Abstract
The score based on the office systolic blood pressure, age, fasting blood glucose level, and estimated glomerular filtration rate (SAGE score) has been proposed as a useful marker to identify elevated values of carotid-femoral pulse wave velocity (PWV). The present cross-sectional study was conducted to examine whether the SAGE score is also a useful marker to identify subjects with elevated brachial-ankle PWV values in Japanese subjects with hypertension. We measured the brachial-ankle PWV and calculated the SAGE score in a total of 1019 employees of a Japanese company with hypertension and 817 subjects with hypertension derived from a multicenter study cohort. The analyses in this study were based on data from these two study groups as well as on a composite population of the two (n = 1836). The receiver operating characteristic curve analysis showed that the area under the curve to identify subjects with brachial-ankle PWV values of ≥1800 cm/s was over 0.70 in each of the three study groups. Even after adjustments, a SAGE score ≥7 had a significant odds ratio for identifying subjects with brachial-ankle PWV values ≥1800 cm/s in the 1836 study subjects from the composite occupational and multicenter study cohort (odds ratio = 2.1, 95% confidence interval = 1.4–3.0, P < 0.01). Thus, in Japanese subjects with hypertension, the SAGE score may be a useful marker for identifying subjects with elevated brachial-ankle PWV values.
Similar content being viewed by others
Introduction
Arterial stiffness, assessed by measuring pulse wave velocity (PVW), has been reported as an independent risk factor for the development of cardiovascular disease (CVD) [1,2,3]. However, the number of individuals with risk factors for CVD is large, and the applicability of PWV measurement on a large scale for assessing the risk of CVD is limited. Therefore, a simple marker is needed to identify patients requiring measurement of PWV as a marker of CV risk in daily clinical practice. PWV is affected by multiple risk factors, such as blood pressure and age, and it is thought that a marker based on the integration of multiple risk factors, rather than on any single risk factor [4,5,6,7,8,9], would be suitable to screen for subjects with elevated PWV values. Based on this background, the SAGE score (a score based on office systolic blood pressure (SBP), age, fasting blood glucose level and estimated glomerular filtration rate (eGFR)) has been proposed as useful for identifying subjects with elevated carotid-femoral PWV values among subjects with hypertension [10]. While carotid-femoral PWV is a commonly used marker of cardiovascular risk in Europe and the United States [3, 7, 8], in Asia, brachial-ankle PWV is used more frequently because of the ease of measurement [5, 6, 11]. Furthermore, a recent individual participant data meta-analysis identified brachial-ankle PWV as an independent predictor of future cardiovascular events [12, 13]. It is a simple-to-measure parameter that can be measured on a large scale. While the brachial-ankle PWV has been used in the management of subjects with CV risk factors or in health checkups conducted in the community or by a company [5, 6, 11], the predictive ability of the SAGE score, which is derived from very simple parameters, for elevated brachial-ankle PWV values remains unclear in subjects with hypertension.
The present cross-sectional study, conducted in subjects with hypertension derived from a Japanese occupational cohort [14, 15], a Japanese multicenter study cohort [16, 17], and a composite of the two cohorts, was aimed at examining whether the SAGE score might be a useful marker to identify subjects with elevated brachial-ankle PWV values among subjects with hypertension.
Methods
Design and subjects
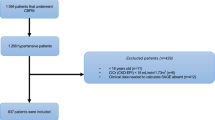
The present study was conducted in cohorts from two previously reported observational studies (i.e., an occupational cohort [14, 15] and subjects with hypertension from a multicenter study [16, 17]).
