Abstract
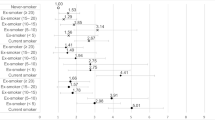
Smoking has negative reproductive consequences. This study investigated the effect of smoking cessation on the main semen parameters. We included 90 participants who applied to our infertility clinic and smoked at least 20 cigarettes a day for at least 1 year. Of the 90 participants, 48 were in the study group and 42 were in the control group. Semen analysis was performed before and at least 3 months after quitting smoking in the study group. Semen analysis was repeated at baseline and at least 3 months later in the control group. Semen parameters such as volume, sperm concentration, total sperm count, morphology, and motility were evaluated according to the World Health Organization criteria. Patient characteristics as well as the duration of the smoking period, the number of cigarettes smoked per day and the time elapsed since smoking cessation were recorded. The mean age of the participants was 34.69 ± 5.3 years, and the duration of infertility was 34.12 ± 12.1 months (n = 90). The number of cigarettes smoked per day was 30.14 ± 6.69, and the smoking time was 8.31 ± 3.53 years. The average time to quit smoking was 104.2 ± 11.51 days (n = 48). A significant increase in semen volume, sperm concentration and total sperm count was observed 3 months after smoking cessation (2.48 ± 0.79 ml vs. 2.90 ± 0.77 ml, p = 0.002; 18.45 × 106/ml ± 8.56 vs. 22.64 × 106/ml ± 11.69, p = 0.001; 45.04 ± 24.38 × 106 vs. 65.1 ± 34.9 × 106, p < 0.001, respectively). This study showed that smoking cessation had a positive effect on sperm concentration, semen volume, and total sperm count. Although smoking cessation contributed positively to sperm motility and morphology, the difference was not statistically significant.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Data availability
The data that support the findings of this study are available from the corresponding author (TT) upon reasonable request.
References
World Health Organisation (2019) WHO global report on trends in prevalence of tobacco use third edition.
Penzias A, Bendikson K, Butts S, Coutifaris C, Falcone T, Gitlin S, et al. Smoking and infertility: a committee opinion. Fertil Steril. 2018;110:611–8.
Caruso RV, O’Connor RJ, Stephens WE, Cummings KM, Fong GT. Toxic metal concentrations in cigarettes obtained from U.S. smokers in 2009: Results from the International Tobacco Control (ITC) United States survey cohort. Int J Environ Res Public Health. 2013;11:202–17.
Richter P, Pechacek T, Swahn M, Wagman V. Reducing levels of toxic chemicals in cigarette smoke: A new healthy people 2010 objective. Public Health Rep. 2008;123:30–38.
Kovac JR, Khanna A, Lipshultz LI. The effects of cigarette smoking on male fertility. Postgrad Med. 2015;127:338–41.
Dai J-B, Wang Z-X, Qiao Z-D. The hazardous effects of tobacco smoking on male fertility. Asian J Androl. 2015;17:954.
Rehman R, Zahid N, Amjad S, Baig M, Gazzaz ZJ. Relationship between smoking habit and sperm parameters among patients attending an infertility clinic. Front Physiol. 2019. https://doi.org/10.3389/fphys.2019.01356.
Alahmar A. Role of oxidative stress in male infertility: An updated review. J Hum Reprod Sci. 2019;12:4.
Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ. Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Fertil Steril. 2002;78:491–9.
Agarwal A, Virk G, Ong C, du Plessis SS. Effect of oxidative stress on male reproduction. World J Mens Health. 2014;32:1.
Jenkins TG, James ER, Alonso DF, Hoidal JR, Murphy PJ, Hotaling JM, et al. Cigarette smoking significantly alters sperm DNA methylation patterns. Andrology. 2017;5:1089–99.
Hwang K, Walters RC, Lipshultz LI. Contemporary concepts in the evaluation and management of male infertility. Nat Rev Urol. 2011;8:86–94.
