Abstract
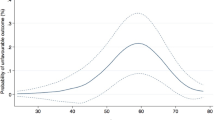
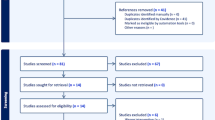
Erectile dysfunction (ED) is the most frequently reported male sexual dysfunction. Penile prosthesis implantation (PPI) is an effective solution for patients with medically refractory ED. Despite advancements in surgical techniques and device technology, detailed evidence on PPI complication rates is limited. A systematic review was conducted following PRISMA guidelines, including literature from Medline, Embase, Cochrane Libraries, and clinicaltrial.gov from 2000 to October 2024. Eligible studies included randomized controlled trials (RCTs), non-randomized comparative studies, and case series with ≥5 participants. Adult male patients (≥18 years) undergoing PPI for ED, Peyronie’s disease, or priapism were considered. Eligible interventions included malleable and hydraulic (two- or three-piece) prosthesis implantation, device explantation and reimplantation, and PPI combined with penile curvature correction. Primary outcomes were intraoperative and postoperative complication rates. Of the 1370 studies initially identified, 151 met inclusion criteria, encompassing a total of 92,777 patients. Device infections were reported in 103 studies, with rates ranging from 0.03–14.3%, predominantly under 5%. Erosion rates spanned 0.02–32.5%, with most studies reporting rates below 5%. Mechanical failure rates were highly variable, exceeding 15% in about half the studies with follow-up periods of 5 to 11 years. Intraoperative complications such as urethral injury and corporeal perforation were uncommon but occurred more frequently in patients with severe fibrosis, including those with priapism. Neurological comorbidities were associated with an elevated risk of mechanical failure, while diabetic patients did not exhibit a significantly increased infection risk compared to the general population. Modern techniques and coated devices have reduced infection and erosion rates. However, mechanical failure remains a concern, emphasizing the need for technological advancements. Tailored device selection and comprehensive pre- and postoperative management are critical to reducing revision rates and improving outcomes. Future research should address gaps in surgical approach optimization and complication management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are available from the corresponding author on reasonable request.
References
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the massachusetts male aging study. J Urol. 1994;151:54–61.
Rojanasarot S, Williams AO, Edwards N, Khera M. Quantifying the number of US men with erectile dysfunction who are potential candidates for penile prosthesis implantation. Sex Med. 2023;11:010.
Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. European association of urology guidelines on sexual and reproductive health—2021 update: male sexual dysfunction[Formula presented]. Eur Urol. 2021;80:333–57.
Levine LA, Becher E, Bella A, Brant W, Kohler T, Martinez-Salamanca JI, et al. Penile prosthesis surgery: current recommendations from the international consultation on sexual medicine. J Sex Med. 2016;13:489–518.
Miller LE, Khera M, Bhattacharyya S, Patel M, Nitschelm K, Burnett AL. Long-term survival rates of inflatable penile prostheses: systematic review and meta-analysis. Urology. 2022;166:6–10.
Wilson SK, Zumbe J, Henry GD, Salem EA, Delk JR, Cleves MA. Infection reduction using antibiotic-coated inflatable penile prosthesis. Urology. 2007;70:337–40.
Eid JF, Wilson SK, Cleves M, Salem EA. Coated implants and “no Touch” surgical technique decreases risk of infection in inflatable penile prosthesis implantation to 0.46%. Urology. 2012;79:1310–5.
Loh-Doyle JC, Lin JS, Doumanian LR, Patil MB, Boyd SD. Outcomes of alternative reservoir placement in the lateral retroperitoneum during inflatable penile prosthesis placement. Urology. 2021;152:35–41.
Frydman V, Pinar U, Abdessater M, Akakpo W, Grande P, Audouin M, et al. Long-term outcomes after penile prosthesis placement for the management of erectile dysfunction: a single-Centre experience. Basic Clin Androl. 2021;31:4.
Colombo F, Gentile G, Vagnoni V, Fiorillo A, Piazza P, Sartorio F, et al. Initial experience of a single center with the use of ZSI 475 penile prosthesis. Asian J Urol. 2021;8:176–82.
Di Pierro GB, Lemma A, Di Lascio G, El Motassime A, Grande P, Di Giulio I, et al. Primary versus revision implant for inflatable penile prosthesis: a propensity score-matched comparison. Andrologia. 2021;53:14240.