# Subjects with hypertension from the Japanese occupational cohort
The occupational cohort consisted of employees working at the headquarters of a single large Japanese construction company located in downtown Tokyo [14, 15]. Informed consent for participation in this study was obtained from each of the study participants prior to their enrollment in this study. The study was conducted with the approval of the Ethical Guidelines Committee of Tokyo Medical University (No. 209 and No. 210 in 2003). The health checkup data obtained for the years 2007 through 2015 were used for the present study. Of the 5857 subjects working at the headquarters of the construction company who had undergone measurement of the brachial-ankle PWV at least once [14], subjects with atrial fibrillation, ankle-brachial pressure index values of <0.95 (in cases with ABI < 0.95, the measured brachial-ankle PWV values are often inaccurate because the pressure waveform recorded at the ankle is obscure) [18], a history of cardiovascular disease or of undergoing hemodialysis, and/or for no data available on blood pressure, age, serum levels of creatinine and/or plasma levels of glucose were excluded. Patients with a systolic blood pressure of ≥140 mm Hg and/or a diastolic blood pressure of ≥90 mm Hg and/or prescribed medication for hypertension were defined as having hypertension. Subjects in the occupational cohort without hypertension were excluded (n = 4296), and 1019 subjects with hypertension from this occupational cohort were included in the present analyses.
# Subjects with hypertension from the Japanese multicenter study cohort
The subjects with hypertension enrolled in this study were the same as those registered in the multicenter prospective observational study, details of which are described elsewhere [16, 17], conducted with the participation of 17 university hospitals in Japan from June 2010 to October 2015. The subjects had a blood pressure of <150/95 mm Hg, were receiving antihypertensive treatment, and had been under follow-up at any of the participating centers for at least 6 months; [16] the data of patients that were obtained at the time of the first measurement of the brachial-ankle PWV were used for the present analyses. A total of 966 subjects were registered in this multicenter study (none of the subjects had atrial fibrillation) [16, 17], and the data of the brachial-ankle PWV recorded at the start of the study period were available for 874 subjects. Among these, 57 subjects were excluded because their ABI values were <0.95 and/or their laboratory data were not available. Finally, 817 subjects with hypertension were included in the present analyses.
# Subjects with hypertension from the combined Japanese occupational and multicenter study cohorts
The analyses were also conducted in composite of subjects (n = 1836) from the Japanese occupational cohort (n = 1019) and the multicenter study cohort (n = 817).
Measurement of brachial-ankle PWV
Brachial-ankle PWV was measured using a volume plethysmographic apparatus (Form/ABI, Omron Healthcare Co., Ltd., Kyoto, Japan), as previously described [11, 14, 15]. Briefly, occlusion cuffs connected to both the plethysmographic and oscillometric sensors were tied around both the upper arms and lower legs of the subjects lying in the supine position. The brachial and posttibial arterial pressures were measured by the oscillometric sensor. The measurements were conducted after the subjects had rested for at least 5 min in the supine position in an air-conditioned room (maintained at 24 °C) designated exclusively for this study.
Laboratory measurements
Serum concentrations of total cholesterol (TC), high-density lipoprotein cholesterol (HDL) and creatinine, as well as the blood glucose concentration, were measured using standard enzymatic methods (Falco Biosystems Co. Ltd, Tokyo). The estimated glomerular filtration rate (eGFR) was calculated from serum creatinine using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation for Japanese subjects [19] but not the original equation [20].
Calculation of the SAGE score
For this study, the SAGE score, to predict elevated values of brachial-ankle PWV, was calculated based on a slight modification of the originally described method (i.e., the eGFR was calculated by the CKD-EPI equation for Japanese subjects) [19] (Table 1). For SBP, thresholds of 140, 160 and 180 mm Hg were used. For age, thresholds of 50, 60 and 70 years were used. For blood glucose, the threshold of 125 mg/dl for patients with glycemia at diabetic levels was used. Finally, for renal function, eGFR thresholds of 90, 60, 30 and 15 ml/min/1.73 m2 were used. Patients with kidney failure (i.e., eGFR <15 ml/min per 1.73 m2) were excluded from the study. Then, the SAGE score was calculated as the sum of the scores for the four variables (SBP, age, plasma glucose and eGFR).
Statistical analysis
Data are expressed as the means ± SD, unless otherwise indicated. The differences in the measured values between groups were assessed by unpaired t test or McNemar’s nonparametric test. In addition, brachial-ankle PWV and the SAGE score were compared between groups by one-way analysis of variance with adjustments for sex, age, smoking status, body mass index, mean blood pressure, blood glucose level, and serum levels of total cholesterol, HDL cholesterol and creatinine.
