. E Disease progression: the patient failed to adhere to the recommended treatment regimen (intravitreal methotrexate injections), resulting in intraocular lymphoma recurrence characterised by recurrent vitreous opacities with multiple subretinal yellowish-white tumour nodules of varying sizes and shapes in the peripheral retina. F Therapeutic response: The intraocular metastatic lesions showed significant regression following multiple intravitreal methotrexate injections.
Treatment and prognosis
All 12 patients received systemic chemotherapy treatment, and five patients received concurrent radiotherapy. Due to their refractory disease status, therapeutic strategies employed in this study consisted of asparaginase-based regimens and programmed cell death-1 (PD-1) inhibitor-based regimens with multiple chemotherapeutic agents (Table 1). Four patients did not receive topical treatment, among whom one patient had only mild ocular symptoms, and three patients had poor general health. One patient underwent orbital mass resection. Diagnostic vitrectomy and intraocular injection of methotrexate were performed in two patients with vitreous opacity and suspected intraocular tumour. Patients with ocular inflammation and high intraocular pressure were given symptomatic treatments. During a mean follow-up period of 23.5 (2–45) months, nine patients relapsed and six patients died of hemophagocytic syndrome or haemorrhagic shock. The mortality rate was as high as 50%. The mean survival time was 17 (2–45) months. For the seven eyes of the six surviving patients, only two eyes retained a BCVA of 20/25, while the rest (4 eyes) reported a BCVA lower than HM. The treatment and prognosis of ENKTL patients with ocular involvement were recorded in Table 3.
Discussion
In this study, we describe our experience in the diagnosis and treatment of ocular manifestations of ENKTL. We report an 8.3% incidence of ocular symptoms in 168 MTNKL patients, and the most common subtype was ENKTL (63.7%). The distribution was consistent with the dominant subtype of ENKTL in the Asian population in the literature [10]. For ENKTL patients, the median age for the 107 patients was 46 years, and was 47 years for the 12 patients with ocular symptoms. This is comparable to the median age of 41 years from a prior study [5], suggesting that ENKTL occurs predominantly in middle-aged adults. The male–female ratio of patients with ocular symptoms was 5:1, consistent with previous data showing an increased susceptibility to ocular manifestations in males [11].
Ocular manifestations in ENKTL predominantly involve the orbit as secondary lesions, mainly due to the direct invasion of adjacent structures in ENKTL [12], though orbital involvement may occasionally serve as the initial presentation [13, 14]. This study included one case that was presented with orbital swelling and visual impairment and had initially been misdiagnosed as cellulitis. This condition may delay correct diagnosis and treatment. Previous studies have reported two different types of ocular involvement in patients with nasal T/NK lymphoma, namely uveitis or vitritis and orbital infiltration [15]. Therefore, we support the recommendation that if the lymphoma does not respond to conventional therapy like steroids and antibiotics, timely use of orbital MRI and CT and biopsy is paramount [7].
ENKTL is a highly invasive and aggressive disease, with patients unfortunately facing poor prognoses and short survival times. ENKTL remains predominantly found in Asian and Latin American populations [16], intriguingly correlated to the geographic distribution of EBV subtype infections. In our study, all patients tested positive for EBV. The correlation between EBV infection and the progression of lymphoma is noteworthy and suggests varying stages of EBV ocular involvement, a hypothesis requiring further validation. Previous studies have shown that EBV-DNA copy number was associated with treatment response and disease prognosis in ENKTL [17, 18], and EBV-infected NK cells might further transform into malignant lymphoma [19]. Studies on the possible molecular pathogenesis of ENKTL have inferred that chronic active EBV infection may be the initial manifestation of EBV infection of NK cells, which progress to ENKTL when accompanied by additional genomic alterations from deficiencies in tumour suppressor genes and the constitutive activation of specific growth or transcription factors [20]. Given that EBV infection contributes to lymphoma progression, we posit that chronic active EBV infection, EBV-positive T-cell, NK-cell lymphoproliferative diseases, and NK/T-cell intraocular lymphoma metastasis may represent different stages of EBV involvement in the eye, for which further investigation is required.
Currently, combined chemotherapy and radiotherapy remain the most common therapeutic regimens for ENKTL patients [21, 22]. In most circumstances, timely systemic treatment is crucial, and local therapy is recommended as an adjunct, though efficacious treatments for ocular involvement are sparse [23]. Standard protocol calls for the surgical removal of tumours confined to the orbit. Diagnostic pars plana vitrectomies are generally recommended for cases of unexplained vitreous opacities or haemorrhage, and intravitreal methotrexate injection has been used for palliative and conservative vision-restoring measures [24]. All patients in this study received multi-agent chemotherapy regimens based on asparaginase or PD-1 inhibitors, and five of them received additional radiotherapy. Even though treatments had been administered accordingly, MTNKL patients with ocular manifestations exhibited significantly higher mortality (50%) compared to the overall MTNKL cohort mortality (27.4%) in this study, suggesting more aggressive disease biology in this subgroup. The median survival time from ENKTL diagnosis was 17 (range: 2–45) months, compared to the previously reported 21.7 (range: 2–69) months in patients with T-cell intraocular lymphoma [9], which aligns with the low survival rate observed in prior studies of ENKTL patients with concurrent ocular symptoms [14, 25, 26].
