Abstract
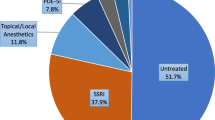
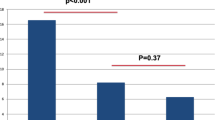
We investigated the prevalence, incidence, and rates of pharmacological treatment of delayed ejaculation using the TriNetX Diamond Network. We included all men evaluated in the inpatient, outpatient, and emergency settings. Prevalence was determined by comparing the number of men diagnosed with delayed ejaculation to the entire population. Incidence was determined by comparing the number of men diagnosed with delayed ejaculation without a prior diagnosis to the overall population without a prior diagnosis. Rates of pharmacologic treatment were calculated by comparing the number of men who received a prescription to the total number of men with delayed ejaculation. Trends in prevalence and incidence were compared using six-month intervals, while trends in pharmacologic treatment were compared using one-year intervals. A total of 23,164 adult males were diagnosed with delayed ejaculation from 2013 to 2019. During the final six-month interval (July to December 2019), 2,747 of 16,496,744 men received a delayed ejaculation diagnosis, and 1,375 of 16,488,270 men without a prior diagnosis were diagnosed with delayed ejaculation. In 2019, only 916 of 4,733 (19.4%) men diagnosed with delayed ejaculation received any prescription, with the most common being testosterone (9.5%), bupropion (6.6%), and buspirone (2.3%). Prevalence, incidence and pharmacologic treatment all had increasing trends.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data regarding any of the subjects in the study has not been previously published. Data will be made available to the editors of the journal for review or query upon request.
References
Shindel AW, Althof SE, Carrier S, Chou R, McMahon CG, Mulhall JP, et al. Disorders of Ejaculation: An AUA/SMSNA Guideline. J Urol. 2022;207:504–12.
Butcher MJ, Welliver RC Jr, Sadowski D, Botchway A, Kohler TS. How is delayed ejaculation defined and treated in North America? Andrology. 2015;3:626–31.
Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–7.
Rowland D, McMahon CG, Abdo C, Chen J, Jannini E, Waldinger MD, et al. Disorders of orgasm and ejaculation in men. J Sex Med. 2010;7:1668–86.
Jannini EA, Lenzi A. Ejaculatory disorders: epidemiology and current approaches to definition, classification and subtyping. World J Urol. 2005;23:68–75.
Perelman MA, Rowland DL. Retarded ejaculation. World J Urol. 2006;24:645–52.
Di Sante S, Mollaioli D, Gravina GL, Ciocca G, Limoncin E, Carosa E, et al. Epidemiology of delayed ejaculation. Transl Androl Urol. 2016;5:541–8.
Czeisler ME, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–7.
Smeets M, Vaes B, Mamouris P, Van Den Akker M, Van Pottelbergh G, Goderis G, et al. Burden of heart failure in Flemish general practices: a registry-based study in the Intego database. BMJ Open. 2019;9:e022972.
Beerten SG, Helsen A, De Lepeleire J, Waldorff FB, Vaes B. Trends in prevalence and incidence of registered dementia and trends in multimorbidity among patients with dementia in general practice in Flanders, Belgium, 2000-2021: a registry-based, retrospective, longitudinal cohort study. BMJ Open. 2022;12:e063891.
Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011;34:41–8.
Corona G, Jannini EA, Mannucci E, Fisher AD, Lotti F, Petrone L, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008;5:1991–8.
Corona G, Mannucci E, Petrone L, Fisher AD, Balercia G, De Scisciolo G, et al. Psychobiological correlates of delayed ejaculation in male patients with sexual dysfunctions. J Androl. 2006;27:453–8.
Paduch DA, Polzer P, Morgentaler A, Althof S, Donatucci C, Ni X, et al. Clinical and Demographic Correlates of Ejaculatory Dysfunctions Other Than Premature Ejaculation: A Prospective, Observational Study. J Sex Med. 2015;12:2276–86.
Abdel-Hamid IA, Ali OI. Delayed Ejaculation: Pathophysiology, Diagnosis, and Treatment. World J Mens Health. 2018;36:22–40.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
McCabe MP, Sharlip ID, Atalla E, Balon R, Fisher AD, Laumann E, et al. Definitions of Sexual Dysfunctions in Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13:135–43.
Abdel-Hamid IA, Elsaied MA, Mostafa T. The drug treatment of delayed ejaculation. Transl Androl Urol. 2016;5:576–91.
Kruger TH, Haake P, Haverkamp J, Kramer M, Exton MS, Saller B, et al. Effects of acute prolactin manipulation on sexual drive and function in males. J Endocrinol. 2003;179:357–65.
Piazza LA, Markowitz JC, Kocsis JH, Leon AC, Portera L, Miller NL, et al. Sexual functioning in chronically depressed patients treated with SSRI antidepressants: a pilot study. Am J Psychiatry. 1997;154:1757–9.
Harrison WM, Rabkin JG, Ehrhardt AA, Stewart JW, McGrath PJ, Ross D, et al. Effects of antidepressant medication on sexual function: a controlled study. J Clin Psychopharmacol. 1986;6:144–9.
Chen J. The pathophysiology of delayed ejaculation. Transl Androl Urol. 2016;5:549–62.
De Luca R, Bonanno M, Manuli A, Calabro RS. Cutting the First Turf to Heal Post-SSRI Sexual Dysfunction: A Male Retrospective Cohort Study. Medicines. 2022;9:45.
Author information
Authors and Affiliations
Contributions
Brian Liao: Idea generation, data collection, data analysis, manuscript writing, manuscript editing. Corey Able: Idea generation, data collection, data analysis, manuscript writing, manuscript editing. Steven Banner: Manuscript writing, manuscript editing. Clemens An: Manuscript writing, manuscript editing. Ali Nasrallah: Manuscript writing, manuscript editing. Kevin Vu: Manuscript writing, manuscript editing. Joseph Sonstein: Idea refinement, manuscript editing. Laith Alzweri: Idea refinement, manuscript editing. Taylor Kohn: Idea refinement, data analysis, manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The process by which the data was de-identified is attested to through a formal determination by a qualified expert as defined in Section §164.514(b)(1) of the HIPAA Privacy Rule. Because studies using TriNetX de-identified patient records do not involve the collection, use, or transmittal of individually identifiable data, the qualified expert has determined these studies are exempted from the need of Institutional Review Board review. Any patient counts less than 10 are obfuscated to ensure patient anonymity, and only aggregate patient counts and statistical summaries are provided.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liao, B., Able, C., Banner, S. et al. A population analysis of delayed ejaculation using a claims database: characteristics and national trends in prevalence, incidence, and pharmacotherapy. Int J Impot Res 37, 471–476 (2025). https://doi.org/10.1038/s41443-024-00937-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-024-00937-z
This article is cited by
-
Rare but real: clinical insights and take-home messages from the special issue on rare male sexual disorders
International Journal of Impotence Research (2025)