Based on an individual-participants database of brachial-ankle PWV in the general population and in subjects with hypertension, Ohkuma et al. reported that the cutoff value of brachial-ankle PWV for predicting future occurrence of CVD was 1830 cm/s in subjects with hypertension [13]. Therefore, in the present study, elevated brachial-ankle PWV was defined by the cutoff value of 1800 cm/s in a cohort with hypertension. Receiver operator characteristic (ROC) curve analysis was applied to obtain the areas under the curve (AUCs) of the markers to identify subjects with brachial-ankle PWV values of ≥1800 cm/s, and the cutoff values for the identification of subjects with elevated brachial-ankle PWV values were examined.
Analyses were conducted using SPSS software (version 25.0; IBM/SPSS Inc., Armonk, NY, USA). The null hypothesis was rejected for values of ≥0.05 in all the statistical tests.
Results
Table 2 shows the clinical characteristics of the subjects with hypertension from the occupational cohort, the multicenter study cohort, and a composite of the two cohorts. The mean SAGE score and brachial-ankle PWV value were higher in the subjects with hypertension from the multicenter study than in those from the occupational cohort (Table 2).
The SAGE score showed a significant correlation with brachial-ankle PWV in the subjects with hypertension from the occupational cohort (R = 0.49, P < 0.01), multicenter study cohort (R = 0.51, P < 0.01), and the composite of the two cohorts (Supplementary Fig. 1). In addition, the brachial-ankle PWV value increased with increasing score for each variable used to calculate the SAGE score in the subjects with hypertension from the composite of the occupational and multicenter study cohorts (Supplementary Fig. 2); similar findings were obtained in each of the individual study cohorts (data not shown).
Table 3 summarizes the Youden’s index of each SAGE score from 5 to 8 in the subjects with hypertension. The ROC curve analyses showed a significant ability of the SAGE score to identify subjects with brachial-ankle PWV values of ≥1800 cm/s among subjects with hypertension from all three study groups (the area under the curve in all the groups was 0.7) (Fig. 1), and the Youden’s J statistics for different cutoff values of the SAGE score in all three groups are described in Fig. 1.
Areas under the curve from the receiver-operator characteristic curve analysis. For predicting baPWV ≥1800 cm/s, receiver operator characteristic curve analysis was used to identify subjects with baPWV ≥1800 cm/s. AUC area under the curve, SAGE score = score based on the office systolic blood pressure, age, glycemia level and estimated glomerular filtration rate score. baPWV brachial-ankle pulse wave velocity
Table 4 summarizes the sensitivities and specificities of different cutoff values of the SAGE score in the three study groups. The SAGE scores reflecting a positive likelihood ratio of ≥5 were 8–10.
Table 5 summarizes the results of the binary logistic regression analysis to determine the ability of the SAGE score to identify brachial-ankle PWV values ≥1800 cm/s in the three study groups. Because SBP and age are major determinants of brachial-ankle PWV, the cutoff values of age and SBP to identify subjects with brachial-ankle PWV values ≥1800 cm/s were determined by ROC curve analyses for the three study groups. The values of these two parameters for identifying brachial-ankle PWV values ≥1800 cm/s were 52 years and 142 mm Hg in the study subjects with hypertension derived from the occupational cohort, 65 years and 142 mm Hg in the subjects with hypertension from the multicenter study cohort, and 60 years and 142 mm Hg in the study subjects with hypertension from the composite of the occupational and multicenter study cohorts. Even after adjustments for age, SBP, and sex, the SAGE score was associated with a significant odds ratio for identifying elevated values of brachial-ankle PWV in the study subjects with hypertension from the occupational cohort and those from the composite of the occupational and multicenter study cohorts (Table 5).
Regarding the composite cohort, according to Youden’s method, a cutoff point of 5 provided the optimal combination of sensitivity and specificity. Higher cutoff points resulted in higher specificity at the cost of lower sensitivity. The cutoff point of 7 (i.e., score values ≥7) had a sensitivity of 57% and specificity of 80%. Thus, the use of this cutoff point would help decision making by accurately ruling out patients who are least likely to have elevated brachial ankle PWV (Table 5).
Discussion
The present study demonstrated a significant odds ratio for the SAGE score to identify subjects with elevated brachial-ankle PWV values among Japanese subjects with hypertension.
