Abstract
The present study aimed to determine the relationship between cataract subtypes and circadian blood pressure (BP) variability in elderly individuals. In this cross-sectional study of a community-based cohort, we assessed bilateral lens opacity using slit lamp photographs of 458 elderly individuals (mean age, 69.1 years). Cataract status was defined as a bilateral Lens Opacities Classification System III grade of ≥3 for nuclear cataract, ≥2 for cortical cataract, and ≥2 for posterior subcapsular cataract (PSC). Ambulatory BP monitoring was performed at 30-min intervals for 48 h. A nondipper pattern of BP was defined as a <10% decline in the mean nighttime systolic BP relative to the mean daytime systolic BP. The prevalence of nondipper patterns was 42.4% and 25.9% in the groups with nuclear cataracts (n = 66) and without cataracts for both eyes (n = 290), respectively. Multivariable logistic regression analysis adjusted for potential confounders revealed a significantly higher odds ratio (OR) for nondipper pattern in the group with nuclear cataract than in that without cataract (OR, 1.81; 95% confidence interval, 1.01–3.24; P = 0.047) but not in the group with cortical cataract (P = 0.61) or PSC (P = 0.95). In conclusion, circadian BP variability was significantly diminished in elderly individuals with nuclear cataracts but not in those with cortical cataracts or PSCs. These associations were independent of daytime light exposure, physical activity, and known risk factors of cataracts, such as aging, obesity, and diabetes.
Similar content being viewed by others
Introduction
Blood pressure (BP) displays a peak during daytime and a trough during nighttime [1]. This circadian BP variability depends on the human circadian timing system of the suprachiasmatic nucleus in the hypothalamus [2]. Nocturnal BP decline (dipping) is an established predictor of cardiovascular diseases and high mortality compared with conventional BP measures, such as daytime BP and office BP. The lack of dipping (nondipper pattern) is a high-risk marker of target organ damage and cardiovascular events [3,4,5]. Nondipper patterns of circadian BP variability can be explained by risk factors such as aging, obesity, and diabetes; however, the factors causing nondipper patterns are not fully understood [6].
Light information is critically important in synchronizing human biological rhythms to environmental conditions [7]. The action spectrum of light information for human circadian physiology shows a peak at a shorter wavelength than that of visual information [8]. Previous experimental studies suggested that bright light intervention during daytime in healthy participants and elderly patients with insomnia significantly increases melatonin secretion and sleep quality [9, 10]. Additionally, in our previous epidemiological study, decreases in daytime light exposure were significantly associated with decreases in nighttime melatonin levels among elderly individuals [11]. Decreased melatonin levels and poor sleep quality were related to higher vascular tone, increased catecholamine levels, and sympathetic activity during nighttime, resulting in an increased nighttime BP [12, 13].
Aging significantly progresses cloudiness in the crystalline lens, which causes decreased light reception to the retina. Age-related cataracts are associated with a significantly lower reception of shorter wavelengths to which intrinsically photosensitive retinal ganglion cells, primary light receptors in the retina are more sensitive [14]. Therefore, we hypothesized that the prevalence of the nondipper pattern of circadian BP variability is higher in elderly individuals with cataracts than in those without cataracts. Although the association between cataracts and hypertension based on conventional BP measures has been investigated, to the best of our knowledge, no previous studies have evaluated the association of cataracts with circadian BP variability [15].
The purpose of this study was to determine the relationship between cataract and circadian BP variability in elderly individuals, where it would be tested that dipping status is different among cataract subtypes.