This study bears several limitations, including its retrospective nature, sample size for ENKTL with ocular involvement, and a homogenous population that may limit its generalisability, despite clinical features of the disease being generally similar [27]. Notably, MTNKL occurred less frequently than B-cell lymphomas in the cohort, resulting in a small sample size. Further, the mean follow-up time was 23.5 months, during which six patients died, making it difficult to investigate whether ocular involvement is an independent factor for the endpoint outcome of ENKTL patients. Lastly, tertiary referral bias may misrepresent the true incidence and nature of disease progression.
Conclusions
In conclusion, ENKTL with ocular manifestation is a rare condition, but attention should be paid to differentiate it from other ocular diseases based on the prevalence of confounded diagnoses noted in this study. While general prognoses have improved due to aggressive regimens and novel therapies, the mortality rate of ENKTL and the vision-threatening nature of ocular involvement remain high and burdensome. We recommend future studies on the epidemiology and clinical outcomes for ENKTL patients with ocular symptoms and hope this study will enhance future discussions and collaborations with the lymphoma and ophthalmologic communities.
Summary
What was known before
-
Extranodal NK-cell lymphoma is a rare and aggressive malignancy with a tendency to invade and involve adjacent tissues.
-
Symptoms in most patients with extranodal NK-cell lymphoma are limited to the orbit.
What this study adds
-
Both the visual prognosis and the overall prognosis of extranodal NK-cell lymphoma patients with ocular symptoms were poor.
-
With the increasing survival rates due to new therapeutic avenues, patients with extranodal NK-cell lymphoma need to be suspected for the presence of ocular involvement, including orbital infiltration and intraocular involvement.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Naresh KN, Medeiros LJ. Introduction to the fifth edition of the World Health Organization classification of tumors of hematopoietic and lymphoid tissues. Mod Pathol. 2023;36:100330.
Attygalle AD, Chan JKC, Coupland SE, Du MQ, Ferry JA, de Jong D, et al. What is new in the 5th edition of the World Health Organization classification of mature B and T/NK cell tumors and stromal neoplasms? J Hematop. 2024;17:71–89.
Sánchez-Romero C, Bologna-Molina R, Paes de Almeida O, Santos-Silva AR, Prado-Ribeiro AC, Brandão TB, et al. Extranodal NK/T cell lymphoma, nasal type: an updated overview. Crit Rev Oncol Hematol. 2021;159:103237.
Laurini JA, Perry AM, Boilesen E, Diebold J, Maclennan KA, Müller-Hermelink HK, et al. Classification of non-Hodgkin lymphoma in Central and South America: a review of 1028 cases. Blood. 2012;120:4795–801.
Cao C, Feng J, Gu H, Tang H, Xu L, Dong H, et al. Distribution of lymphoid neoplasms in Northwest China: analysis of 3244 cases according to WHO classification in a single institution. Ann Diagn Pathol. 2018;34:60–5.
Tse E, Zhao W-L, Xiong J, Kwong Y-L. How we treat NK/T-cell lymphomas. J Hematol Oncol. 2022;15:74.
Dai W, Zhong M, Shen W, Zou K, Bai CG. Natural killer T-cell lymphoma originating from the orbit. Chin Med J. 2012;125:1677–80.
Tagawa Y, Namba K, Ogasawara R, Kanno H, Ishida S. A case of mature natural killer-cell neoplasm manifesting multiple choroidal lesions: primary intraocular natural killer-cell lymphoma. Case Rep Ophthalmol. 2015;6:380–4.
Chaput F, Amer R, Baglivo E, Touitou V, Kozyreff A, Bron D, et al. Intraocular T-cell Lymphoma: clinical Presentation, Diagnosis, Treatment, and Outcome. Ocul Immunol Inflamm. 2017;25:639–48.
Yoon SE, Song Y, Kim SJ, Yoon DH, Chen TY, Koh Y, et al. Comprehensive analysis of peripheral T-cell and natural killer/T-cell lymphoma in Asian patients: a multinational, multicenter, prospective registry study in Asia. Lancet Reg Health West Pac. 2021;10:100126.
Hu ZZ, Wang Y. The factors associated with the early diagnosis of nasal NK/T-cell lymphoma with prominent ocular symptoms and general nasal NKTL. Am J Otolaryngol. 2019;40:353–7.
Lee GI, Kim YD, Young SM, Shin S, Woo KI. Clinical characteristics and treatment outcomes of natural killer/T-cell lymphoma involving the ocular adnexa. Br J Ophthalmol. 2019;103:269–73.
