Abstract
The importance of cosyntropin stimulation during adrenal vein sampling (AVS) is not fully established, partly due to insufficient AVS data relating the presence and absence of cosyntropin stimulation with postoperative outcome. Therefore, we investigated differences in AVS indices before and after cosyntropin stimulation, and determined whether unstimulated or stimulated AVS indices better correlated with treatment outcome. A retrospective study was conducted in two parts: one with 185 patients who underwent AVS and the other with 81 patients who underwent unilateral adrenalectomy for unilateral aldosterone oversecretion. The selectivity index (SI), lateralized ratio (LR), and contralateral ratio (CR) before and after cosyntropin stimulations were determined, along with blood pressure outcome 1 year after surgery. Primary aldosteronism was diagnosed according to the Japanese Endocrine Society 2009 guidelines. The percentage of AVS patients with successful catheterization, defined as unstimulated SI > 2 before and stimulated SI > 5, increased after cosyntropin stimulation from 52% to 93% and from 74% to 98% for the right and left adrenal veins, respectively. LR decreased after cosyntropin stimulation (P < 0.001). In the postoperative patients, complete and partial clinical success was achieved in 49 and 27%, respectively. Low CR (<1) and high LR (≥2.6) after cosyntropin stimulation better correlated with postoperative blood pressure outcome than those before stimulation (CR < 1 and LR ≥ 2). These data suggest that cosyntropin stimulation facilitated the judgment of catheter insertion and postcosyntropin AVS indices may be more useful for predicting treatment outcome after unilateral adrenalectomy. Further study should examine the usefulness of cosyntropin stimulation in AVS performed in other settings.
Similar content being viewed by others
Introduction
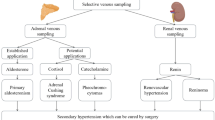
Adrenal vein sampling (AVS) is considered the gold standard for establishing laterality of aldosterone oversecretion in the diagnosis of primary aldosteronism (PA) before surgery [1]. However, there remain considerable disagreements in the protocol and diagnostic thresholds of AVS, including the use of stimulation by cosyntropin, a synthetic derivative of adrenocorticotrophic hormone (ACTH) [1,2,3].
Most diagnostic centers in Japan perform cosyntropin stimulation during AVS, partly because Japanese guidelines set aldosterone cutoff values for adrenal aldosterone oversecretion only after cosyntropin stimulation [4, 5]. However, in other areas of the world, unstimulated AVS is common, partly owing to the cost, time, and doubts on the efficacy of stimulated AVS on the outcome [2, 6].
The effects of cosyntropin stimulation on AVS-related metrics and the extent of agreement between unstimulated and stimulated values have been reported previously [7, 8]. A recent meta-analysis reported that AVS with ACTH stimulation can significantly reduce the number of unsuccessful cannulations without reducing the number of incorrect lateralizations [9]. Cosyntropin stimulation increases the selectivity index (SI), a measure of successful catheter insertion calculated as the ratio of plasma cortisol concentration in the adrenal vein to that in the infra-adrenal inferior vena cava (IVC) [10]. The 2014 Expert Consensus Statement suggested using unstimulated SI ≥ 2.0 and cosyntropin-stimulated SI ≥ 3.0 to define successful catheterization [1]. Other guidelines and statements recommend a higher cutoff for a postcosyntropin SI of ≥5 [4, 5, 11]. As the catheter insertion success rate in the same patient by the same radiologist on the same day is postulated to be similar before and after cosyntropin stimulation, analyzing the unstimulated and stimulated SI, and adrenal and peripheral cortisol values may help to explore the possibility that unstimulated AVS may be inappropriately labeling some catheter insertions as unsuccessful.
The lateralized ratio (LR) and contralateral ratio (CR) are mainly used to determine the indication for unilateral adrenalectomy. Cosyntropin stimulation decreased LR in some studies [8, 10, 12, 13] but had no effect in others [14]. LR cutoff values differ among different guidelines and statements. The 2014 Consensus refers to unstimulated LR between 2.0 and 4.0, and stimulated LR between 2.6 and 4.0 [1], whereas the Japan Endocrine Society (JES) guidelines referred to stimulated LR ≥ 2.6 to consider unilateral lesions [4, 15].
Therefore, we aimed to compare the AVS results with and without cosyntropin stimulations in terms of the rates of successful AVS, the rates of lateralized AVS, and the degree of correlation with blood pressure outcome.