Methods
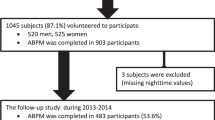
Participants
A total of 1127 community-dwelling elderly subjects aged ≥60 years were voluntarily enrolled in the Housing Environments and Health Investigation among Japanese Older People in Nara, Kansai Region: a prospective community-based cohort (HEIJO-KYO) study conducted between September and April 2010 to 2014 [11]. Of these, a senior ophthalmologist assessed the ocular status using slit lamp photographs after pupillary dilatation in 661 participants. Participants with intraocular lens (IOL) implanted (n = 100), insufficient pupil dilation for evaluation (n = 102), and corneal opacity (n = 1) in either eye were excluded. Therefore, data from the remaining 458 participants were studied. Retroilluminations necessary for the assessment of cortical and posterior subcapsular opacity were unavailable for some participants (n = 7). All participants provided written informed consent. The study protocol was approved by the Nara Medical University ethics committee.
Assessment of cataracts
Ocular status was assessed using photographs of anterior segments with the slit lamp biomicroscopy (SL 130, Carl Zeiss Meditec AG, Germany) by a senior ophthalmologist (KM) after pupillary dilatation using topical 5% phenylephrine hydrochloride (Kowa Pharmaceutical Co., Ltd, Tokyo, Japan). To avoid a significant risk of acute primary angle closure, pupillary dilatation was not performed for participants with a narrow angle. Nuclear sclerosis was assessed using a narrow-slit beam oriented 45° to the line of sight, and cortical and posterior subcapsular opacities were assessed using a retroillumination photograph. Cataract was graded using the Lens Opacities Classification System III (LOCS III) chart with 0.25-unit intervals by another senior ophthalmologist (TY) who was masked to participants’ medical information [16]. To consider light reception to the bilateral retina, nuclear cataract was defined as ≥3.0 in both eyes, cortical cataract as ≥2.0 in both eyes, and posterior subcapsular cataract (PSC) as ≥2.0 in both eyes and categorized as nuclear cataract, cortical cataract, PSC, and no cataract in at least one eye. Agreement for nuclear cataract graded between the two-senior ophthalmologist (TY and KM) in the initial consecutive 276 eyes of 138 participants was sufficiently high (continuous data: Spearman’s rank correlation coefficient, 0.97; categorized data of ≥3.0: Kappa coefficient = 0.99). Typical photographs of cataract subtypes graded using the LOCS III chart are shown in Fig. 1.
Photographs of cataract subtypes graded using the Lens Opacities Classification System III. Panels a, b, and c indicate typical nuclear color grades 2, 3, and 4, respectively. The nuclear color gradually becomes deep yellow with increasing grade. Panels d, e, and f indicate typical cortical cataract grades 1, 2, and 3, respectively. Retroillumination images indicate cortical opacity (arrow) located in the peripheral lesion of the pupil. The area of cortical opacities expands with increased grade. Panles g, h, and i indicate typical posterior subcapsular grades 1, 2, and 3, respectively. Posterior subcapsular opacity (arrowhead) located near the center of the pupil. The area of posterior subcapsular opacity expands with increasing grade
Measurement of circadian BP variability
Ambulatory BP (ABP) monitoring was performed using a validated ambulatory recorder (TM-2430; A&D Co. Ltd., Tokyo, Japan) and a cuff on the nondominant arm. BP was measured at 30-min intervals for 48 h. Daytime and nighttime were defined as out-of-bed and in-bed periods given in the sleep diary entries, respectively. BPs measured <10 times during daytime or <5 times during nighttime, as the result of errors, were excluded from analyses. Mean daytime and nighttime systolic BPs (SBPs) were used as ABP parameters. Dipping was defined as the percentage of nighttime SBP decline relative to daytime SBP. A nondipper pattern of BP was defined as a <10% decline in the mean nighttime SBP relative to the mean daytime SBP [17]. The day-to-day reproducibility of dipping from the present study samples was moderate (intraclass correlation coefficient, 0.58; 95% confidence interval [CI], 0.52–0.64).