Marchino T, Ibáñez N, Prieto S, Novelli S, Szafranska J, Mozos A, et al. An aggressive primary orbital natural killer/T-cell lymphoma case: poor response to chemotherapy. Ophthalmic Plast Reconstr Surg. 2014;30:e131–4.
Ely A, Evans J, Sundstrom JM, Malysz J, Specht CS, Wilkinson M. Orbital involvement in extranodal natural killer T cell lymphoma: an atypical case presentation and review of the literature. Orbit. 2012;31:267–9.
Hon C, Kwok AK, Shek TW, Chim JC, Au WY. Vision-threatening complications of nasal T/NK lymphoma. Am J Ophthalmol. 2002;134:406–10.
Xiong J, Zhao W-L. Advances in multiple omics of natural-killer/T cell lymphoma. J Hematol Oncol. 2018;11:134.
Ito Y, Kimura H, Maeda Y, Hashimoto C, Ishida F, Izutsu K, et al. Pretreatment EBV-DNA copy number is predictive of response and toxicities to SMILE chemotherapy for extranodal NK/T-cell lymphoma, nasal type. Clin Cancer Res. 2012;18:4183–90.
Kanakry JA, Li H, Gellert LL, Lemas MV, Hsieh WS, Hong F, et al. Plasma Epstein-Barr virus DNA predicts outcome in advanced Hodgkin lymphoma: correlative analysis from a large North American cooperative group trial. Blood. 2013;121:3547–53.
Zhang Y, Nagata H, Ikeuchi T, Mukai H, Oyoshi MK, Demachi A, et al. Common cytological and cytogenetic features of Epstein-Barr virus (EBV)-positive natural killer (NK) cells and cell lines derived from patients with nasal T/NK-cell lymphomas, chronic active EBV infection and hydroa vacciniforme-like eruptions. Br J Haematol. 2003;121:805–14.
Sun KM, Wong YH, Cheung KC, Yuen CM, Chan YT, Lai WJ, et al. Update on molecular diagnosis in extranodal NK/T-cell lymphoma and its role in the era of personalized medicine. Diagnostics. 2022;12:409.
Flower A, Xavier AC, Cairo MS. Mature (non-anaplastic, non-cutaneous) T-/NK-cell lymphomas in children, adolescents and young adults: state of the science. Br J Haematol. 2019;185:418–35.
de Pádua Covas Lage LA, Machado PPF, Reichert CO, Miranda E, Culler HF, da Siqueira SAC, et al. High-dose extended-field radiotherapy plus chemotherapy improved survival in extranodal NK/T-cell lymphoma in a real-life setting: results from the multicenter T-Cell Brazil Project. Sci Rep. 2022;12:20557.
Kecik M, Prod’hom S, Giannotti F, Thumann G, Malclès A. Simultaneous intraocular and orbital involvement of NK/T-cell lymphoma. J Fr Ophtalmol. 2021;44:e595–6.
Wickremasinghe SS, Ojaimi E, Lim L, Stawell R, McKelvie P, Zamir E. Intravitreal methotrexate as adjunctive, palliative therapy in intraocular T-cell lymphoma. Ocul Immunol Inflamm. 2010;18:184–6.
Thompson AC, McCall CM, Proia AD. Beneath the retinal pigment epithelium: histopathologic findings in metastatic extranodal natural killer/T-cell lymphoma, nasal type. Ocul Oncol Pathol. 2018;4:388–94.
Coupland SE, Foss HD, Assaf C, Auw-Haedrich C, Anastassiou G, Anagnostopoulos I, et al. T-cell and T/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: a clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology. 1999;106:2109–20.
Fox CP, Ahearne MJ, Pettengell R, Dearden C, El-Sharkawi D, Kassam S, et al. Guidelines for the management of mature T- and natural killer-cell lymphomas (excluding cutaneous T-cell lymphoma): a British Society for Haematology Guideline. Br J Haematol. 2022;196:507–22.
Acknowledgements
The authors would like to thank all the patients and their families for their participation.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 81770963, 81770964); Open Project of Sichuan Provincial Key Laboratory for Human Disease Gene Study.
Author information
Authors and Affiliations
Contributions
Luo J and TR wrote the main manuscript text. TR, FP and ZPQ collected patients’ data. Luo J, LCX and MYJ analysed the data. Li J and GVY prepared figures and tables. FP and ZPQ funded this study. All authors reviewed the manuscript and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine (Approval No. XHEC-D-2024-112), and consent was obtained from all patients prior to participation in the study. All procedures were conducted in accordance with the principles outlined in the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, J., Tao, R., Liu, Cx. et al. Ocular manifestations of patients with extranodal NK/T-cell lymphoma. Eye 39, 3243–3248 (2025). https://doi.org/10.1038/s41433-025-04052-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04052-1