Scarberry KA, Thomas GM, Cowper M, Chouhan JD, Thakker PU, Matz EL, et al. Sustained glycemic control observed in diabetic men who improve hemoglobin A1c values to allow for elective penile prosthesis placement. Urology. 2020;146:140–4.
Baumgarten AS, Kavoussi M, VanDyke ME, Ortiz NM, Khouri RK, Ward EE, et al. Avoiding deep pelvic complications using a ‘Five-Step’ technique for high submuscular placement of inflatable penile prosthesis reservoirs. BJU Int. 2020;126:457–63.
Hatzichristodoulou G, Yang DY, Ring JD, Hebert KJ, Ziegelman MJ, Köhler TS. Multicenter experience using collagen fleece for plaque incision with grafting to correct residual curvature at the time of inflatable penile prosthesis placement in patients with Peyronie’s disease. J Sex Med. 2020;17:1168–74.
Weinberg AC, Siegelbaum MH, Lerner BD, Schwartz BC, Segal RL. Inflatable penile prosthesis in the ambulatory surgical setting: outcomes from a large urological group practice. J Sex Med. 2020;17:1025–32.
Fuentes JL, Yi YA, Davenport MT, Bergeson RL, Ward EE, Morey AF. Long-term sequelae of inflatable penile prosthesis: clinical characteristics of patients who develop distal cylinder tip extrusion. Transl Androl Urol. 2020;9:38–42.
Fernández-Pascual E, Gonzalez-García FJ, Rodríguez-Monsalve M, Turo J, Martínez-Ballesteros C, Carballido J, et al. Surgical technique for complex cases of peyronie’s disease with implantation of penile prosthesis, multiple corporeal incisions, and grafting with collagen fleece. J Sex Med. 2019;16:323–32.
Falcone M, Preto M, Ceruti C, Timpano M, Garaffa G, Sedigh O, et al. A comparative study between 2 different grafts used as patches after plaque incision and inflatable penile prosthesis implantation for end-stage Peyronie’s disease. J Sex Med. 2018;15:848–52.
Kavoussi NL, Viers BR, VanDyke ME, Pagliara TJ, Morey AF. “Stiction Syndrome”: non-operative management of patients with difficult AMS 700 series inflation. J Sex Med. 2017;14:1079–83.
Pineda M, Burnett AL. Distinguishing failure to cure from complication after penile prosthesis implantation. J Sex Med. 2017;14:731–7.
Blewniewski M, Ostrowski I, Pottek T, Neugart F, Ciechan J, Llorens C, et al. Safety and efficacy outcomes of ZSI 475 penile prosthesis. Urologia J. 2017;84:98–101.
Tsambarlis PN, Chaus F, Levine LA. Successful placement of penile prostheses in men with severe corporal fibrosis following vacuum therapy protocol. J Sex Med. 2017;14:44–6.
Garber BB, Lim C. Inflatable penile prosthesis insertion in men with severe intracorporal fibrosis. Curr Urol. 2017;10:92–6.
Pescatori E, Alei G, Antonini G, Avolio A, Bettocchi C, Bitelli M, et al. INSIST-ED: Italian society of andrology registry on penile prosthesis surgery. First data analysis. Arch Ital Urol Androl. 2016;88:122–7.
Karpman E, Brant WO, Kansas B, Bella AJ, Jones LRA, Eisenhart E, et al. Reservoir alternate surgical implantation technique: preliminary outcomes of initial PROPPER study of low profile or spherical reservoir implantation in submuscular location or traditional prevesical space. J Urol. 2015;193:239–44.
Bozkurt IH, Arslan B, Yonguç T, Kozacioglu Z, Degirmenci T, Gunlusoy B, et al. Patient and partner outcome of inflatable and semi-rigid penile prosthesis in a single institution. Int Braz J Urol. 2015;41:535–41.
Stember DS, Garber BB, Perito PE. Outcomes of abdominal wall reservoir placement in inflatable penile prosthesis implantation: a safe and efficacious alternative to the space of retzius. J Sex Med. 2014;11:605–12.