Methods
Subjects
This retrospective, single-institution study was approved by the institutional review board of our facility without the reapplication of written informed consent due to its retrospective nature (Institutional Approval Number 4085). A total of 189 patients underwent AVS at Tokyo Women’s Medical University Hospital from January 2013 to December 2015 and 185 patients with sufficient data were analyzed. In a separate analysis, 126 patients with unilateral adrenalectomy performed for unilateral aldosterone oversecretion from 2000 to 2015 were reviewed, and of those, 81 patients with sufficient data, including AVS results and blood pressure control 1 year after surgery, were analyzed for treatment outcome. PA diagnosis was established according to the Japan Endocrine Society guidelines [4]: those with a plasma aldosterone concentration (PAC)/plasma renin activity ratio >200 were screened and those positive for at least 2 confirmatory tests including the captopril challenge test, upright furosemide loading test, and saline loading test were diagnosed as PA. AVS was performed in those who considered surgery a therapeutic option.
AVS procedure
AVS procedures were performed by or under the supervision of experienced radiologists. Contrast-enhanced multidetector computed tomography (CT) was performed before AVS to guide the identification of the right adrenal vein [16, 17] and an intraprocedural plasma cortisol concentration assay was not utilized. Medication was adjusted prior to AVS so that MR antagonists, angiotensin I-converting enzyme inhibitors, angiotensin II type 1 receptor blockers, diuretics, and β-adrenergic blockers were withdrawn for the appropriate durations specified in the guidelines [4] and hypokalemia was corrected. Sequential sampling was performed before and 15 min after cosyntropin (0.25 mg bolus intravenously) stimulation. Blood samples were taken from the IVC distal to the renal veins, right adrenal vein, left adrenal vein, common duct, and other positions. Plasma aldosterone and cortisol concentrations were measured using SPAC-S (FUJIREBIO, Inc., Tokyo, Japan) and Elecsys Cortisol II (Roche Diagnostics K.K., Tokyo, Japan), respectively. The following AVS indices were calculated: SI = (adrenal vein plasma cortisol concentration)/(IVC plasma cortisol concentration); LR = (dominant adrenal aldosterone/cortisol)/(nondominant adrenal aldosterone/cortisol); and CR = (nondominant adrenal aldosterone/cortisol)/(IVC aldosterone/cortisol). All patients were analyzed irrespective of SI values. For those with dominant oversecretion from the left, the greater aldosterone/cortisol ratio from the left adrenal vein or that from the common duct was used to calculate LR.
Surgery and blood pressure outcome determination
Successful catheterization was determined as an SI of ≥2 before cosyntropin stimulation and ≥5 after cosyntropin stimulation [4]. We adopted the most commonly used precosyntropin SI cutoff and the strictest postcosyntropin SI cutoff value in the literature [2, 4]. Adrenal vein cortisol concentration references of ≥30 µg/dL before cosyntropin stimulation and ≥200 µg/dL after cosyntropin stimulation [18] were also considered in the clinical judgment regarding successful catheterization [5].
The decision to offer surgery was mainly based on the combination of three criteria: (1) unilateral adrenal vein aldosterone concentration ≥14,000 pg/mL [4], (2) postcosyntropin LR ≥ 2.6 [4, 15], and (3) postcosyntropin CR < 1.0 [19, 20]. Precosyntropin indices and CT findings, and the presence of adrenal nodules or hypertrophy were also considered in the decision to offer unilateral adrenalectomy. Histopathology was examined on the postoperative specimen to confirm aldosterone-producing adenoma or hypertrophy.
Seated office BP was measured at clinic visits for regular postoperative follow-up after 5 min of rest in the sitting position against the back of a chair and without conversation. All BP measurements performed at a visit were averaged for analysis. The types and doses of antihypertensive medication, namely calcium channel blockers, angiotensin II type 1 receptor blockers, thiazide-type or loop diuretics, mineralocorticoid receptor blockers, α- adrenergic blockers, and β-adrenergic blockers, were recorded. Blood pressure management followed the Japanese Society of Hypertension 2009 or 2014 Guidelines [21, 22]. Antihypertensive medication 1 year after unilateral adrenalectomy was assessed to categorize patients as “complete,” “partial,” or “absent” clinical success in terms of antihypertensive medication. We assessed the number of types of antihypertensive medication in addition to the defined daily doses (DDD) of antihypertensive medication as outlined in the PASO consensus [23]. Patients categorized as complete or partial clinical success showed office blood pressures below 140/90 mm Hg 1 year after surgery. Biochemical outcomes were assessed based on plasma potassium, use of potassium supplementation, aldosterone concentrations, and plasma renin activity.
