Abstract
Hypertension is a major contributor to the global disease burden, affecting more than one billion individuals worldwide. Despite decades of recognition of its adverse health effects, hypertension control rates remain suboptimal. Epidemiology provides essential knowledge for understanding disease distribution and identifying risk factors at the individual, social, and environmental levels. Recent evidence emphasizes both traditional lifestyle determinants, including excess sodium intake, low potassium intake, obesity, physical inactivity, smoking, and alcohol consumption, and emerging contributors, such as gut microbiota dysregulation and infectious diseases. Among those, the urinary sodium-to-potassium ratio has gained attention as an important factor associated with hypertension risk. Additionally, social determinants of health, including socioeconomic disparities, neighborhood deprivation, and structural racism, exacerbate the risk of hypertension and impede its effective control. Environmental factors such as air pollution, extreme temperatures, and occupational stress further contribute to the complexity of hypertension epidemiology. Regarding contemporary epidemiological methodology, our proposed concepts of the “Bench and Real-World Cycle” and “Real-World Evidence Cycle” highlight the necessity of continuously integrating real-world evidence into practice. In addition to classical cohort studies, real-world data derived from electronic health records including health checkups and insurance claims data are indispensable tools for addressing previous research limitations. This multifaceted perspective will accelerate evidence-based epidemiological approaches for preventing and treating hypertension.

Similar content being viewed by others
Introduction
Hypertension is a major contributor to the global disease burden [1]. The number of patients with hypertension continues to increase because of an aging population, particularly in developed countries. Although the adverse effects of hypertension on the global burden of disease have been recognized for decades [2], hypertension remains a crucial target for improving public health. Accordingly, multiple regional and international guidelines have been developed worldwide to address this challenge [3,4,5,6,7,8]. In these guidelines, epidemiology provides the fundamental knowledge needed to understand hypertension and describe its distribution. This mini-review introduces the latest epidemiological evidence and proposes new concepts for utilizing real-world data to develop contemporary epidemiological approaches for future countermeasures.
Hypertension statistics and burden
Globally, hypertension affected ~648 million people aged 30–79 years in 1990 and increased to 1.28 billion by 2019, suggesting that approximately one-third of adults have hypertension [9]. If current trends continue, the global burden is projected to reach ~1.5 billion people by 2030 and 2.0 billion people by 2050. In Japan, the number of adults with hypertension is estimated to be 43 million [10, 11], implying that nearly half of Japanese adults have hypertension. These estimations were based on blood pressure (BP) ≥ 140/ ≥ 90 mmHg as the definition for both hypertension diagnosis and BP control targets [9,10,11]. Meanwhile, lower BP cutoff points are gaining attention, as illustrated in the United States, where 130/80 mmHg serves as the diagnostic threshold for hypertension [4].
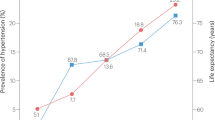
Reducing the risk for cardiovascular disease at lower BP levels will be a crucial challenge. A significantly increased risk of cardiovascular disease has been observed even in individuals with elevated BP (systolic/diastolic BP of 130–139/80–89 mmHg) in Japan [12,13,14]. According to the Evidence for Cardiovascular Prevention from Observational Cohorts in Japan (EPOCH-JAPAN), the population attributable fraction (PAF) of BP ≥ 130/80 mmHg for total cardiovascular disease mortality in patients without antihypertensive treatment was 38.6% [13]. A similar PAF estimation based on cardiovascular disease incidence was observed in another study conducted in Japan [14]. The Global Cardiovascular Risk Consortium recently reported that elevated BP and smoking are the two most influential modifiable risk factors for global longevity [15]. At an index age of 50 years, a systolic BP ≥ 130 mmHg shortened life expectancy in women and men by 1.7 and 1.8 years, respectively [15]. Moreover, it shortened the cardiovascular disease-free life expectancy by 1.3 and 1.8 years in women and men, respectively. Although the effect size appears modest compared to that of smoking or diabetes [15], the extremely high prevalence of elevated BP yields a profound population-level impact. Another estimate revealed that high systolic BP contributed to 10.85 million deaths in 2021 with the global population-attributable fraction of 15.99% [16]. Hypertension contributes to increased healthcare costs globally [17].
The relative cardiovascular risk due to high BP is more pronounced in younger populations [12,13,14]. However, because relatively short-term cardiovascular risks, such as 5- or 10-year risks, are very low in younger populations, healthcare providers sometimes have difficulty encouraging young individuals to modify their behavior. In this regard, lifetime risk estimates can be helpful tools because they represent the absolute risk during the remainder of one’s life [18]. Using lifetime risk estimation, we can provide young populations with high actual absolute risk estimates that they may face over their extended lifetimes [19,20,21].
Hypertension risk factors at the individual level
Traditional risk factors for hypertension include unhealthy alcohol consumption, smoking, physical inactivity, unhealthy dietary patterns, and obesity [3,4,5,6,7, 16]. Table 1 summarizes the lifestyle-related risk factors highlighted in recent hypertension guidelines [3,4,5,6,7]. As a representative unhealthy dietary pattern, high sodium and low potassium intake are key targets in promoting a population-based approach to combat high BP. In this context, urinary sodium-to-potassium ratio is now the focus because its measurement is more convenient than sodium or potassium measurements and is associated with BP [22,23,24,25,26,27,28]. Furthermore, the urinary sodium-to-potassium ratio is more strongly associated with home BP than with office BP [29] and is reportedly associated with cardiovascular diseases, including subclinical heart failure [22, 30,31,32]. This is supported by the results showing that salt substitutes with reduced sodium levels and increased potassium levels lowered BP and reduced the risk of cardiovascular disease and all-cause mortality compared to regular salt [33]. The influence of salt sensitivity should be considered when assessing the association between salt intake and hypertension. Asian population may exhibit greater salt sensitivity, potentially due to “relative aldosterone excess” reflected in the high aldosterone-to-renin ratio, often accompanied by a low-renin profile [34,35,36,37,38,39,40]. This may be supported by the fact that primary aldosteronism is a common form of secondary hypertension in Asia [41,42,43].
