Abstract
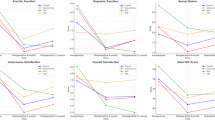
Very few studies examine sexuality after penile cancer (PeCa) surgery and/or evaluate predictors of sexual satisfaction. Since 2016, primary PeCa patients at our institute routinely received the International Index of Erectile Function (IIEF-15) questionnaire: preoperatively (baseline) and 3-, 6-, 12- and 24-months postoperatively. We included patients who were surgically treated at our institute and completed the baseline and ≥1 follow-up questionnaire. Sexually active patients were divided into groups: wide local excision (WLE), glansectomy, partial penectomy and total penectomy with perineal urethrostomy. Linear mixed effects models were used for longitudinal analyses with repeated measures to examine predictors of overall sexual satisfaction. 647 patients with (suspected) PeCa were evaluated and received questionnaires. 543 (83.9%) returned the questionnaires. 242 were suitable for analysis. Preoperatively, only 55/242 (22.7%) were sexually active. Postoperatively, the number of sexually active patients increased for WLE (30.8% at baseline, 43.5% at two-year follow-up) and glansectomy (35.0% to 40.0%, both p < 0.001). Sexual satisfaction was below the level of healthy men in all patients, both pre- and postoperatively. Longer follow-up time, younger age, and penile-sparing surgeries were predictors for better sexual satisfaction. Our findings underscore the importance of considering penile-sparing surgical approaches in the treatment of PeCa when oncologically feasible. The significant improvements in sexual activity and sexual satisfaction following WLE and glansectomy support this approach. However, the overall sexual satisfaction after all PeCa surgery remains below the level of the healthy men, both pre- and post-operative, emphasizing the importance of guidance throughout the treatment trajectory.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The dataset generated during and/or analysed during the current study is available from the corresponding author on reasonable request. The dataset is not publicly available due to privacy of the patients.
References
Agrawal A, Pai D, Ananthakrishnan N, Smile SR, Ratnakar C. The histological extent of the local spread of carcinoma of the penis and its therapeutic implications. BJU Int. 2000;85:299–301.
Sri D, Sujenthiran A, Lam W, Minter J, Tinwell BE, Corbishley CM, et al. A study into the association between local recurrence rates and surgical resection margins in organ-sparing surgery for penile squamous cell cancer. BJU Int. 2018;122:576–82.
Hegarty PK, Eardley I, Heidenreich A, McDougal WS, Minhas S, Spiess PE, et al. Penile cancer: organ-sparing techniques. BJU Int. 2014;114:799–805.
Dräger DL, Protzel C, Hakenberg OW. Identifying Psychosocial Distress and Stressors Using Distress-screening Instruments in Patients With Localized and Advanced Penile Cancer. Clin Genitourin Cancer. 2017;15:605–9.
Chaubey A, Tiwari S, Suryavanshi P, Jain V. Quality of Life Evaluation after Partial Penile Amputation for Penile Cancer. Ann Afr Med. 2024;23:352–7.
Bullen K, Edwards S, Marke V, Matthews S. Looking past the obvious: experiences of altered masculinity in penile cancer. Psychooncology. 2010;19:933–40.
Jovanović D, Aćimović M, Pejčić T, Milojević B, Čegar B, Zeković M, et al. Comprehensive Evaluation of Quality of Life in Penile Cancer Patients following Surgical Treatment. Healthcare. 2023;11:3091.
Suarez-Ibarrola R, Cortes-Telles A, Miernik A. Health-Related Quality of Life and Sexual Function in Patients Treated for Penile Cancer. Urol Int. 2018;101:351–7.
Sedigh O, Falcone M, Ceruti C, Timpano M, Preto M, Oderda M, et al. Sexual function after surgical treatment for penile cancer: Which organ-sparing approach gives the best results? Can Urol Assoc J. 2015;9:E423–7.
Falcone M, Preto M, Oderda M, Timpano M, Russo GI, Capogrosso P, et al. Total Glans Resurfacing for the Management of Superficial Penile Cancer: A Retrospective Cohort Analysis in a Tertiary Referral Center. Urology. 2020;145:281–6.
Djajadiningrat RS, van Werkhoven E, Meinhardt W, van Rhijn BW, Bex A, van der Poel HG, et al. Penile sparing surgery for penile cancer-does it affect survival? J Urol. 2014;192:120–5.
Leijte JA, Kirrander P, Antonini N, Windahl T, Horenblas S. Recurrence patterns of squamous cell carcinoma of the penis: recommendations for follow-up based on a two-centre analysis of 700 patients. Eur Urol. 2008;54:161–8.
Roussel E, Peeters E, Vanthoor J, Bozzini G, Muneer A, Ayres B, et al. Predictors of local recurrence and its impact on survival after glansectomy for penile cancer: time to challenge the dogma? BJU Int. 2021;127:606–13.
Cakir OO, Schifano N, Venturino L, Pozzi E, Castiglione F, Alnajjar HM, et al. Surgical technique and outcomes following coronal-sparing glans resurfacing for benign and malignant penile lesions. Int J Impot Res. 2022;34:495–500.
Pérez J, Chavarriaga J, Ortiz A, Orrego P, Rueda S, Quiroga W, et al. Oncological and Functional Outcomes After Organ-Sparing Plastic Reconstructive Surgery for Penile Cancer. Urology. 2020;142:161–5.e1.
Scarberry K, Angermeier KW, Montague D, Campbell S, Wood HM. Outcomes for Organ-Preserving Surgery for Penile Cancer. Sex Med. 2015;3:62–6.