Measurements of the covariates
Body mass index (BMI) was calculated as weight (kg) by height (m2). Current smoking, economic, and medical status were evaluated using a self-administered questionnaire. Diabetes mellitus was determined based on medical history, current use of anti-diabetic therapy, and fasting plasma glucose and glycated hemoglobin levels. Glaucoma was determined based on medical history and current use of anti-glaucoma eye drops. A standardized sleep and urination diary was used to estimate bedtimes, rising times, and a nocturnal void frequency. An actigraph (Actiwatch 2; Respironics Inc., Murrysville, PA, USA) on the nondominant wrist was used to record physical activity and ambulatory light intensity at 1-min intervals for two consecutive daytimes. Details for the measurements of daytime light exposure were previously reported [11].
Statistical analysis
Means and proportions were compared between the groups with and without a nondipper pattern of BP using unpaired t- and chi-square tests, respectively. Comparisons between cataract subtypes were performed using linear or logistic regression analysis with dummy variables for cataract status. In multivariable logistic regression analysis, odds ratios (ORs) and 95% CI for nondipper pattern of BP in relation to cataract subtypes were simultaneously adjusted for variables that were marginally significantly associated with nondipper pattern (P < 0.30), such as age (per 5 years), obesity (BMI ≥ 25 vs. < 25 kg/m2), antihypertensive drug use (yes vs. no), diabetes (yes vs. no), nocturnal void frequency (none, 1, 2, and ≥3 times/night), and daytime physical activity (per 100 counts/min) in the univariate comparisons (Table 1). Statistical analyses were performed using SPSS 24.0 for Windows (IBM SPSS Inc., Chicago, IL, USA). A two-sided P < 0.05 was considered statistically significant.
Results
The mean (standard deviation) age of the 458 participants was 69.1 (6.4) years, and 235 (51.3%) individuals were male. The mean daytime and nighttime SBPs were 132.9 (13.8) and 113.6 (15.7) mmHg, respectively, and the mean dipping was 14.4 (8.4)%. The number of participants having a nondipper pattern of BP was 127 (27.7%). The nondipper pattern was marginally to significantly (P < 0.30) associated with older age, obesity, more antihypertensive drug use, diabetes, higher nocturnal void frequency, and less daytime physical activity (Table 1). In addition, the relationships between these parameters and cataract status are suggested in the supplemental table.
The number of participants without cataract, with nuclear cataract, with cortical cataract, and with PSC was 290 (63.3%), 66 (14.4%), 106 (23.5%), and 28 (6.2%), respectively (Table 2). Daytime SBP did not significantly differ between the groups without cataract and with nuclear cataract, whereas nighttime SBP was significantly higher by 4.3 mmHg (95% CI, 0.1–8.4) in the group with nuclear cataract than in that without cataract, resulting in a significantly smaller dipping in the group with nuclear cataract by 2.6% (95% CI, 0.4–4.8). In contrast, there were no significant differences in dipping between the groups without cataract and with cortical cataract (difference, −0.8%; 95% CI, −2.7 to 1.0) or PSC (difference, −1.2%; 95% CI, −4.5 to 2.2).
The prevalence of nondipper patterns was 42.4% and 25.9% in the groups with nuclear cataracts and those without cataracts, respectively (Table 3). Logistic regression analysis revealed a significantly higher OR for the nondipper pattern in the group with nuclear cataracts than in the group without (OR, 2.13; 95% CI, 1.24–3.68; P = 0.007). The association was significant between the groups with nuclear cataracts only (n = 44) and those without cataracts (P = 0.041). In multivariable logistic regression analysis adjusted for potential confounders, such as age, obesity, diabetes, antihypertensive drug use, nocturnal void frequency, and physical activity, OR for nondipper pattern was significantly higher in the group with nuclear cataracts than in that without cataracts (OR, 1.81; 95% CI, 1.01–3.24; P = 0.047). Additionally, adjustment for each antihypertensive drug class, i.e., calcium-channel blockers (n = 116), angiotensin converting enzyme inhibitors/angiotensin receptor blockers (n = 120), diuretics (n = 20), or alpha-/beta-blockers (n = 18), instead of the parameter of any antihypertensive treatment, did not significantly change the main results (data not shown). Further adjustment for glaucoma (prevalence, 4.1%) or daytime light exposure (median, 346.8 lux; interquartile range, 170.1–770.6) did not change this (glaucoma adjusted: OR, 1.82; 95% CI, 1.02–3.27; P = 0.044; light exposure adjusted: OR, 1.83; 95% CI, 1.02–3.29; P = 0.042). In contrast, there were no significant differences in ORs for the nondipper pattern in the group with cortical cataracts (OR, 0.87; 95% CI, 0.52–1.48; P = 0.61) or PSCs (OR, 0.95; 95% CI, 0.38–2.34; P = 0.95) compared to the group without cataracts.