Several studies have reported associations between the risk factors for CVD and elevated carotid-femoral PWV values [2, 3, 8]. A recent meta-analysis demonstrated that among various risk factors for CVD, blood pressure and age are the major determinants of carotid-femoral PWV [4]. In addition, we demonstrated, based on the data of 12517 Japanese subjects, that blood pressure and age are also major determinants of brachial-ankle PWV [5]. Then, a collaborative study demonstrated an interaction between blood pressure and age in their relation to carotid-femoral PWV [8]. Furthermore, increased PWV is also observed in patients with diabetes mellitus and chronic kidney disease [6, 7, 11]. Thus, prediction of PWV based on any single risk factor may have a limitation. The SAGE score is a comprehensive marker calculated based on multiple risk factors for CVD [10], and the present study demonstrated that the SAGE score is a useful marker for identifying subjects with elevated brachial-ankle PWV values in Japanese subjects with hypertension, independent of the individual risk factors for CVD.
Xaplanteris et al. reported that the best cutoff value of the SAGE score for identifying elevated carotid-femoral PWV values was 8 in subjects with hypertension [10]. We attempted to examine the cutoff value of the SAGE score for identifying elevated brachial-ankle PWV values in subjects with hypertension derived from different cohorts. In a quantitative approach (according to the Youden index), the optimal cutoff ranged from 5 to 7 in the three cohorts. However, in a qualitative approach that prioritizes a satisfactory positive predictive value while retaining a high negative predictive value (meaning that subjects not referred would accurately be considered as least likely to have elevated brachial-ankle PWV and thus would not be deprived of the risk predictive value of this biomarker), the optimal cutoff for the composite cohort was 7. Any differences in the cutoff values of the SAGE score for identifying increased arterial stiffness as assessed by carotid-femoral PWV and brachial-ankle PWV may also be attributable to the fact that carotid-femoral PWV reflects the stiffness of the large-sized arteries and brachial-ankle PWV reflects the stiffness of the middle-sized to large-sized arteries. In addition, the ROC curve was not sufficiently steep to determine its peak for identifying brachial-ankle PWV values of ≥1800 cm/s in either group (Fig. 1). The mean SAGE score was higher in subjects with hypertension from the multicenter study cohort than in those from the occupational cohort. Therefore, the clinical characteristics that determine the SAGE score in the study cohort might affect the cutoff value of the SAGE score to identify subjects with elevated brachial-ankle PWV values.
Clinical implications
In relation to the screening methods for the risk of CVD, PWV might be placed as a second-line parameter in the screening system [11, 21]. The SAGE score can be calculated from the data obtained from the first-line screening [10] and applied to identify subjects needing for measurement of PWV. Furthermore, brachial-ankle PWV had a close relationship with the carotid-femoral PWV [22], and meta-analyses of individual-participants data have already demonstrated that not only carotid-femoral PWV but also brachial-ankle PWV are independent predictors of future cardiovascular events, independent of conventional CV risk assessment models, such as the Framingham risk score [12, 13, 23]. Therefore, the SAGE score might be a simple marker for risk assessment for CVD in first-line screening, independent of conventional CV risk assessment models.