Bundhun PK, Janoo G, Bhurtu A, Teeluck AR, Soogund MZS, Pursun M, et al. Tobacco smoking and semen quality in infertile males: a systematic review and meta-analysis. BMC Public Health. 2019;19:36.
De Brucker S, Drakopoulos P, Dhooghe E, De Geeter J, Uvin V, Santos-Ribeiro S, et al. The effect of cigarette smoking on the semen parameters of infertile men. Gynecol Endocrinol. 2020;36:1127–30.
Sharma R, Harlev A, Agarwal A, Esteves SC. Cigarette smoking and semen quality: a new meta-analysis examining the effect of the 2010 World Health Organization laboratory methods for the examination of human semen. Eur Urol. 2016;70:635–45.
Prentki Santos E, López-Costa S, Chenlo P, Pugliese MN, Curi S, Ariagno J, et al. Impact of spontaneous smoking cessation on sperm quality: case report. Andrologia. 2011;43:431–5.
World Bank Prevalence of current tobacco use, males. https://data.worldbank.org/indicator/SH.PRV.SMOK.MA?locations=TR. Accessed 9 Jun 2022.
Öztekin Ü, Caniklioğlu M, Sarı S, Selmi V, Gürel A, Işıkay L. Evaluation of male infertility prevalence with clinical outcomes in middle anatolian region. Cureus. 2019. https://doi.org/10.7759/cureus.5122.
World Bank Population ages 15–64, male. https://data.worldbank.org/indicator/SP.POP.1564.MA.IN?locations=TR. Accessed 9 Jun 2022.
Eisenberg ML, Li S, Behr B, Pera RR, Cullen MR. Relationship between semen production and medical comorbidity. Fertil Steril. 2015;103:66–71.
Guo D, Li S, Behr B, Eisenberg ML. Hypertension and male fertility. World J Mens Health. 2017;35:59.
Griswold MD. Spermatogenesis: the commitment to meiosis. Physiol Rev. 2016;96:1–17.
Fukuda T, Miyake H, Enatsu N, Matsushita K, Fujisawa M. Assessment of time-dependent changes in semen parameters in infertile men after microsurgical varicocelectomy. Urology. 2015;86:48–51.
Al Bakri A, Lo K, Grober E, Cassidy D, Cardoso JP, Jarvi K. Time for improvement in semen parameters after varicocelectomy. J Urol. 2012;187:227–31.
Ghaed MA, Makian SA, Moradi A, Maghsoudi R, Gandomi-Mohammadabadi A. Best time to wait for the improvement of the sperm parameter after varicocelectomy: 3 or 6 months? Arch Ital di Urol e Androl. 2020. https://doi.org/10.4081/aiua.2020.3.259.
Kızılay F, Altay B. Evaluation of the effects of antioxidant treatment on sperm parameters and pregnancy rates in infertile patients after varicocelectomy: a randomized controlled trial. Int J Impot Res. 2019;31:424–31.
WHO (2021) World Health Organization. WHO laboratory manual for the examination and processing of human semen. 6th ed. World Health Organization, Department of Reproductive Health and Research. Geneva, Switzerland.
Bonnie RJ, Stratton K, Kwan LY. Public health implications of raising the minimum age of legal access to tobacco products. Public Heal Implic Rais Minim Age Leg Access to Tob Prod. 2015. https://doi.org/10.17226/18997.
Harlev A, Agarwal A, Gunes SO, Shetty A, du Plessis SS. Smoking and male infertility: an evidence-based review. World J Mens Health. 2015;33:143.
Asare-Anane H, Bannison SB, Ofori EK, Ateko RO, Bawah AT, Amanquah SD, et al. Tobacco smoking is associated with decreased semen quality. Reprod Health. 2016;13:90.
Ozgur K, Isikoglu M, Seleker M, Donmez L. Semen quality of smoking and non-smoking men in infertile couples in a Turkish population. Arch Gynecol Obstet. 2005;271:109–12.
Zinaman MJ, Brown CC, Selevan SG, Clegg ED. Semen quality and human fertility: a prospective study with healthy couples. J Androl. 2000;21:145–53.