Accumulating evidence suggests that gut microbiota dysregulation may contribute to the pathogenesis of hypertension [44, 45]. A cross-sectional study of Hong Kong Chinese adults demonstrated that differences in gut microbiota composition and gut microbiota-associated short-chain fatty acid profiles were associated with hypertension in women but not in men [46]. This suggests that dysregulation of the gut microbiota contributes to the sex differences underlying the pathology of hypertension. Another study reported that resistant hypertension is characterized by decreased microbial diversity, elevated Actinobacteria levels, and distinct metabolomic profiles involving glycerophospholipid metabolism [47]. A Japanese study suggested that gut microbiome variability may influence the renin-angiotensin system through various pathways [48]. These findings suggest that the gut environment could be a candidate target for hypertension management. Bowel movements may be a confounding or mediating factor for these associations because a longitudinal study demonstrated that the absence of daily bowel movements was associated with elevated day-to-day BP variability [49].
Infectious diseases can lead to hypertension. A retrospective study reported that hospitalized Coronavirus Disease-2019 (COVID-19) patients had a 2.23 times and non-hospitalized COVID-19 patients had a 1.52 times higher risk for development of persistent hypertension than influenza counterparts [50]. A cross-sectional study of 19 survivors with severe COVID-19 observed significantly elevated muscle sympathetic nerve activity, arterial stiffness, and impaired endothelial function after discharge for COVID-19 [51].
Genetic factors are unmodifiable but crucial for predicting hypertension. Children can inherit a parental history of hypertension, which contributes to the development of high BP in adolescence [52]. The use of polygenic risk scores has been explored for prediction [53,54,55,56]. The Tohoku Medical Megabank Community-Based Cohort Study recently highlighted the predictive value of polygenic risk scores, which capture the cumulative burden of hypertension-associated genetic variants, even in adults without a family history of hypertension [57, 58].
Hypertension risk factors in the social and surrounding environment
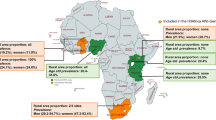
The “Social Determinants of Health (Rainbow Model)” by Dahlgren & Whitehead [59], along with the “Ecological Model” by McLeroy et al. [60], highlight that upstream factors such as socioeconomic conditions, social environment, and environment play a crucial role in the prevention and control of hypertension beyond individual lifestyle factors (Fig. 1).
Possible social determinants influencing hypertension: a multilevel perspective. This framework was adapted from the Dahlgren-Whitehead rainbow model of the social determinants of health [59]
The most concerning increases in hypertension prevalence have been observed in sub-Saharan Africa, Oceania, and South Asia, in contrast to the more stable trends in high-income regions [9]. However, various health disparities have been reported, even in high-income countries. A Japanese national database study of 127.8 million participants revealed significant income-related inequalities in hypertension prevalence (40.2%/48.6% vs. 21.5%/33.3% in low-income vs. high-income women/men, respectively), suggesting socioeconomic gradients according to income, even within a high-income country [61]. Racial/ethnic differences and neighborhood deprivation contribute to undiagnosed hypertension in multiethnic countries, such as the United States [62]. In the United States, social determinants mediated 33.0% of the black–white difference in uncontrolled BP, with low-income, low educational attainment, and disadvantaged neighborhoods being key contributors [63]. Racism is a direct determinant of hypertension risk. Interpersonal and structural racism have been associated with elevated postpartum BP [64]. The American Heart Association recognizes structural racism as a fundamental driver of cardiovascular health disparities [65].
The COVID-19 pandemic highlighted the interaction between social determinants and access to health systems during crises. During COVID-19-related social restrictions, BP elevations were observed [66, 67]. In addition, we reported that patients treated for hypertension refrained from regular medical visits due to lower household income during the 2020 social restrictions compared to higher-income patients (19.6% vs. 8.8%) [68]. These factors may be related to the recent real-world evidence indicating the association between COVID-19 and cardiovascular diseases [69].
Environmental changes can influence BP and cardiovascular disease risk in a wide range of populations. A multinational study of 567 cities across 27 countries, including Japan, reported that both extreme heat and cold (outside the 1st–99th percentiles) temperatures were significantly associated with increased cardiovascular mortality [70]. Air pollution is a significant risk factor for developing hypertension. Chinese studies have demonstrated that long-term exposure to particulate matter ≤2.5 μm (PM2.5) was associated with increased BP, with remarkable effects in individuals with baseline elevated BP [71], and that this association might be mediated through arachidonate metabolite pathways [72]. Traffic noise and air pollution reportedly increase cardiovascular risk through shared mechanisms, including sympathovagal imbalance, endothelial dysfunction, and vascular inflammation [73]. Exposure to volatile organic compounds contributes to the risk of hypertension [74, 75]. Environmental exposure appears to affect BP in the pediatric population [76].
Disasters are critical factors for hypertension. After the Great East Japan Earthquake in 2011, BP increased, partly due to subsequent lifestyle changes resulting from evacuation [77,78,79]. The association between volcanic smog and elevated BP has been suggested [80]. Furthermore, occupational stress also manifests as BP patterns. A BP reduction from weekdays to the weekend is greater in individuals with high job strain and high job demands [81]. Acute circadian misalignment due to work-related social jetlag can increase arterial stiffness and morning BP surge [82].
Epidemiology of hypertension control
Among women and men with hypertension in 2019 worldwide, 41% and 51% were estimated to be undiagnosed, 12% and 11% were diagnosed but untreated, and 24% and 20% were treated but uncontrolled, resulting in BP control rates of only 23% and 18%, respectively [9]. The situation appeared better in high-income Western and Asia-Pacific regions, where 27–34% of both women and men were undiagnosed, 10–14% were diagnosed but untreated, 21% were treated but uncontrolled, and the proportion of patients with controlled BP was 31–43%. The most concerning increases in the prevalence of hypertension were observed in sub-Saharan Africa, Oceania, and parts of South Asia, where BP control rates remain critically low.