Statistical analysis
Values of P < 0.05 were considered significant. Statistical analyses were carried out with JMP® Pro 15 (SAS Institute, Inc., Cary, NC) or SPSS for Windows statistical package (version 21; SPSS, Inc., Chicago, IL). Spearman’s rank correlation or Wilcoxon’s signed-rank test was used for nonparametric comparisons.
Results
Relations between unstimulated and ACTH-stimulated AVS indices
The clinical features of the 185 AVS patients analyzed are summarized in Table 1. SI in both the right and left adrenal veins was significantly increased (P < 0.0001 for both sides), and LR and CR were decreased (P < 0.0001 and P = 0.0059, respectively) after cosyntropin stimulation.
The percentage of AVS patients with successful catheterization determined by SI values increased drastically after cosyntropin stimulation (Fig. 1). For the right adrenal vein, only 52% of AVS patients showed precosyntropin SI ≥ 2, but after cosyntropin stimulation, 93% showed SI ≥ 5. The success rate for the left adrenal vein increased from 74% to 98% after cosyntropin stimulation in the same series of patients. Notably, there was a significant overlap between the absolute values of plasma cortisol concentration from IVC and adrenal veins without cosyntropin stimulation (Fig. 2); the 95th percentile value for IVC cortisol (27.5 µg/dL) was roughly equivalent to the median cortisol concentration in adrenal veins before cosyntropin stimulation (right 24.8 µg/dL, left 32.7 µg/dL).
Selectivity index (SI) before and after 0.25 mg bolus cosyntropin simulation in 185 adrenal vein sampling (AVS) patients. SI = adrenal cortisol/inferior vena cava cortisol. a Right adrenal vein and b left adrenal vein. Dotted lines indicate the cutoff values for unstimulated SI of 2 and stimulated SI of 5
LR decreased after cosyntropin stimulation and the rate of lateral aldosterone secretion (LR ≥ 2 before and LR ≥ 2.6 after cosyntropin stimulation) decreased from 72.4% to 36.2% after stimulation (Fig. 3a). Of note, the side with the greater adrenal aldosterone/cortisol ratio differed before and after cosyntropin stimulation in 26.5% of patients. Of 49 such patients, 3 showing postcosyntropin LR ≥ 2.6 had either low SI or the use of topical steroids. The judgment of lateral secretion differed in 106 patients (57.3%): 74 patients (40.0%) were judged lateral only without cosyntropin and 6 patients (3.2%) were judged lateral only after cosyntropin stimulation.
a Lateralized ratio (LR) before and after cosyntropin stimulation of 185 adrenal vein sampling (AVS) patients. LR = (dominant adrenal aldosterone/cortisol)/(nondominant adrenal aldosterone/cortisol). Dotted lines indicate the cutoff values for unstimulated LR of 2 and stimulated LR of 4. b–d LR and postoperative BP outcome in 81 unilateral adrenalectomy patients. b Unstimulated LR with a cutoff of 2.0. c Stimulated LR with a cutoff of 2.6. d Stimulated LR with a cutoff of 4.0. Spearman’s rank correlation test
Stimulated and unstimulated AVS indices and blood pressure outcome after unilateral adrenalectomy
The clinical features of the 81 unilateral adrenalectomy patients are summarized in Table 2. Histopathology of the postoperative specimen revealed cortical adenoma in 63 patients, cortical adenoma with hyperplasia in 15 patients, and hyperplasia in 3 patients. Adrenal pathology did not significantly correlate with BP outcome (P = 0.342). Similar to the 185 AVS patients, those with adrenalectomy showed significantly decreased LR (P = 0.023, Wilcoxon’s signed-rank test) and CR (P < 0.001) after cosyntropin stimulation.