Limitations
This study had several limitations. (1) Supplementary Fig. 3 depicts the histograms of the SAGE score and brachial-ankle pulse wave velocity in subjects with hypertension and in those without hypertension in the occupational cohort. They were skewed left in subjects without hypertension. In the occupational cohort of the present study, there were 4296 subjects without hypertension with a mean age of 41 years; among them, only 87 subjects (2%) had brachial-ankle PWV values ≥1600 cm/s (this brachial-ankle value is the cutoff value to identify subjects at high risk for cardiovascular disease in the general population [12]), and 21 subjects (0.5%) had brachial-ankle PWV values >1800 cm/s. Thus, the number of subjects with elevated brachial-ankle PWV values in middle-aged Japanese subjects without hypertension was small. In addition, in the subjects without hypertension from the occupational cohort, a SAGE score of 2 was the best cutoff value for identifying subjects with brachial-ankle PWV values ≥1600 cm/s (Supplementary Fig. 4). Age ≥50 years, SBP ≥ 140 mm Hg, eGFR <60 ml/min/1.73 m2, or fasting blood glucose >125 mg/dl alone would represent a SAGE score of 2. Thus, the applicability of the SAGE score in this particular form might be limited in subjects with a low risk for cardiovascular disease. Therefore, further studies in subjects with/without several risk factors for cardiovascular disease are needed to establish the precise cutoff value(s) of the SAGE score to identify subjects with increased arterial stiffness related to the development of CVD. (2) Sex differences and ethnic differences in the values of PWV have been reported [24, 25]. However, in the present study, the differences in the predictive ability of the SAGE score as a marker of PWV between male and female subjects and between subjects of different ethnicities were not examined. (3) Unlike the case for SBP, age and eGFR, the diabetic levels were bifurcated. The threshold of 125 mg/dl for patients with glycemia was defined as the diabetic level in the SAGE scoring system. On the other hand, the normal fasting glucose level is <110 mg/dl [26]. We attempted to use the modified SAGE score using this cutoff value for glycemia (i.e., fasting blood glucose ≥110 mg/dl and 126 mg/dl assigned a score of 2. The AUCs of the original SAGE score and modified SAGE score to identify subjects with brachial-ankle PWV values ≥1800 cm/s are summarized in the Supplementary Table. The results revealed no significant difference in the cutoff value obtained using the two fasting glucose levels (≥110 mg/dl and ≥126 mg/dl).
Conclusion
In Japanese subjects with hypertension, the SAGE score may be a useful marker for identifying subjects with elevated brachial-ankle PWV values.
References
Tomiyama H, Yamashina A. Non-invasive vascular function tests: their pathophysiological background and clinical application. Circ J 2010;74:24–33.
Safar ME. Arterial stiffness as a risk factor for clinical hypertension. Nat Rev Cardiol. 2018;15:97–105.
Yannoutsos A, Ahouah M, Dreyfuss Tubiana C, Topouchian J, Safar ME, et al. Aortic stiffness improves the prediction of both diagnosis and severity of coronary artery disease. Hypertens Res. 2018;41:118–25.
Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension 2009;54:1328–36.
Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T, et al. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement-a survey of 12517 subjects. Atherosclerosis 2003;166:303–9.
Tomiyama H, Hirayama Y, Hashimoto H, Yambe M, Yamada J, Koji Y, et al. The effects of changes in the metabolic syndrome detection status on arterial stiffening: a prospective study. Hypertens Res 2006;29:673–8.
Satoh H, Kishi R, Tsutsui H. Metabolic syndrome is a significant and independent risk factor for increased arterial stiffness in Japanese subjects. Hypertens Res 2009;32:1067–71.
Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J. 2010;31:2338–50.
Haraguchi N, Koyama T, Kuriyama N, Ozaki E, Matsui D, Watanabe I, et al. Assessment of anthropometric indices other than BMI to evaluate arterial stiffness. Hypertens Res. 2019;42:1599–605.
Xaplanteris P, Vlachopoulos C, Protogerou AD, Aznaouridis K, Terentes-Printzios D, Argyris AA, et al. A clinical score for prediction of elevated aortic stiffness: derivation and validation in 3943 hypertensive patients. J Hypertens 2019;37:339–46.
Tomiyama H, Matsumoto C, Shiina K, Yamashina A. Brachial-Ankle PWV: current status and future directions as a useful marker in the management of cardiovascular disease and/or cardiovascular risk factors. J Atheroscler Thromb. 2016;23:128–46.
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, et al. Collaborative group for j-bavel (japan brachial-ankle pulse wave velocity individual participant data meta-analysis of prospective studies)*. brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension 2017;69:1045–52.
Ohkuma T, Tomiyama H, Ninomiya T, Kario K, Hoshide S, Kita Y, et al. Collaborative Group for Japan brachial-ankle pulse wave velocity individual participant data meta-analysis of prospective studies (j-bavel). proposed cutoff value of brachial-ankle pulse wave velocity for the management of hypertension. Circ J 2017;81:1540–2.
Tomiyama H, Shiina K, Vlachopoulos C, Iwasaki Y, Matsumoto C, Kimura K, et al. Involvement of Arterial Stiffness and Inflammation in Hyperuricemia-Related Development of Hypertension. Hypertension 2018;72:739–45.