Although Japan belongs to the high-income Asia-Pacific region and has a well-developed insurance system due to the Universal Health Insurance System, BP control in Japan seems to be suboptimal [9]. Among Japanese patients undergoing antihypertensive treatment, the proportion of patients with systolic/diastolic BP < 130/ < 80 mmHg was estimated to be 22.7–52.6% [83,84,85,86,87]. Our previous study reported that inadequate treatment and elevated pre-treatment BP levels were the two strongest factors for uncontrolled BP in Japan; 40.6% of cases with BP ≥ 140/ ≥ 90 mmHg and 25.6% of cases with BP ≥ 130/ ≥ 80 mmHg were due to failure to intensify antihypertensive medication to three or more agents [83]. These proportions could represent the quantifiable magnitude of “clinical inertia”, which refers to the failure of healthcare providers to initiate or intensify therapy despite unachieved therapeutic goals [88]. A Dutch cohort study identified BP levels closer to the target as factors associated with physicians being less likely to change antihypertensive therapy despite uncontrolled BP [89]. Furthermore, the recent report indicates that regional disparities in BP control exist even within Japan, revealing that healthcare resources significantly influence outcomes [90]. Even within a single country, comprehensive policy approaches encompassing the equitable distribution of healthcare resources may become crucial.
A hypertension-specialized clinic in Ohasama, where home BP was used to guide antihypertensive medication adjustment, achieved 93.6% home morning BP < 135/ < 85 mmHg between 2016 and 2019 [91]. Stroke incidence has shown a decreasing trend in Ohasama Town, Hanamaki City, Japan, where a community-based home BP monitoring program is ongoing as part of the Ohasama study [92]. These previous reports may provide an illustrative example of achieving target BP using home BP measurements [91, 92]. Also given that home BP measurements themselves can reduce BP [93,94,95,96], making home BP measurement devices more accessible would be beneficial. Further digitalization could be a key approach to achieving this, in part, through the development of wearable devices [97]. However, at present, healthcare providers should pay attention to the accuracy of BP measurement devices used by patients because unvalidated BP measurement devices are available for general consumers [98, 99]. A recent cross-sectional survey in Taiwan demonstrated that physicians identified device unreliability as a major barrier to the implementation of home BP measurement [100].
Medical teams, including non-physicians, are key factors in achieving good BP control [101]. A meta-analysis showed that pharmacist- and community health worker-led interventions produced the greatest BP reductions compared to physician-led interventions [102]. Another meta-analysis reported that multidisciplinary team-based care consistently outperformed usual care in controlling BP [103]. A large-scale Chinese cluster-randomized trial showed that when trained non-physician providers initiated and titrated antihypertensive medications following a stepped-care protocol under physician supervision, systolic/diastolic BP decreased by 23.1/9.9 mmHg, leading to a 33% reduction in the primary composite cardiovascular outcome [104].
Future directions of hypertension epidemiology using real-world data
Research using real-world data, i.e., routinely collected data in regular practice [105, 106], is growing in the field of hypertension epidemiology. In Japan, insurer-based databases that integrate annual health checkups and claims data have been widely used as real-world data [66, 83, 107]. It has provided real-world associations between BP levels and cardiovascular or kidney diseases [83, 108,109,110,111,112] and information on actual healthcare patterns as partly introduced above [101, 110, 113, 114]. Classical epidemiological approaches, represented by well-designed prospective cohort studies, are recognized as possible data sources contributing to real-world evidence [105, 106] and have the potential to enhance its scientific rigor through the provision of novel information.
Considering the broad availability of antihypertensive medications and BP measurements, real-world evidence will become increasingly important for advancing hypertension epidemiology and the social implementation of effective strategies to prevent and manage hypertension. Real-world evidence can be applied in practice, creating a feedback cycle back to the real world. Considering this, we propose the “Real-World Evidence Cycle” (Fig. 2), which will be a key concept describing the feedback cycle of usage patterns, effectiveness and safety information, and implementation feasibility from real-world data back to real-world practice. Additionally, the term “Bench to Bedside” has traditionally been used in translational research [115], but it could evolve into “Bench and Real-World Cycle” (Fig. 2).
Real-world centered research cycles in modern hypertension epidemiology evolution from the traditional bench-to-bedside approach to real-world research paradigms. The framework includes bidirectional “Bench and Real-World Cycle” and continuous “Real-World Evidence Cycle” for optimizing hypertension interventions in clinical practice
The Real-World Evidence Cycle is a framework centered on the concept of real-world evidence. It emphasizes the importance of evidence derived from real-world data and the necessity of applying that evidence back to real-world settings. In this cycle, both the sources and applications of knowledge exist in the real world, creating a continuous process of evidence generation, validation, and implementation. By accelerating this circulation, the relationships between exposure and outcomes can be clarified in near real time, allowing rapid refinement of prevention and management strategies. The rapid report of BP elevation during the COVID-19 pandemic in the Japanese population exemplifies the value of timely real-world evidence [66], providing crucial early warnings that inform public health responses in Japan [116]. In this context, Japan’s advantage lies in its universal health insurance system, which enables the integration of nationwide health check-up data with medical claims databases. This comprehensive coverage allows for the creation of population-wide Real-World Evidence Cycle across diverse Japanese communities. However, reducing the barriers to real-world data access is crucial for maximizing this potential. For example, the National Health and Nutrition Examination Survey (NHANES) in the United States and Clinical Practice Research Datalink (CPRD) in the United Kingdom have relatively low barriers to data access, enabling their widespread use by researchers globally and accelerating evidence generation.
The “Bench and Real-World Cycle” complement this framework by integrating laboratory and interventional research within the same real-world system. Evidence obtained from real-world data can generate new hypotheses for mechanistic or experimental studies (“real world to bench”), while findings from these studies can be re-evaluated and contextualized under real-world conditions (“bench to real world”). This concept also incorporates the reverse process, referred to as “bedside to bench.” The term “Real-World” is broader and more comprehensive than “Bedside,” because modern healthcare is not confined to traditional clinical settings. It encompasses situations such as medication use outside hospitals and clinics, as well as healthcare devices operated at home or in community environments. Furthermore, the Real-World Cycle and the Bench and Real-World Cycle are particularly valuable in contexts where randomized clinical trials are ethically or practically infeasible, for example, studies on medication discontinuation or treatment in vulnerable populations such as pregnant women. Ultimately, promoting these real-world concepts encourages researchers to recognize that evidence generation must be coupled with its application in practice beyond bedsides, thereby bridging the gap between scientific discovery and population health improvement. Regarding the evaluation of treatment, target trial emulation (TTE), as proposed by Hernán et al., is a useful design principle that uses observational data to mimic randomized trials using real-world data [117, 118].