Croghan SM, Cullen IM, Raheem O. Functional outcomes and health-related quality of life following penile cancer surgery: a comprehensive review. Sex Med Rev. 2023;11:441–59.
Platform Oncologie. SONCOS: Multidisciplinaire normering oncologische zorg in Nederland - version 10. 2022.
Sansalone S, Silvani M, Leonardi R, Vespasiani G, Iacovelli V. Sexual outcomes after partial penectomy for penile cancer: results from a multi-institutional study. Asian J Androl. 2017;19:57–61.
Falcone M, Preto M, Plamadeala N, Scavone M, Ferro I, Cirigliano L, et al. Total penectomy and perineal urethrostomy configuration in locally advanced penile cancer: oncological, surgical and functional outcomes. Am J Transl Res. 2024;16:6636–45.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Utomo E, Blok BF, Pastoor H, Bangma CH, Korfage IJ. The measurement properties of the five-item International Index of Erectile Function (IIEF-5): a Dutch validation study. Andrology. 2015;3:1154–9.
Meystre-Agustoni G, Jeannin A, de Heller K, Pécoud A, Bodenmann P, Dubois-Arber F. Talking about sexuality with the physician: are patients receiving what they wish? Swiss Med Wkly. 2011;141:w13178.
Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med. 2004;58:2093–103.
Gott M, Galena E, Hinchliff S, Elford H. “Opening a can of worms”: GP and practice nurse barriers to talking about sexual health in primary care. Fam Pr. 2004;21:528–36.
Roumieux C, Royakkers L, Albersen M, Dancet E. The impact of diagnosis and treatment of penile cancer on intimacy: a qualitative assessment. Int J Impot Res. 2024. https://doi.org/10.1038/s41443-024-00992-6.
Yang J, Chen J, Wu XF, Song NJ, Xu XY, Li Q, et al. Glans preservation contributes to postoperative restoration of male sexual function: a multicenter clinical study of glans preserving surgery. J Urol. 2014;192:1410–7.
Yu C, Hequn C, Longfei L, Minfeng C, Zhi C, Feng Z, et al. Sexual Function after Partial Penectomy: A Prospectively Study From China. Sci Rep. 2016;6:21862.
Masters W, Johnson V. Human sexual response. Boston: Little Brown; 1966.
Stoffel JT, Van der Aa F, Wittmann D, Yande S, Elliott S. Fertility and sexuality in the spinal cord injury patient. World J Urol. 2018;36:1577–85.
Traa MJ, Roukema JA, De Vries J, Rutten HJ, Langenhoff B, Jansen W, et al. Biopsychosocial predictors of sexual function and quality of sexual life: a study among patients with colorectal cancer. Transl Androl Urol. 2015;4:206–17.
Gil N, Fisher A, Beeken RJ, Pini S, Miller N, Buck C, et al. The role of partner support for health behaviours in people living with and beyond cancer: A qualitative study. Psychooncology. 2022;31:1997–2006.
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61.
Nimbi FM, Tripodi F, Rossi R, Navarro-Cremades F, Simonelli C. Male Sexual Desire: An Overview of Biological, Psychological, Sexual, Relational, and Cultural Factors Influencing Desire. Sex Med Rev. 2020;8:59–91.
Nicolosi A, Laumann EO, Glasser DB, Moreira ED Jr., Paik A, Gingell C. Sexual behavior and sexual dysfunctions after age 40: the global study of sexual attitudes and behaviors. Urology. 2004;64:991–7.
Acknowledgements
We wish to thank the Netherlands Cancer Institute urology department secretaries for their dedicated assistance. Their careful management of patient questionnaire tracking and data entry significantly contributed to the research process.
Author information
Authors and Affiliations
Contributions
MV helped with acquisition of data, statistical analysis and interpretation of data, drafting the manuscript, with critical revision for important intellectual content and approved the final version of the manuscript. MvH helped with acquisition of data, statistical analysis and interpretation of data, with critical revision for important intellectual content and approved the final version of the manuscript. HdV helped with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. KdL helped with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. JC helped with conception and design of the study, with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. SO helped with conception and design of the study, with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. IC helped with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. EM helped with conception and design of the study, with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. JK helped with conception and design of the study, with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. VN helped with statistical analysis and interpretation of the data, with critical revision for important intellectual content and approved the final version of the manuscript. HP helped with conception and design of the study, with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. HE helped with conception and design of the study, with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. MN helped with conception and design of the study, with statistical analysis and interpretation of the data, with drafting the manuscript, with critical revision for important intellectual content, approved the final version of the manuscript and provided supervision of the project. OR helped with conception and design of the study, with statistical analysis and interpretation of the data, with drafting the manuscript, with critical revision for important intellectual content, approved the final version of the manuscript and provided supervision of the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was approved by the Institutional Review Board of the Netherlands Cancer Institute (IRBd21-038). All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all participants involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vreeburg, M., van Harten, M., de Vries, H. et al. Sexual functioning after penile cancer surgery: comparison between surgical approaches in a large patient cohort. Int J Impot Res 37, 728–735 (2025). https://doi.org/10.1038/s41443-025-01063-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-025-01063-0
This article is cited by
-
“Penile cancer and sexuality: advancing care beyond oncological outcomes”
International Journal of Impotence Research (2025)
-
“Sexuality in penile cancer: lessons learned and the road ahead”
International Journal of Impotence Research (2025)
-
Organerhalt oder Radikalität? Moderne chirurgische Konzepte im Spannungsfeld von Funktion und Onkologie
Die Urologie (2025)