Zacharakis E, Garaffa G, Raheem AA, Christopher AN, Muneer A, Ralph DJ. Penile prosthesis insertion in patients with refractory ischaemic priapism: early vs delayed implantation. BJU Int. 2014;114:576–81.
Grewal S, Vetter J, Brandes SB, Strope SA. A population-based analysis of contemporary rates of reoperation for penile prosthesis procedures. Urology. 2014;84:112–6.
Simsek A, Kucuktopcu O, Ozgor F, Ozkuvanci U, Baykal M, Sarilar O, et al. Self and partner satisfaction rates after 3 part inflatable penile prosthesis implantation. Arch Ital Urol Androl. 2014;86:219.
Morey AF, Cefalu CA, Hudak SJ. High submuscular placement of urologic prosthetic balloons and reservoirs via transscrotal approach. J Sex Med. 2013;10:603–10.
Vitarelli A, Divenuto L, Fortunato F, Falco A, Pagliarulo V, Antonini G, et al. Long term patient satisfaction and quality of life with AMS700CX inflatable penile prosthesis. Arch Ital Urol Androl. 2013;85:133–7.
Ohl DA, Brock G, Ralph D, Bogache W, Jones L, Munarriz R, et al. Prospective evaluation of patient satisfaction, and surgeon and patient trainer assessment of the coloplast titan one touch release three-piece inflatable penile prosthesis. J Sex Med. 2012;9:2467–74.
Henry GD, Brinkman MJ, Mead SF, Delk JR, Cleves MA, Jennermann C, et al. A survey of patients with inflatable penile prostheses: assessment of timing and frequency of intercourse and analysis of implant durability. J Sex Med. 2012;9:1715–21.
Levine LA, Benson J, Hoover C. Inflatable penile prosthesis placement in men with peyronie’s disease and drug-resistant erectile dysfunction: a single-center study. J Sex Med. 2010;7:3775–83.
Paranhos M, Andrade E, Antunes AA, Barbieri ALN, Claro JA, Srougi M. Penile prosthesis implantation in an academic institution in Latin America. Int Braz J Urol. 2010;36:591–601.
Lux M, Reyes-Vallejo L, Morgentaler A, Levine LA. Outcomes and satisfaction rates for the redesigned 2-piece penile prosthesis. J Urol. 2007;177:262–6.
Montague DK, Angermeier KW. Corporeal excavation: new technique for penile prosthesis implantation in men with severe corporeal fibrosis. Urology. 2006;67:1072–5.
Minervini A, Ralph DJ, Pryor JP. Outcome of penile prosthesis implantation for treating erectile dysfunction: experience with 504 procedures. BJU Int. 2006;97:129–33.
Zermann DH, Kutzenberger J, Sauerwein D, Schubert J, Loeffler U. Penile prosthetic surgery in neurologically impaired patients: long-term followup. J Urol. 2006;175:1041–4.
Abouassaly R, Angermeier KW, Montague DK. Risk of infection with an antibiotic coated penile prosthesis at device replacement for mechanical failure. J Urol. 2006;176:2471–3.
Jensen JB, Larsen EH, Kirkeby HJ, Jensen KME. Clinical experience with the mentor alpha-1 inflatable penile prosthesis: report on 65 patients. Scand J Urol Nephrol. 2005;39:69–72.
Milbank AJ, Montague DK, Angermeier KW, Lakin MM, Worley SE. Mechanical failure of the American medical systems ultrex inflatable penile prosthesis: Before and after 1993 structural modification. J Urol. 2002;167:2502–6.
Hollenbeck BK, Miller DC, Ohl DA. The utility of lockout valve reservoirs in preventing autoinflation in penile prostheses. Int Urol Nephrol. 2002;34:379–83.
Soliman HE, Milad MF, Ayyat FM, Zein TA, Hussein ESA. Penile implants in the treatment of organic impotence. Saudi Med J. 2001;22:30–3.
Chung E, Solomon M, Deyoung L, Brock GB. Comparison between AMS 700TM CX and ColoplastTM titan inflatable penile prosthesis for peyronie’s disease treatment and remodeling: clinical outcomes and patient satisfaction. J Sex Med. 2013;10:2855–60.