Considering the increasing importance of the “Real-World Evidence Cycle,” improving the accuracy and validity of real-world data is also an important challenge [107]. For example, despite the existence of established guidelines, only a small proportion of Japanese health checkup organizations routinely perform BP measurements in accordance with the recommendations [119, 120]. In China, the real-world office systolic BP differs from the unobserved automated office systolic BP by +18 mmHg [121]. The proportion of patients with controlled BP varies according to the measurement time and season [122,123,124]. Furthermore, the electronic health records used to define outcomes in research studies are often inaccurate because clinicians register the disease name or code on claims to receive reimbursement, leading to biased risk estimates [107]. At present, these limitations should be carefully considered and transparently reported when using real-world data from electronic health records. Classical epidemiological studies that systematically collect validated information on exposure and outcomes are indispensable for strengthening real-world evidence. The integration of digital hypertension technologies could further accelerate evidence generation [99], particularly when combined with efforts toward data standardization and institutional collaboration. Furthermore, the use of generative artificial intelligence may enable rapid analysis of standardized BP data at unprecedented scales, potentially transforming future hypertension management.
Table 2 shows perspectives on hypertension epidemiology in Asian populations. Among Asian populations, BP exerts a particularly strong influence compared with other metabolic risk factors [125]. Given the aging population, the importance of hypertension management in Asian populations is expected to increase.
Conclusions
Hypertension is still a global public health challenge that requires immediate attention. Preventing hypertension effectively requires a comprehensive approach that addresses traditional individual-level risk factors, upstream social determinants, including socioeconomic disparities, environmental exposures, and structural racism, which profoundly influence hypertension. These considerations underscore the urgent need for innovative intervention strategies that extend beyond clinical settings and encompass community-based multidisciplinary approaches. Given this viewpoint, promoting a comprehensive “Bench and Real-World Cycle” and “Real-World Evidence Cycle” framework may become increasingly important in hypertension epidemiology. This will accelerate with the development of digital devices, including the evolution of home BP measurement devices and integration of electronic data. This will ultimately inform evidence-based policy decisions and optimize population-level interventions for this modifiable yet inadequately controlled cardiovascular risk factor.
References
GBD Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2162–203.
Lawes CM, Vander Hoorn S, Rodgers A. International Society of H. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Ohya Y, Sakima A, Arima H, Fukami A, Furuhashi M, Ishida M, et al. Key highlights of the Japanese Society of Hypertension Guidelines for the management of elevated blood pressure and hypertension 2025 (JSH2025). Hypertens Res. 2025;48:2500–11.
Jones DW, Ferdinand KC, Taler SJ, Johnson HM, Shimbo D, Abdalla M, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025;82:e212–316.
McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024;45:3912–4018.
Mancia G, Kreutz R, Brunstrom M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071.
Wang TD, Chiang CE, Chao TH, Cheng HM, Wu YW, Wu YJ, et al. 2022 Guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the Management of Hypertension. Acta Cardiol Sin. 2022;38:225–325.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Hisamatsu T, Miura K. Epidemiology and control of hypertension in Japan: a comparison with Western countries. J Hum Hypertens. 2024;38:469–76.
Hisamatsu T, Segawa H, Kadota A, Ohkubo T, Arima H, Miura K. Epidemiology of hypertension in Japan: beyond the new 2019 Japanese guidelines. Hypertens Res. 2020;43:1344–51.
Harada A, Ueshima H, Kinoshita Y, Miura K, Ohkubo T, Asayama K, et al. Absolute risk score for stroke, myocardial infarction, and all cardiovascular disease: Japan Arteriosclerosis Longitudinal Study. Hypertens Res. 2019;42:567–79.
Satoh M, Ohkubo T, Miura K, Harada A, Tsutsui A, Hozawa A, et al. Long-term risk of cardiovascular mortality according to age group and blood pressure categories of the latest guideline. Hypertens Res. 2025;48:1428–33.
Kuwahara K, Ohkubo T, Inoue Y, Honda T, Yamamoto S, Nakagawa T, et al. Blood pressure classification using the Japanese Society of Hypertension Guidelines for the Management of Hypertension and cardiovascular events among young to middle-aged working adults. Hypertens Res. 2024;47:1861–70.
Global Cardiovascular Risk C, Magnussen C, Alegre-Diaz J, Al-Nasser LA, Amouyel P, Aviles-Santa L, et al. Global Effect of Cardiovascular Risk Factors on Lifetime Estimates. N Engl J Med. 2025;393:125–38.
Martin SS, Aday AW, Allen NB, Almarzooq ZI, Anderson CAM, Arora P, et al. 2025 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2025;151:e41–e660.
Marques-Vidal P, Maung KK, Gouveia A. Twenty-year trends of potentially avoidable hospitalizations for hypertension in Switzerland. Hypertens Res. 2024;47:2847–54.
Beiser A, D’Agostino RB Sr, Seshadri S, Sullivan LM, Wolf PA. Computing estimates of incidence, including lifetime risk: Alzheimer’s disease in the Framingham Study. The Practical Incidence Estimators (PIE) macro. Stat Med. 2000;19:1495–522.
Satoh M, Ohkubo T, Asayama K, Murakami Y, Sugiyama D, Yamada M, et al. Lifetime Risk of Stroke and Coronary Heart Disease Deaths According to Blood Pressure Level: EPOCH-JAPAN (Evidence for Cardiovascular Prevention From Observational Cohorts in Japan). Hypertension. 2019;73:52–59.
Imai Y, Hirata T, Saitoh S, Ninomiya T, Miyamoto Y, Ohnishi H, et al. Impact of hypertension stratified by diabetes on the lifetime risk of cardiovascular disease mortality in Japan: a pooled analysis of data from the Evidence for Cardiovascular Prevention from Observational Cohorts in Japan study. Hypertens Res. 2020;43:1437–44.
Nakayama S, Satoh M, Metoki H, Murakami T, Asayama K, Hara A, et al. Lifetime risk of stroke stratified by chronic kidney disease and hypertension in the general Asian population: the Ohasama study. Hypertens Res. 2021;44:866–73.
Hisamatsu T, Kogure M, Tabara Y, Hozawa A, Sakima A, Tsuchihashi T, et al. Practical use and target value of urine sodium-to-potassium ratio in assessment of hypertension risk for Japanese: Consensus Statement by the Japanese Society of Hypertension Working Group on Urine Sodium-to-Potassium Ratio. Hypertens Res. 2024;47:3288–302.
Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 h urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988;297:319-28.
Perez V, Chang ET. Sodium-to-potassium ratio and blood pressure, hypertension, and related factors. Adv Nutr. 2014;5:712–41.
Hisamatsu T, Lloyd-Jones DM, Colangelo LA, Liu K. Urinary sodium and potassium excretions in young adulthood and blood pressure by middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. J Hypertens. 2021;39:1586–93.
Thi Minh Nguyen T, Miura K, Tanaka-Mizuno S, Tanaka T, Nakamura Y, Fujiyoshi A, et al. Association of blood pressure with estimates of 24-h urinary sodium and potassium excretion from repeated single-spot urine samples. Hypertens Res. 2019;42:411–8.
Tabara Y, Takahashi Y, Kumagai K, Setoh K, Kawaguchi T, Takahashi M, et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: the Nagahama study. J Hypertens. 2015;33:2407–13.
Stamler J, Chan Q, Daviglus ML, Dyer AR, Van Horn L, Garside DB, et al. Relation of Dietary Sodium (Salt) to Blood Pressure and Its Possible Modulation by Other Dietary Factors: The INTERMAP Study. Hypertension. 2018;71:631–7.
Muroya T, Satoh M, Murakami T, Nakayama S, Asayama K, Hirose T, et al. Association between urinary sodium-to-potassium ratio and home blood pressure and ambulatory blood pressure: the Ohasama study. J Hypertens. 2022;40:862–9.
Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrode KM, Kumanyika SK, et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med. 2009;169:32–40.
Muroya T, Satoh M, Metoki H, Nakayama S, Hirose T, Murakami T, et al. Association between urinary sodium-to-potassium ratio and BNP in a general population without antihypertensive treatment and cardiovascular diseases: the Ohasama study. Hypertens Res. 2025;48:2292–302.
Ma Y, He FJ, Sun Q, Yuan C, Kieneker LM, Curhan GC, et al. 24-Hour Urinary Sodium and Potassium Excretion and Cardiovascular Risk. N Engl J Med. 2022;386:252–63.
Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, et al. Effect of Salt Substitution on Cardiovascular Events and Death. N Engl J Med. 2021;385:1067–77.
Satoh M, Kikuya M, Hosaka M, Asayama K, Inoue R, Metoki H, et al. Association of aldosterone-to-renin ratio with hypertension differs by sodium intake: the Ohasama study. Am J Hypertens. 2015;28:208–15.
Satoh M, Kikuya M, Ohkubo T, Mori T, Metoki H, Hashimoto T, et al. Aldosterone-to-renin ratio and nocturnal blood pressure decline in a general population: the Ohasama study. J Hypertens. 2011;29:1940–7.
Satoh M, Kikuya M, Ohkubo T, Mori T, Metoki H, Hara A, et al. Aldosterone-to-renin ratio as a predictor of stroke under conditions of high sodium intake: the Ohasama study. Am J Hypertens. 2012;25:777–83.
Satoh M, Kikuya M, Ohkubo T, Imai Y. Role of angiotensinogen and relative aldosterone excess in salt-sensitive hypertension. Hypertension. 2012;59:e57.
Satoh M, Kikuya M, Ohkubo T, Imai Y. Role of relative aldosterone excess in salt-sensitive hypertension among African ancestry. Am J Hypertens. 2012;25:398–9.
Satoh M, Kikuya M, Hara A, Ohkubo T, Mori T, Metoki H, et al. Aldosterone-to-renin ratio and home blood pressure in subjects with higher and lower sodium intake: the Ohasama study. Hypertens Res. 2011;34:361–6.
Satoh M, Hosaka M, Asayama K, Kikuya M, Inoue R, Metoki H, et al. Aldosterone-to-renin ratio and nocturnal blood pressure decline assessed by self-measurement of blood pressure at home: the Ohasama Study. Clin Exp Hypertens. 2014;36:108–14.
Yoon M, Hong N, Ha J, Lee CJ, Ku CR, Rhee Y, et al. Prevalence and clinical characteristics of primary aldosteronism in a tertiary-care center in Korea. Hypertens Res. 2022;45:1418–29.
Ito Y, Takeda R, Karashima S, Yamamoto Y, Yoneda T, Takeda Y. Prevalence of primary aldosteronism among prehypertensive and stage 1 hypertensive subjects. Hypertens Res. 2011;34:98–102.
Xu Z, Yang J, Hu J, Song Y, He W, Luo T, et al. Primary Aldosteronism in Patients in China With Recently Detected Hypertension. J Am Coll Cardiol. 2020;75:1913–22.
Durgan DJ, Zubcevic J, Vijay-Kumar M, Yang T, Manandhar I, Aryal S, et al. Prospects for Leveraging the Microbiota as Medicine for Hypertension. Hypertension. 2024;81:951–63.
Xu C, Marques FZ. How Dietary Fibre, Acting via the Gut Microbiome, Lowers Blood Pressure. Curr Hypertens Rep. 2022;24:509–21.
Virwani PD, Qian G, Hsu MSS, Pijarnvanit T, Cheung CN, Chow YH, et al. Sex Differences in Association Between Gut Microbiome and Essential Hypertension Based on Ambulatory Blood Pressure Monitoring. Hypertension. 2023;80:1331–42.
Guo J, Jia P, Gu Z, Tang W, Wang A, Sun Y, et al. Altered gut microbiota and metabolite profiles provide clues in understanding resistant hypertension. J Hypertens. 2024;42:1212–25.
Mizoguchi R, Karashima S, Miyajima Y, Ogura K, Kometani M, Aono D, et al. Impact of gut microbiome on the renin-aldosterone system: Shika-machi Super Preventive Health Examination results. Hypertens Res. 2023;46:2280–92.
Kubozono T, Akasaki Y, Kawasoe S, Ojima S, Yamaguchi S, Kuwahata S, et al. Relationship between defecation status and blood pressure level or blood pressure variability. Hypertens Res. 2024;47:128–36.
Zhang V, Fisher M, Hou W, Zhang L, Duong TQ. Incidence of New-Onset Hypertension Post-COVID-19: Comparison With Influenza. Hypertension. 2023;80:2135–48.