Tomiyama H, Komatsu S, Shiina K, Matsumoto C, Kimura K, Fujii M, et al. Effect of Wave Reflection and Arterial Stiffness on the Risk of Development of Hypertension in Japanese Men. J Am Heart Assoc. 2018;7:e008175 https://doi.org/10.1161/JAHA.117.008175.
Tomiyama H, Ishizu T, Kohro T, Matsumoto C, Higashi Y, Takase B, et al. Longitudinal association among endothelial function, arterial stiffness and subclinical organ damage in hypertension. Int J Cardiol. 2018;253:161–6. https://doi.org/10.1016/j.ijcard.2017.11.022
Tomiyama H, Kohro T, Higashi Y, Takase B, Suzuki T, Ishizu T, et al. A multicenter study design to assess the clinical usefulness of semi-automatic measurement of flow-mediated vasodilatation of the brachial artery. Int Heart J. 2012;53:170–5.
Motobe K, Tomiyama H, Koji Y, Yambe M, Gulinisa Z, Arai T, et al. Cut-off value of the ankle-brachial pressure index at which the accuracy of brachial-ankle pulse wave velocity measurement is diminished. Circ J 2005;69:55–60.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis. 2010;56:32–8.
Levey AS, Stevens LA. Estimating GFR using the CKD Epidemiology Collaboration (CKD-EPI) creatinine equation: more accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;55:622–7.
Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. American heart association council on hypertension. recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement From the American Heart Association. Hypertension 2015;66:698–722.
Tanaka H, Munakata M, Kawano Y, Ohishi M, Shoji T, Sugawara J, et al. Comparison between carotid-femoral and brachial-ankle pulse wave velocity as measures of arterial stiffness. J Hypertens 2009;27:2022–7.
Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63:636–46.
Avolio AP, Kuznetsova T, Heyndrickx GR, Kerkhof PLM, Li JK. Arterial flow, pulse pressure and pulse wave velocity in men and women at various ages. Adv Exp Med Biol. 2018;1065:153–68.
Rezai MR, Wallace AM, Sattar N, Finn JD, Wu FC, Cruickshank JK. Ethnic differences in aortic pulse wave velocity occur in the descending aorta and may be related to vitamin D. Hypertension. 2011;58:247–53.
American Diabetes Association. Standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S1–S193.
Funding
This study was partially supported financially by a Grant-in-Aid for scientific research from the Ministry of Health, Labour and Welfare, by the Japanese Atherosclerosis Prevention Research Fund (A study of Multi-center Assessment on the Clinical Usefulness of Semi-automatic Measurement of Flow-mediated Vasodilatation of the Brachial Artery: FMD-J study), and by the Omron Health Care Company, Kyoto, Japan.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The sponsor (Omron Health Care Company) assisted in the data formatting (i.e., the brachial-ankle pulse wave velocity data stored in the hard disc of the equipment used for measurement of the brachial-ankle pulse wave velocity was transferred to an Excel file); other than this, the company played no role in the design or conduct of the study, i.e., in the data collection, management, analysis or interpretation of the data, or in the preparation, review or approval of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tomiyama, H., Vlachopoulos, C., Xaplanteris, P. et al. Usefulness of the SAGE score to predict elevated values of brachial-ankle pulse wave velocity in Japanese subjects with hypertension. Hypertens Res 43, 1284–1292 (2020). https://doi.org/10.1038/s41440-020-0472-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-020-0472-7
Keywords
This article is cited by
-
LDL-C/HDL-C ratio as a predictor of atherosclerosis in the Japanese population: insights from a cross-sectional study
BMC Cardiovascular Disorders (2025)
-
Does elevated pulse wave velocity improve risk prediction in low-risk populations?
Hypertension Research (2025)
-
Definition of hyperfiltration taking into account age-related decline in renal function in kidney donor candidates with obesity and glucose tolerance disorder
Hypertension Research (2025)
-
A SAGE score cutoff that predicts high-pulse wave velocity as measured by oscillometric devices in Brazilian hypertensive patients
Hypertension Research (2022)