Discussion
The present study suggested that circadian BP variability was significantly diminished in elderly individuals with nuclear cataracts but not in those with cortical cataracts or PSCs. These results are independent of known risk factors for nondipper patterns of BP. In addition, the association between nuclear cataracts and the nondipper pattern of circadian BP variability was independent of daytime light exposure and physical activity.
To the best of our knowledge, the present study is the first to report associations between cataract subtypes and circadian BP variability in a general population. A meta-analysis that included approximately 300,000 individuals from nine previous cohort studies suggested that hypertension based on conventional BP measures increases the incidence of PSC but not nuclear or cortical cataracts; however, evidence of cataracts as a risk factor for hypertension may be lacking [15]. In the present study, there were no significant differences in daytime SBP in individuals with and without any type of cataract, whereas nighttime SBP was increased in individuals with nuclear cataract, resulting in a smaller dipping percentage. The associations of PSC and cortical cataract with a nondipper pattern were not significant, although this may have been caused by the relatively smaller case size of graded ≥3.0 for cortical cataract (n = 27; prevalence, 6.0%) and PSC (n = 6; prevalence, 1.3%) than for nuclear cataract (n = 66, 14.4%). In addition, lesser lens opacity in the central area, possibly related to light reception, in cortical cataracts and PSCs than in nuclear cataracts may be the cause of the nonsignificant association. A lens cloudiness with yellowing, typically found in nuclear cataracts, was reported to be associated with less transmission for short wavelengths, especially after the age of 70 years [18]. Further longitudinal studies with larger sample sizes investigating the association between cataract subtypes and subsequent changes in circadian BP variability are needed.
Although the mechanisms underlying the association between nuclear cataracts and nondipper patterns of BP variation are not fully understood, circadian misalignment and sleep disturbances induced by cataracts may contribute to BP changes. Senile cataracts are associated with significantly less light reception, particularly in shorter wavelengths, to which human circadian physiology is sensitive [14]. Previous studies have suggested that bright light intervention during the daytime significantly increases nighttime melatonin secretion and sleep quality [9, 10]. Melatonin increases endothelium-derived nitric oxide, which decreases vascular tone [12]. Circadian misalignment and poor sleep quality have been reported to increase catecholamines, such as epinephrine and norepinephrine levels, resulting in increased sympathetic activity [13, 19]. These increases in the vascular tone, catecholamines, and sympathetic activity during nighttime play significant roles in the diminished circadian BP variability. In our previous reports, we observed a significant association between increased daytime light exposure and higher nighttime melatonin levels and the associations of higher melatonin levels and better sleep quality with lower nighttime BP and larger dipping [11, 20, 21]. These potential mechanisms should be further investigated.
Cataract surgery may be a therapeutic option for aligning circadian BP variability and preventing cardiovascular diseases; however, this would require further interventional study. Cataract surgery, replacement of clouded crystalline lenses with IOLs, drastically increases the capacity for light reception to the retina [14]. A Japanese study using a pretest-posttest design suggested significant decreases in daytime SBP and diastolic BP based on a self-report questionnaire at 1 week and 1 month after IOL implantation compared with data at baseline [22]. In addition, cataract surgery significantly improved sleep quality as measured using self-reported questionnaires [23, 24]. Additionally, in our previous study, cataract surgery was significantly associated with objectively measured sleep quality, but urinary levels of melatonin metabolite did not differ between individuals with and without cataract surgery [25].