After adrenalectomy, 49% of patients showed complete and 27% showed partial clinical success at 1 year in terms of the number of types of antihypertensive medication. Correlation data using DDD were generally similar to those using the number of types of antihypertensive medications (Supplementary Figures). Patients with stimulated LR ≥ 2.6 showed better clinical outcome and this correlation was significant only with stimulated LR and not with unstimulated LR with a cutoff of 2 (Fig. 3b, c). Interestingly, stimulated LR no longer significantly correlated with BP outcome when the LR threshold was increased to 4 (P = 0.27) (Fig. 3d). Of 8 patients with postcosyntropin LR between 2.6 and 4, 63% showed complete and 25% showed partial clinical success, indicating a possible better postoperative outcome than that of the total patients. In terms of CR, the relationship to postoperative clinical success was not significant with unstimulated CR (Fig. 4a), but those with stimulated CR less than 1 showed a better rate of clinical success, which was highly significant (P < 0.001) (Fig. 4b). In the current series, virtually all patients achieved complete biochemical success; therefore, postoperative biochemical success was not statistically analyzed.
Discussion
Assessment of catheterization and laterality in unstimulated and stimulated AVS
Differences in unstimulated and ACTH-stimulated AVS indices were examined along with 1-year postoperative blood pressure outcome and we found that cosyntropin stimulation led to a marked increase in the rate of AVS judged to be successful, a decrease in the rate of lateralized AVS, and a better correlation of AVS indices (CR and LR) with postoperative BP outcome.
It has been reported that the SI, a measure of successful adrenal vein catheterization, increases with cosyntropin stimulation. This can be a great benefit if similar diagnostic accuracy is maintained. In this study, because both unstimulated and stimulated measurements were performed in the same patients on the same day by the same radiologists, we expected the actual rate of successful catheterization to be relatively similar in unstimulated and stimulated AVS. As ACTH increases adrenal blood flow [24], cosyntropin stimulation may have alleviated the difficulty in blood collection from the right adrenal vein to some extent. We suspect that some of our unstimulated AVS patients may have been inappropriately labeled as unsuccessful even though the catheters were correctly placed in the adrenal veins because of physiological cortisol fluctuations and nonsimultaneous sampling. When performing AVS without cosyntropin stimulation, measures are taken to minimize variations in cortisol concentration, such as creating a relaxed atmosphere, resting enough before and during the procedure, performing AVS at fixed times during the day, and performing bilateral simultaneous sampling from both adrenal veins [25]. Although these measures may be effective to some extent, it might be more feasible to perform AVS with cosyntropin.
Unstimulated AVS is being used in many centers worldwide, and the usefulness of unstimulated AVS has been established [2]. Our study does not contradict the usefulness of unstimulated AVS. Our patients underwent adrenalectomy because they were expected to benefit from the surgery, and because a high proportion of patients achieved clinical and biochemical success, it may have been difficult to show the diagnostic ability of unstimulated AVS.
AVS is considered a difficult procedure and is therefore not performed at a sufficient number of centers, even though it is the current gold standard to establish laterality. Implementation of cosyntropin stimulation may help reduce such strain by providing easier confirmation of successful catheterization.
Cosyntropin stimulation significantly reduced the rate of lateralized patients in our study. In the operated patients, a decrease in the median LR after cosyntropin stimulation was also observed, but to a lesser degree. A reduction in LR after cosyntropin stimulation has been observed in previous studies, and it is considered a significant drawback of cosyntropin stimulation [10]. Moreover, the ACTH stimulation test is used in some centers to diagnose PA and distinguish APA from bilateral aldosterone excess [26]. Unilateral PA showed a greater decrease in the PAC/cortisol ratio, but the ratio remained higher in unilateral PA than in bilateral PA after ACTH stimulation. As a decrease in the PAC/cortisol ratio in unilateral PA likely translates into decreased LR in stimulated AVS, the finding may suggest that decreased LR does not necessarily compromise the diagnostic ability of stimulated AVS. In this respect, the usefulness of employing the PAC/cortisol ratio during AVS in addition to LR for operative indication may be a subject of future study.
Unstimulated and stimulated AVS indices and association with postoperative blood pressure outcome
Postoperative clinical outcome after adrenalectomy is known to be influenced by factors such as age, sex, body mass index, preoperative blood pressure levels, kidney function, serum potassium levels, and the presence of diabetes mellitus [27, 28]. Umakoshi et al. [29] found that cosyntropin-stimulated LR predicted postoperative outcome. Some studies [28, 30] have examined postoperative outcome and AVS indices both before and after cosyntropin stimulation. In our previous study, using the multivariate model, body mass index and stimulated CR were significantly correlated with resolution outcome [28]. In our present study focused on ACTH stimulation, postoperative clinical improvement was correlated with high stimulated LR ( ≥ 2.6) and low stimulated CR ( < 1). Unstimulated LR or CR was not significantly related to postoperative BP improvement, but as our study included only a small number of patients who did not meet unstimulated or stimulated LR and CR thresholds for operation, our results do not contradict the usefulness of unstimulated AVS. Our result that stimulated LR ≥ 2.6 correlated more strongly than stimulated LR ≥ 4.0 with postoperative clinical success may imply that adopting a more lenient stimulated LR value may be considered for some patients for operative indication in combination with other factors such as stimulated CR and this should be examined in further studies.