Faria D, Moll-Bernardes RJ, Testa L, Moniz CMV, Rodrigues EC, Rodrigues AG, et al. Sympathetic Neural Overdrive, Aortic Stiffening, Endothelial Dysfunction, and Impaired Exercise Capacity in Severe COVID-19 Survivors: A Mid-Term Study of Cardiovascular Sequelae. Hypertension. 2023;80:470–81.
Park HK, Shim YS. Hypertension prevalence in Korean adolescents according to parental hypertension: data from the Korea National Health and Nutrition Survey. Hypertens Res. 2025;48:1003–11.
Pazoki R, Dehghan A, Evangelou E, Warren H, Gao H, Caulfield M, et al. Genetic Predisposition to High Blood Pressure and Lifestyle Factors: Associations With Midlife Blood Pressure Levels and Cardiovascular Events. Circulation. 2018;137:653–61.
Said MA, Verweij N, van der Harst P. Associations of Combined Genetic and Lifestyle Risks With Incident Cardiovascular Disease and Diabetes in the UK Biobank Study. JAMA Cardiol. 2018;3:693–702.
Vaura F, Kauko A, Suvila K, Havulinna AS, Mars N, Salomaa V, et al. Polygenic Risk Scores Predict Hypertension Onset and Cardiovascular Risk. Hypertension. 2021;77:1119–27.
Kurniansyah N, Goodman MO, Kelly TN, Elfassy T, Wiggins KL, Bis JC, et al. A multi-ethnic polygenic risk score is associated with hypertension prevalence and progression throughout adulthood. Nat Commun. 2022;13:3549.
Takase M, Hirata T, Nakaya N, Kogure M, Hatanaka R, Nakaya K, et al. Associations of family history of hypertension, genetic, and lifestyle risks with incident hypertension. Hypertens Res. 2025;48:2606–17.
Takase M, Hirata T, Nakaya N, Nakamura T, Kogure M, Hatanaka R, et al. Associations of combined genetic and lifestyle risks with hypertension and home hypertension. Hypertens Res. 2024;47:2064–74.
Dahlgren G, Whitehead M. The Dahlgren-Whitehead model of health determinants: 30 years on and still chasing rainbows. Public Health. 2021;199:20–24.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77.
Aida J, Inoue Y, Tabuchi T, Kondo N. Modifiable risk factors of inequalities in hypertension: analysis of 100 million health checkups recipients. Hypertens Res. 2024;47:1555–66.
Rivier CA, Renedo DB, Sunmonu NA, de Havenon A, Sheth KN, Falcone GJ. Neighborhood Deprivation, Race, Ethnicity, and Undiagnosed Hypertension: Results From the All of Us Research Program. Hypertension. 2024;81:e10–e12.
Akinyelure OP, Jaeger BC, Oparil S, Carson AP, Safford MM, Howard G, et al. Social Determinants of Health and Uncontrolled Blood Pressure in a National Cohort of Black and White US Adults: the REGARDS Study. Hypertension. 2023;80:1403–13.
Janevic T, Howell FM, Burdick M, Nowlin S, Maru S, Boychuk N, et al. Racism and Postpartum Blood Pressure in a Multiethnic Prospective Cohort. Hypertension. 2025;82:206–15.
Albert MA, Churchwell K, Desai N, Johnson JC, Johnson MN, Khera A, et al. Addressing Structural Racism Through Public Policy Advocacy: A Policy Statement From the American Heart Association. Circulation. 2024;149:e312–29.
Satoh M, Murakami T, Obara T, Metoki H. Time-series analysis of blood pressure changes after the guideline update in 2019 and the coronavirus disease pandemic in 2020 using Japanese longitudinal data. Hypertens Res. 2022;45:1408–17.
Laffin LJ, Kaufman HW, Chen Z, Niles JK, Arellano AR, Bare LA, et al. Rise in Blood Pressure Observed Among US Adults During the COVID-19 Pandemic. Circulation. 2022;145:235–7.
Toyama M, Satoh M, Hashimoto H, Iwabe Y, Yagihashi T, Nakayama S, et al. Association between equivalized annual household income and regular medical visits for hypertensive patients since the COVID-19 outbreak. Hypertens Res. 2025;48:786–95.
Lee S, Hwang SH, Park S, Son Y, Kim S, Kim HJ, et al. Burden of Cardiovascular Outcomes After SARS-CoV-2 Infection in South Korea and Japan: A Binational Population-Based Cohort Study. Circulation. 2025;152:11–23.
Alahmad B, Khraishah H, Roye D, Vicedo-Cabrera AM, Guo Y, Papatheodorou SI, et al. Associations Between Extreme Temperatures and Cardiovascular Cause-Specific Mortality: Results From 27 Countries. Circulation. 2023;147:35–46.
Dong S, Yu B, Yin C, Li Y, Zhong W, Feng C, et al. Associations between PM 2.5 and its chemical constituents and blood pressure: a cross-sectional study. J Hypertens. 2024;42:1897–905.
Wang T, Han Y, Chen X, Chen W, Li H, Wang Y, et al. Particulate Air Pollution and Blood Pressure: Signaling by the Arachidonate Metabolism. Hypertension. 2023;80:2687–96.
Hahad O, Rajagopalan S, Lelieveld J, Sorensen M, Kuntic M, Daiber A, et al. Noise and Air Pollution as Risk Factors for Hypertension: Part II-Pathophysiologic Insight. Hypertension. 2023;80:1384–92.
Zheng X, Zou P, Zeng C, Liu J, He Y. Increased levels of urine volatile organic compounds are associated with hypertension risk. J Hypertens. 2025;43:136–44.
McGraw KE, Domingo-Relloso A, Riggs DW, Medgyesi DN, Neupane R, Stingone JA, et al. Exposure to Volatile Organic Compounds and Blood Pressure in NHANES 2011 to 2018. Hypertension. 2025;82:136–48.
Zachariah JP, Jone PN, Agbaje AO, Ryan HH, Trasande L, Perng W, et al. Environmental Exposures and Pediatric Cardiology: A Scientific Statement From the American Heart Association. Circulation. 2024;149:e1165–75.
Satoh M, Kikuya M, Ohkubo T, Imai Y. Acute and subacute effects of the great East Japan earthquake on home blood pressure values. Hypertension. 2011;58:e193–4.