The strength of the present study was its adjustment of statistical models for daily light exposure profiles that could be potential confounding factors. In addition, ABP monitoring performed on multiple days may have minimized the potential for misclassification in circadian BP status misclassification, although the day-to-day reproducibility of dipping was moderate. However, the present study has some limitations to describe. First, the cross-sectional design precluded the assessment of causality. Second, the case size of cortical cataracts and PSCs may be small to detect the significance of the association with circadian BP variability. Additionally, for the same reason, we could not conduct quantitative analysis on the association between cataract grades in addition to exclusive cataract categories and circadian BP status, suggesting that future studies with large case sizes are needed. Third, cataract was graded by a single senior ophthalmologist, which may have possibly resulted in misclassification; however, agreement for nuclear cataract graded with another senior ophthalmologist in the initial consecutive 276 eyes was sufficiently high. In addition, retinal information possibly associated with BP profiles was not considered in the present study [26, 27].
In conclusion, circadian BP variability was significantly diminished in elderly individuals with nuclear cataracts but not in those with cortical cataracts or PSCs. These results were independent of daytime light exposure and physical activity in addition to known risk factors for nondipper patterns of BP, such as aging, obesity, and diabetes. Further longitudinal studies investigating the association of cataract subtypes with subsequent changes in circadian BP variability are needed.
References
Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–74.
Paschos GK, FitzGerald GA. Circadian clocks and vascular function. Circ Res. 2010;106:8337–41.
Cuspidi C, Giudici V, Negri F, Sala C, Mancia G. Left ventricular geometry, ambulatory blood pressure and extra-cardiac organ damage in untreated essential hypertension. Blood Press Monit. 2010;15:124–31.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51:55–61.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466–72.
Czeisler CA, Kronauer RE, Allan JS, Duffy JF, Jewett ME, Brown EN, et al. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science. 1989;244:1328–33.
Brainard GC, Hanifin JP, Greeson JM, Byrne B, Glickman G, Gerner E, et al. Action spectrum for melatonin regulation in humans: evidence for a novel circadian photoreceptor. J Neurosci. 2001;21:6405–12.
Hashimoto S, Kohsaka M, Nakamura K, Honma H, Honma S, Honma K. Midday exposure to bright light changes the circadian organization of plasma melatonin rhythm in humans. Neurosci Lett. 1997;221:89–92.
Mishima K, Okawa M, Shimizu T, Hishikawa Y. Diminished melatonin secretion in the elderly caused by insufficient environmental illumination. J Clin Endocrinol Metab. 2001;86:129–34.
Obayashi K, Saeki K, Iwamoto J, Okamoto N, Tomioka K, Nezu S, et al. Positive effect of daylight exposure on nocturnal urinary melatonin excretion in the elderly: a cross-sectional analysis of the HEIJO-KYO study. J Clin Endocrinol Metab. 2012;97:4166–73.
Arangino S, Cagnacci A, Angiolucci M, Vacca AM, Longu G, Volpe A, et al. Effects of melatonin on vascular reactivity, catecholamine levels, and blood pressure in healthy men. Am J Cardiol. 1999;83:1417–9.
Burgess HJ, Trinder J, Kim Y, Luke D. Sleep and circadian influences on cardiac autonomic nervous system activity. Am J Physiol. 1997;273:H1761–8.
Turner PL, Van Someren EJ, Mainster MA. The role of environmental light in sleep and health: effects of ocular aging and cataract surgery. Sleep Med Rev. 2010;14:269–80.