Strengths and limitations
The strengths of the study include our examination of a relatively large number of patients in which unstimulated and stimulated AVS indices were available in the same patient on the same day by the same radiologist, minimizing factors that potentially cause variability. Limitations of the study include those inherent to retrospective studies of PA, such as selection bias at different steps of PA diagnosis: patient screening, functional confirmation tests, AVS, and adrenalectomy. We used bolus cosyntropin stimulation in the current study, but there can be variability in aldosterone and cortisol concentrations depending on the time between injection and sampling. The results of continuous cosyntropin infusion should be assessed in future analyses. Our 185 AVS patients included those with low SI and AVS procedures performed during different times of day. The AVS result analysis included a small percentage of PA patients with concurrent cortisol oversecretion and/or medications that affect renin and aldosterone measurements. The decision to offer unilateral adrenalectomy was primarily based on postcosyntropin AVS indices. As randomized, large-scale, prospective study of PA is difficult to conduct, we believe that our study, even with limitations, still provides us with information partly on which to base clinical decisions.
Conclusions
Cosyntropin use in AVS facilitated the identification of successful catheterization and postcosyntropin AVS indices were more useful in predicting the blood pressure response after unilateral adrenalectomy. Taken together, our results suggest the importance and usefulness of cosyntropin stimulation in AVS. Further information, such as on the applicability of our findings in other settings, would be helpful for improving the execution and interpretation of AVS for better treatment outcomes.
References
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension 2014;63:151–60.
Rossi GP, Barisa M, Allolio B, Auchus RJ, Amar L, Cohen D, et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012;97:1606–14.
Bardet S, Chamontin B, Douillard C, Pagny JY, Hernigou A, Joffre F, et al. SFE/SFHTA/AFCE consensus on primary aldosteronism, part 4: Subtype diagnosis. Ann Endocrinol (Paris). 2016;77:208–13.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism-the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
The Japan Society of Endocrinology. Consensus statement on the clinical practice of primary aldosteronism in Japan. Folia Endocrinol Jpn. 2016;92.
Amar L, Baguet JP, Bardet S, Chaffanjon P, Chamontin B, Douillard C, et al. SFE/SFHTA/AFCE primary aldosteronism consensus: introduction and handbook. Ann Endocrinol (Paris). 2016;77:179–86.
Tanemoto M, Suzuki T, Abe M, Abe T, Ito S. Physiologic variance of corticotropin affects diagnosis in adrenal vein sampling. Eur J Endocrinol. 2009;160:459–63.
Nakamura Y, Satoh F, Morimoto R, Kudo M, Takase K, Gomez-Sanchez CE, et al. 18-oxocortisol measurement in adrenal vein sampling as a biomarker for subclassifying primary aldosteronism. J Clin Endocrinol Metab. 2011;96:E1272–8.
Laurent I, Astère M, Zheng F, Chen X, Yang J, Cheng Q, et al. Adrenal venous sampling with or without adrenocorticotropic hormone stimulation: a meta-analysis. J Clin Endocrinol Metab. 2018;104:1060–8.
Seccia TM, Miotto D, De Toni R, Pitter G, Mantero F, Pessina AC, et al. Adrenocorticotropic hormone stimulation during adrenal vein sampling for identifying surgically curable subtypes of primary aldosteronism: comparison of 3 different protocols. Hypertension 2009;53:761–6.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Carr CE, Cope C, Cohen DL, Fraker DL, Trerotola SO. Comparison of sequential versus simultaneous methods of adrenal venous sampling. J Vasc Inter Radiol. 2004;15:1245–50.
Rossi GP, Pitter G, Bernante P, Motta R, Feltrin G, Miotto D. Adrenal vein sampling for primary aldosteronism: the assessment of selectivity and lateralization of aldosterone excess baseline and after adrenocorticotropic hormone (ACTH) stimulation. J Hypertens. 2008;26:989–97.