Rahimi-Madiseh M, Mohammadi M, Hassanvand A, Ahmadi R, Shahmohammadi M, Rostamzadeh A. Assessment of the toxicity effects of nicotine on sperm and IVF and the potential protective role of silymarin—an experimental study in mice. Middle East Fertil Soc J. 2020. https://doi.org/10.1186/s43043-020-00025-4.
Elshal MF, El-Sayed IH, Elsaied MA, El-Masry SA, Kumosani TA. Sperm head defects and disturbances in spermatozoal chromatin and DNA integrities in idiopathic infertile subjects: Association with cigarette smoking. Clin Biochem. 2009;42:589–94.
Ranganathan P, Rao KA, Thalaivarasai Balasundaram S. Deterioration of semen quality and sperm‐DNA integrity as influenced by cigarette smoking in fertile and infertile human male smokers—A prospective study. J Cell Biochem. 2019;120:11784–93.
Trummer H, Habermann H, Haas J, Pummer K. The impact of cigarette smoking on human semen parameters and hormones. Hum Reprod. 2002;17:1554–9.
Vanegas JC, Chavarro JE, Williams PL, Ford JB, Toth TL, Hauser R, et al. Discrete survival model analysis of a couple’s smoking pattern and outcomes of assisted reproduction. Fertil Res Pr. 2017;3:5.
Tang Q, Pan F, Wu X, Nichols CE, Wang X, Xia Y, et al. Semen quality and cigarette smoking in a cohort of healthy fertile men. Environ Epidemiol. 2019;3:e055.
Oyeyipo IP, Raji Y, Emikpe BO, Bolarinwa AF. Effects of nicotine on sperm characteristics and fertility profile in adult male rats: a possible role of cessation. J Reprod Infertil. 2011;12:201–7.
Pacifici R, Altieri I, Gandini L, Lenzi A, Pichini S, Rosa M, et al. Nicotine, Cotinine, and trans-3-Hydroxycotine Levels in Seminal Plasma of Smokers. Ther Drug Monit. 1993;15:358–63.
Gorber SC, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M. The accuracy of self-reported smoking: A systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009;11:12–24.
Soulakova JN, Hartman AM, Liu B, Willis GB, Augustine S. Reliability of adult self-reported smoking history: data from the tobacco use supplement to the current population survey 2002–2003 cohort. Nicotine Tob Res. 2012;14:952–60.
Minhas S, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. European association of urology guidelines on male sexual and reproductive health: 2021 update on male infertility. Eur Urol. 2021;80:603–20.
Author information
Authors and Affiliations
Contributions
Conceptualization, statistical analysis, writing—original draft, writing—review and editing: DK, TT, ET, MY, MAR. Conceptualization, investigation, data curation, resources: TT, MY, MAR, AG, MS Conceptualization, formal analysis, review: AG, MS. Paper editing, review: DK, EA, RBD, MG, AV Supervision: MG, AV. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Fatih Sultan Mehmet Training and Research Hospital Clinical Research Ethics Committee 2021/17 approval was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kulaksiz, D., Toprak, T., Tokat, E. et al. Sperm concentration and semen volume increase after smoking cessation in infertile men. Int J Impot Res 34, 614–619 (2022). https://doi.org/10.1038/s41443-022-00605-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-022-00605-0
This article is cited by
-
Mechanisms and reversibility of nicotine-induced spermatogenesis impairment and DNA methylation changes
Communications Biology (2025)
-
Impact of conventional cigarette and electronic cigarette use on sperm quality and IVF/ICSI outcomes
Scientific Reports (2025)
-
Investigating cigarette smoke-induced airway inflammation and sperm activity impairment in rats based on cilia-associated proteins
3 Biotech (2025)
-
Nickel and human sperm quality: a systematic review
BMC Public Health (2024)
-
Influence of substance use on male reproductive health and offspring outcomes
Nature Reviews Urology (2024)