Yu X, Lyu D, Dong X, He J, Yao K. Hypertension and risk of cataract: a meta-analysis. PLoS ONE. 2014;9:e114012.
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111:831–6.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Artigas JM, Felipe A, Navea A, Fandiño A, Artigas C. Spectral transmission of the human crystalline lens in adult and elderly persons: color and total transmission of visible light. Invest Ophthalmol Vis Sci. 2012;53:4076–84.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA. 2009;106:4453–8.
Obayashi K, Saeki K, Tone N, Kurumatani N. Relationship between melatonin secretion and nighttime blood pressure in elderly individuals with and without antihypertensive treatment: a cross-sectional study of the HEIJO-KYO cohort. Hypertens Res. 2014;37:908–13.
Oume M, Obayashi K, Asai Y, Ogura M, Takeuchi K, Tai Y, et al. Objective sleep quality and night-time blood pressure in the general elderly population: a cross-sectional study of the HEIJO-KYO cohort. J Hypertens. 2018;36:601–7.
Ichikawa K. Changes in blood pressure and sleep duration in patients with blue light-blocking/yellow-tinted intraocular lens (CHUKYO study). Hypertens Res. 2014;37:659–64.
Asplund R, Ejdervik Lindblad B. The development of sleep in persons undergoing cataract surgery. Arch Gerontol Geriatr. 2002;35:179–87.
Alexander I, Cuthbertson FM, Ratnarajan G, Safa R, Mellington FE, Foster RG, et al. Impact of cataract surgery on sleep in patients receiving either ultraviolet-blocking or blue-filtering intraocular lens implants. Invest Ophthalmol Vis Sci. 2014;55:4999–5004.
Obayashi K, Saeki K, Miyata K, Nishi T, Tone N, Ogata N, et al. Comparisons of objective sleep quality between elderly individuals with and without cataract surgery: a cross-sectional study of the HEIJO-KYO cohort. J Epidemiol. 2015;25:529–35.
Smith W, Malan NT, Schutte AE, Schutte R, Mc Mels C, Vilser W, et al. Retinal vessel caliber and its relationship with nocturnal blood pressure dipping status: the SABPA study. Hypertens Res. 2016;39:730–6.
Gu YM, Petit T, Wei FF, Thijs L, Jacobs L, Zhang ZY, et al. Renal glomerular dysfunction in relation to retinal arteriolar narrowing and high pulse pressure in seniors. Hypertens Res. 2016;39:138–43.
Acknowledgements
We would like to thank Sachiko Uemura-Sogahara, Naomi Takenaka, Keiko Nakajima for their valuable help with data collection.
Funding
This work was supported by research fundings from the Department of Indoor Environmental Medicine, Nara Medical University; JSPS KAKENHI (grant numbers: 24790774, 22790567, 25860447, 25461393, 15H04776, and 15H04777); the Mitsui Sumitomo Insurance Welfare Foundation; the Meiji Yasuda Life Foundation of Health and Welfare; the Osaka Gas Group Welfare Foundation; the Japan Diabetes Foundation; the Daiwa Securities Health Foundation; the Japan Science and Technology Agency; YKK AP Inc.; Ushio Inc.; the Nara Prefecture Health Promotion Foundation; a Nara Medical University Grant-in-Aid for Collaborative Research Projects; the Tokyo Electric Power Company; EnviroLife Research Institute Co., Ltd.; and Sekisui Chemical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KO and KS received research grants from YKK AP Inc.; Ushio Inc.; Tokyo Electric Power Company; EnviroLife Research Institute Co., Ltd.; and Sekisui Chemical Co., Ltd. The remaining authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Yoshikawa, T., Obayashi, K., Miyata, K. et al. Diminished circadian blood pressure variability in elderly individuals with nuclear cataracts: cross-sectional analysis in the HEIJO-KYO cohort. Hypertens Res 42, 204–210 (2019). https://doi.org/10.1038/s41440-018-0140-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-018-0140-3