Nishizawa M, Hoshide S, Okawara Y, Shimpo M, Matsuo T, Kario K. Aftershock Triggers Augmented Pressor Effects in Survivors: Follow-Up of the Great East Japan Earthquake. Am J Hypertens. 2015;28:1405–8.
Ohira T, Hosoya M, Yasumura S, Satoh H, Suzuki H, Sakai A, et al. Evacuation and Risk of Hypertension After the Great East Japan Earthquake: The Fukushima Health Management Survey. Hypertension. 2016;68:558–64.
Brook RD, Brook JR, Tam EK. Volcanic smog and cardiometabolic health: Hawaiian hypertension?. J Clin Hypertens. 2019;21:533–5.
Karelius S, Pentti J, Juhanoja E, Jula A, Koskinen S, Niiranen TJ, et al. Association of work-related psychosocial factors and day-to-day home blood pressure variation: the Finn-Home study. J Hypertens. 2024;42:337–43.
Nakamura N, Akiyama H, Nishimura M, Zhu K, Suzuki K, Higuchi M, et al. Acute social jetlag augments morning blood pressure surge: a randomized crossover trial. Hypertens Res. 2023;46:2179–91.
Satoh M, Muroya T, Murakami T, Obara T, Asayama K, Ohkubo T, et al. The impact of clinical inertia on uncontrolled blood pressure in treated hypertension: real-world, longitudinal data from Japan. Hypertens Res. 2024;47:598–607.
Fujishima S, Kodama S, Tsuchihashi T. Achievement rate of blood pressure <140/90 mmHg and <130/80 mmHg in subjects with hypertension; findings from a Japanese health checkup in 2017. Clin Exp Hypertens. 2020;42:648–55.
Yokokawa H, Suzuki M, Aoki N, Sato Y, Naito T. Achievement of target blood pressure among community residents with hypertension and factors associated with therapeutic failure in the northern territory of Japan. J Int Med Res. 2022;50:3000605221126878.
Ohno K, Takase H, Sugiura T, Machii M, Nonaka D, Tokumaru M, et al. Current status and recent changes in blood pressure and dietary salt consumption in Japanese individuals. Clin Exp Hypertens. 2021;43:287–94.
Sakima A, Yamazato M, Kohagura K, Ishida A, Matayoshi T, Tana T, et al. Achievement rate of target blood pressure in patients with hypertension treated by hypertension specialists and non-specialists in a real-world setting. Hypertens Res. 2023;46:2460–9.
Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34.
Ali DH, Kilic B, Hart HE, Bots ML, Biermans MCJ, Spiering W, et al. Therapeutic inertia in the management of hypertension in primary care. J Hypertens. 2021;39:1238–45.
Iwabe Y, Satoh M, Nobayashi H, Izumi S, Murakami T, Toyama M, et al. Regional disparities in blood pressure control after hypertension treatment initiation in Japan: a real-world data analysis. Hypertens Res. 2025; https://doi.org/10.1038/s41440-025-02454-y.
Satoh M, Metoki H, Murakami T, Tatsumi Y, Asayama K, Kikuya M, et al. Home blood pressure control and prescribing patterns of anti-hypertensive medications in a home blood pressure-based hypertension-specialized clinic in Japan: a sub-analysis of the Ohasama study. Hypertens Res. 2025;48:26–36.
Imai Y. A personal history of research on hypertension From an encounter with hypertension to the development of hypertension practice based on out-of-clinic blood pressure measurements. Hypertens Res. 2022;45:1726–42.
Satoh M, Tatsumi Y, Nakayama S, Shinohara Y, Kawazoe M, Nozato Y, et al. Self-measurement of blood pressure at home using a cuff device for change in blood pressure levels: systematic review and meta-analysis. Hypertens Res. 2025;48:574–91.
Hozawa A, Shimazu T, Kuriyama S, Tsuji I. Benefit of home blood pressure measurement after a finding of high blood pressure at a community screening. J Hypertens. 2006;24:1265–71.
Sheppard JP, Tucker KL, Davison WJ, Stevens R, Aekplakorn W, Bosworth HB, et al. Self-monitoring of Blood Pressure in Patients With Hypertension-Related Multi-morbidity: Systematic Review and Individual Patient Data Meta-analysis. Am J Hypertens. 2020;33:243–51.
McManus RJ, Little P, Stuart B, Morton K, Raftery J, Kelly J, et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ. 2021;372:m4858.
Kario K, Williams B, Tomitani N, McManus RJ, Schutte AE, Avolio A, et al. Innovations in blood pressure measurement and reporting technology: International Society of Hypertension position paper endorsed by the World Hypertension League, European Society of Hypertension, Asian Pacific Society of Hypertension, and Latin American Society of Hypertension. J Hypertens. 2024;42:1874–88.
Picone DS, Campbell NRC, Schutte AE, Olsen MH, Ordunez P, Whelton PK, et al. Validation Status of Blood Pressure Measuring Devices Sold Globally. JAMA. 2022;327:680–1.
Kario K, Asayama K, Arima H, Matsumoto C, Nakagawa N, Nomura A, et al. Digital hypertension – what we need for the high-quality management of hypertension in the new era. Hypertns Res. 2025;48:3130–46.
Lin YS, Lin HJ, Wang TD. Physicians’ knowledge, awareness and instructions of home blood pressure monitoring: Asia HBPM survey in Taiwan. Hypertens Res. 2025;48:60–7.
Satoh M. Understanding clinical inertia in hypertension management: clues from real-world data. Hypertens Res. 2025;48:3046–8.
Mills KT, O’Connell SS, Pan M, Obst KM, He H, He J. Role of Health Care Professionals in the Success of Blood Pressure Control Interventions in Patients With Hypertension: A Meta-Analysis. Circ Cardiovasc Qual Outcomes. 2024;17:e010396.
Akasaki Y, Suematsu Y, Azushima K, Shiga Y, Sakima A, Satoh M, et al. Impact of patient care teams on blood pressure control in patients with hypertension: a systematic review and meta-analysis. Hypertens Res. 2025;48:1827–38.
He J, Ouyang N, Guo X, Sun G, Li Z, Mu J, et al. Effectiveness of a non-physician community health-care provider-led intensive blood pressure intervention versus usual care on cardiovascular disease (CRHCP): an open-label, blinded-endpoint, cluster-randomised trial. Lancet. 2023;401:928–38.