Ralla B, Goranova I, Börnstein N, Friedersdorff F, Maxeiner A, Magheli A, et al. Complications, functional and quality of life outcomes following primary and secondary implantation of penile prosthesis at a tertiary referral center. Int J Impot Res. 2018;30:49–53.
Sansalone S, Garaffa G, Djinovic R, Antonini G, Vespasiani G, Ieria FP, et al. Simultaneous total corporal reconstruction and implantation of a penile prosthesis in patients with erectile dysfunction and severe fibrosis of the corpora cavernosa. J Sex Med. 2012;9:1937–44.
Johnson BE, Langford BT, VanDyke ME, Matz EL, Cook GS, Franzen BP, et al. Long-term experience with AMS-700 CXR inflatable penile prosthesis in high-risk patients with corporal fibrosis. Int J Impot Res. 2024;37:66–71.
Park SH, Wilson SK, Wen L. Subcoronal incision for inflatable penile prosthesis does not risk glans necrosis. J Urol. 2023;210:678–87.
Lucas JW, Gross MS, Barlotta RM, Sudhakar A, Hoover CRV, Wilson SK, et al. Optimal modeling: an updated method for safely and effectively eliminating curvature during penile prosthesis implantation. Urology. 2020;146:133–9.
Hatzichristodoulou G. The PICS technique: a novel approach for residual curvature correction during penile prosthesis implantation in patients with severe Peyronie’s disease using the collagen fleece TachoSil. J Sex Med. 2018;15:416–21.
Clavell-Hernández J, Wang R. Penile size restoration with nondegloving approach for Peyronie’s disease: initial experience. J Sex Med. 2018;15:1506–13.
Gross MS, Stember DS, Garber BB, Perito PE. A retrospective analysis of risk factors for IPP reservoir entry into the peritoneum after abdominal wall placement. Int J Impot Res. 2017;29:215–8.
Weinberg AC, Pagano MJ, Deibert CM, Valenzuela RJ. Sub-coronal inflatable penile prosthesis placement with modified no-touch technique: a step-by-step approach with outcomes. J Sex Med. 2016;13:270–6.
Garber BB, Khurgin JL, Stember DS, Perito PE. Pseudo-malfunction of the coloplast titan inflatable penile prosthesis one-touch release pump. Urology. 2014;84:857–9.
Borges F, Hakim L, Kline C. Surgical technique to maintain penile length after insertion of an inflatable penile prosthesis via infrapubic approach. J Sex Med. 2006;3:550–3.
Krughoff K, Bearelly P, Apoj M, Munarriz NA, Thirumavalavan N, Pan S, et al. Multicenter surgical outcomes of penile prosthesis placement in patients with corporal fibrosis and review of the literature. Int J Impot Res. 2022;34:86–92.
Bearelly P, D’Amico M, Pan S, Thirumavalavan N, Gross MS, Maria P, et al. Intraoperative use of vancomycin paste during penile prosthesis placement: initial outcomes. Int J Impot Res. 2022;34:81–5.
Rahman NU, Carrion RE, Bochinski D, Lue TF. Combined penile plication surgery and insertion of penile prosthesis for severe penile curvature and erectile dysfunction. J Urol. 2004;171:2346–9.
Wilson SK, Henry GD, Delk JR, Cleves MA. The mentor alpha 1 penile prosthesis with reservoir lock-out valve: effective prevention of auto-inflation with improved capability for ectopic reservoir placement. J Urol. 2002;168:1475–8.
Barham DW, Chang C, Hammad M, Pyrgidis N, Swerdloff D, Gross K, et al. Delayed placement of an inflatable penile prosthesis is associated with a high complication rate in men with a history of ischemic priapism. J Sex Med. 2023;20:1052–6.
Loloi J, Matloubieh J, Riley C, Babar M, Melendez D, Watts K, et al. Hypertension and low cholesterol as risk factors for infection after primary inflatable penile prosthesis surgery. J Mens Health. 2022;18:1–5.
Falcone M, Pucci L, Garaffa G, Cocci A, Gillo A, Capece M, et al. An outcomes analysis of penile prosthesis implantation following radical cystoprostatectomy and urinary diversion: a multicentric retrospective cohort study. Int J Impot Res. 2020;32:126–32.
Kim KS, Bae WJ, Kim SW, Lee MY. Experience with AMS 700 LGX penile prostheses for preserving penile length in Korea. BMC Urol. 2019;19:6.