Monticone S, Satoh F, Giacchetti G, Viola A, Morimoto R, Kudo M, et al. Effect of adrenocorticotropic hormone stimulation during adrenal vein sampling in primary aldosteronism. Hypertension 2012;59:840–6.
Satoh F, Abe T, Tanemoto M, Nakamura M, Abe M, Uruno A, et al. Localization of aldosterone-producing adrenocortical adenomas: significance of adrenal venous sampling. Hypertens Res. 2007;30:1083–95.
Morita S, Yamazaki H, Sonoyama Y, Nishina Y, Ichihara A, Sakai S. Successful adrenal venous sampling by non-experts with reference to CT images. Cardiovasc Interv Radiol. 2016;39:1001–6.
Morita S, Nishina Y, Yamazaki H, Sonoyama Y, Ichihara A, Sakai S. Dual adrenal venous phase contrast-enhanced MDCT for visualization of right adrenal veins in patients with primary aldosteronism. Eur Radiol. 2016;26:2073–7.
Omura M, Sasano H, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Clinical characteristics of aldosterone-producing microadenoma, macroadenoma, and idiopathic hyperaldosteronism in 93 patients with primary aldosteronism. Hypertens Res. 2006;29:883–9.
Umakoshi H, Tanase-Nakao K, Wada N, Ichijo T, Sone M, Inagaki N, et al. Importance of contralateral aldosterone suppression during adrenal vein sampling in the subtype evaluation of primary aldosteronism. Clin Endocrinol (Oxf). 2015;83:462–7.
Wolley MJ, Gordon RD, Ahmed AH, Stowasser M. Does contralateral suppression at adrenal venous sampling predict outcome following unilateral adrenalectomy for primary aldosteronism? A retrospective study. J Clin Endocrinol Metab. 2015;100:1477–84.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2009;32:3–107.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014;37:253–390.
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Lefebvre H, Thomas M, Duparc C, Bertherat J, Louiset E. Role of ACTH in the interactive/paracrine regulation of adrenal steroid secretion in physiological and pathophysiological conditions. Front Endocrinol (Lausanne). 2016;7:98.
Steichen O, Amar L. Diagnostic criteria for adrenal venous sampling. Curr Opin Endocrinol Diabetes Obes. 2016;23:218–24.
Kita T, Furukoji E, Sakae T, Kitamura K. Efficient screening of patients with aldosterone-producing adenoma using the ACTH stimulation test. Hypertens Res. 2019;42:801–6.
Steichen O, Zinzindohoué F, Plouin PF, Amar L. Outcomes of adrenalectomy in patients with unilateral primary aldosteronism: a review. Horm Metab Res. 2012;44:221–7.
Bokuda K, Yatabe M, Mizuguchi Y, Niiyama M, Seki Y, Watanabe D, et al. Body mass index and contralateral ratio predict outcome following unilateral adrenalectomy in primary aldosteronism. Hypertens Res. 2017;40:988–93.
Umakoshi H, Tsuiki M, Yokomoto-Umakoshi M, Takeda Y, Takashi Y, Kurihara I, et al. Correlation between lateralization index of adrenal venous sampling and standardized outcome in primary aldosteronism. J Endocr Soc. 2018;2:893–902.
Shibayama Y, Wada N, Naruse M, Kurihara I, Ito H, Yoneda T, et al. The occurrence of apparent bilateral aldosterone suppression in adrenal vein sampling for primary aldosteronism. J Endocr Soc. 2018;2:398–407.
Funding
The study was funded in part by Novartis Research Grant and Tanabe Mitsubishi Research Grant to MY and supported in part by a JSPS KAKENHI Grant Number 16H05316 to AI.
Author information
Authors and Affiliations
Contributions
The research was designed by MY, KB, and AI, and was conducted by MY, KB, SM, JY, YS, DW, TA, SM, SS, and AI. MY and KY analyzed the data and performed the statistical analysis. MY drafted the article. Critical revision of the article was performed by SM, JY, SM, and AI. MY was granted the JSH Women Investigator’s Award by the Japanese Society of Hypertension for this work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yatabe, M., Bokuda, K., Yamashita, K. et al. Cosyntropin stimulation in adrenal vein sampling improves the judgment of successful adrenal vein catheterization and outcome prediction for primary aldosteronism. Hypertens Res 43, 1105–1112 (2020). https://doi.org/10.1038/s41440-020-0445-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-020-0445-x