Food and Drug Administration (United States). Framework for FDA’S Real-world Evidence Program. 2018. https://www.fda.gov/media/120060/download. Accessed 05/Jan/2026.
National Institute for Health and Clinical Excellence (United Kingdom). NICE real-world evidence framework, Corporate document Reference number:ECD9. 2022. https://www.nice.org.uk/corporate/ecd9/chapter/methods-for-real-world-studies-of-comparative-effects. Accessed 05/Jan/2026.
Satoh M, Nakayama S, Toyama M, Hashimoto H, Murakami T, Metoki H. Usefulness and caveats of real-world data for research on hypertension and its association with cardiovascular or renal disease in Japan. Hypertens Res. 2024;47:3099–113.
Satoh M, Nakayama S, Hashimoto H, Toyama M, Iwabe Y, Yagihashi T, et al. Differential coronary heart disease risk among antihypertensive and lipid-lowering medication users versus non-users: A real-world data analysis. J Clin Lipido. 2025;19:294–302.
Suenaga T, Satoh M, Murakami T, Hirose T, Obara T, Nakayama S, et al. Cross-classification by systolic and diastolic blood pressure levels and chronic kidney disease, proteinuria, or kidney function decline. Hypertens Res. 2023;46:1860–9.
Kitaoka K, Kaneko H, Suzuki Y, Okada A, Mizuno A, Fujiu K, et al. Blood pressure control and treatment status at 1 year after the first health check-up in individuals with observed referral-level blood pressure. Hypertens Res. 2025;48:2537–47.
Mori Y, Mizuno A, Fukuma S. Low on-treatment blood pressure and cardiovascular events in patients without elevated risk: a nationwide cohort study. Hypertens Res. 2024;47:1546–54.
Tabara Y, Shoji-Asahina A, Ogawa A, Sato Y. Additive association of blood pressure and short stature with stroke incidence in 450,000 Japanese adults: the Shizuoka study. Hypertens Res. 2024;47:2075–85.
Ito H, Seki T, Kawazoe Y, Takiguchi T, Akagi Y, Kubota K, et al. Prognostic impact of the timing of antihypertensive medication initiation for hypertension detected at health screening on primary prevention of adverse cardiovascular events: Age-stratified real-world data analysis. Hypertens Res. 2025;48:2401-12.
Satoh M, Nobayashi H, Iwabe Y. Delayed treatment initiation as one of the crucial factors in clinical inertia: lessons from a real-world database research. Hypertens Res. 2025;48:2732–4.
McKinney GR, Stavely HE. From Bench to Bedside: The Biologist in Drug Development. BioScience. 1966;16:683–7.
Shibata S, Kobayashi K, Tanaka M, Asayama K, Yamamoto E, Nakagami H, et al. COVID-19 pandemic and hypertension: an updated report from the Japanese Society of Hypertension project team on COVID-19. Hypertens Res. 2023;46:589–600.
Hernan MA, Wang W, Leaf DE. Target Trial Emulation: A Framework for Causal Inference From Observational Data. JAMA. 2022;328:2446–7.
Hernan MA, Robins JM. Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available. Am J Epidemiol. 2016;183:758–64.
Watanabe T, Satoh H, Sugawara Y, Tsukita Y, Goto T, Kikuchi A. The Current State of Blood Pressure Measurement in Medical Examination Institutions —A Study Based on Questionnaire Replies. Health Eval Promot. 2020;47:463–8.
Kobayashi K, Hatori N, Sakai H, Furuki T, Miyakawa M, Tamura K, et al. Comparison of questionnaire responses regarding awareness of Japanese Society of Hypertension guidelines for the management of hypertension between 2014 and 2019 in primary care. Hypertens Res. 2021;44:1147–57.
Chapman N, Jayasinghe S, Moore MN, Picone DS, Schultz MG, Jose MD, et al. Absolute cardiovascular risk assessment using ‘real world’ clinic blood pressures compared to standardized unobserved and ambulatory methods: an observational study. Hypertens Res. 2024;47:2855–63.
Yan Q, Cheng M, Xu W, Cheng Y, Wu F, Wang Y, et al. The control rate of hypertension across months of year and hours of day in a large real-world database. Hypertens Res. 2024;47:2981–8.
Hanazawa T, Asayama K, Watabe D, Tanabe A, Satoh M, Inoue R, et al. Association Between Amplitude of Seasonal Variation in Self-Measured Home Blood Pressure and Cardiovascular Outcomes: HOMED-BP (Hypertension Objective Treatment Based on Measurement By Electrical Devices of Blood Pressure) Study. J Am Heart Assoc. 2018;7:e008509.
Hanazawa T, Asayama K, Watabe D, Hosaka M, Satoh M, Yasui D, et al. Seasonal variation in self-measured home blood pressure among patients on antihypertensive medications: HOMED-BP study. Hypertens Res. 2017;40:284–90.
Liu L, Miura K, Fujiyoshi A, Kadota A, Miyagawa N, Nakamura Y, et al. Impact of metabolic syndrome on the risk of cardiovascular disease mortality in the United States and in Japan. Am J Cardiol. 2014;113:84–89.
Acknowledgements
The manuscript was comprehensively edited by Editage (Cactus Communications). Additional language refinement was performed using DeepL, Claude, Grammarly, and ChatGPT software. We thank all the staff who supported us in the preparation of this review.
Funding
This study was supported by Grants for Scientific Research (KAKENHI) (JP25K02854) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; academic support from Bayer Yakuhin Co., Ltd.; a grant from the Daiwa Securities Foundation; a grant from the Kowa Life Science Foundation; and the Medical Research Encouragement Prize of the Japan Medical Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MS received academic support from Bayer Yakuhin Co., Ltd., and a grant from the Kowa Life Science Foundation funded by Kowa Co., Ltd. HM concurrently holds the position of Director of the Tohoku Institute for the Management of Blood Pressure, supported by Omron Healthcare Co., Ltd. We previously obtained access to the databases of the Japan Health Insurance Association (JHIA), JMDC Inc., and DeSC Healthcare, Inc.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Satoh, M., Nakayama, S., Nobayashi, H. et al. Current hypertension epidemiology and contemporary approaches using the “Real-World Evidence Cycle” framework. Hypertens Res (2026). https://doi.org/10.1038/s41440-025-02532-1
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41440-025-02532-1