Grande P, Antonini G, Cristini C, De Berardinis E, Gatto A, Di Lascio G, et al. Penoscrotal versus minimally invasive infrapubic approach for inflatable penile prosthesis placement: a single-center matched-pair analysis. World J Urol. 2018;36:1167–74.
Roth J, Monn M, Shelton T, Mellon M. A novel technique for direct visualization of reservoir placement for penoscrotal inflatable penile prostheses using a single incision. Indian J Urol. 2018;34:283–6.
Ji YS, Ko YH, Song PH, Moon KH. Long-term survival and patient satisfaction with inflatable penile prosthesis for the treatment of erectile dysfunction. Korean J Urol. 2015;56:461–5.
Bozkurt IH, Arslan B, Kozacioglu Z, Yonguc T, Degirmenci T, Gunlusoy B, et al. Does the etiology affect the outcome and satisfaction rates of penile prosthesis implantation surgery? Kaohsiung J Med Sci. 2014;30:570–3.
Djordjevic ML, Kojovic V. Penile prosthesis implantation and tunica albuginea incision without grafting in the treatment of Peyronie’s disease with erectile dysfunction. Asian J Androl. 2013;15:391–4.
Chung E, Van CT, Wilson I, Cartmill RA. Penile prosthesis implantation for the treatment for male erectile dysfunction: clinical outcomes and lessons learnt after 955 procedures. World J Urol. 2013;31:591–5.
Thomas AZ, Carrol R, Manecksha RP, Thornhill JA, Grainger R, McDermott TED. Extended long term functional outcome of inflatable penile prosthesis in a single institution. Ir Med J. 2011;104:53–5.
Kim DS, Yang KM, Chung HJ, Choi HM, Choi YD, Choi HK. AMS 700CX/CXM inflatable penile prosthesis has high mechanical reliability at long-term follow-up. J Sex Med. 2010;7:2602–7.
Moncada I, Martínez-Salamanca JI, Jara J, Cabello R, Moralejo M, Hernández C. Inflatable penile prosthesis implantation without corporeal dilation: a cavernous tissue sparing technique. J Urol. 2010;183:1123–6.
Hartman RJ, Helfand BT, McVary KT. Outcomes of lateral retroperitoneal reservoir placement of three-piece penile prosthesis in patients following radical prostatectomy. Int J Impot Res. 2010;22:279–83.
Natali A, Olianas R, Fisch M. Penile implantation in Europe: successes and complications with 253 implants in Italy and Germany. J Sex Med. 2008;5:1503–12.
Dhar NB, Angermeier KW, Montague DK. Long-term mechanical reliability of AMS 700CXTM/CXM inflatable penile prosthesis. J Urol. 2006;176:2599–601.
Levine LA, Estrada CR, Morgentaler A. Mechanical reliability and safety of, and patient satisfaction with the ambicor inflatable penile prosthesis: Results of a 2 center study. J Urol. 2001;166:932–7.
Deuk Choi Y, Jin Choi Y, Hwan Kim J, Ki Choi H. Mechanical reliability of the AMS 700CXM inflatable penile prosthesis for the treatment of male erectile dysfunction. J Urol. 2001;165:822–4.
Carson CC. Penile prosthesis implantation in the treatment of Peyronie’s disease and erectile dysfunction. Int J Impot Res. 2000;12:S122–S126.
Khoei A, Racik N, Bansal U, Flores F, Khera M. The low submuscular reservoir placement with transfascial fixation for inflatable penile prostheses. J Sex Med. 2022;19:1309–12.
Pazir Y, Yanaral F, Caglar U, Ortac M, Sarilar O, Ozgor F. Evaluation of satisfaction and outcomes of patients who underwent two-piece inflatable penile prosthesis implantation. Cureus. 2022;14:26097.
Cocera R, Torremade J, Suarez JF, Fernandez-Concha J, Vigues F. Comparative analysis of penile implants in patients with vasculogenic erectile dysfunction versus postradical prostatectomy erectile dysfunction. Int J Impot Res. 2020;32:606–10.
Rolle L, Falcone M, Ceruti C, Timpano M, Sedigh O, Ralph DJ, et al. A prospective multicentric international study on the surgical outcomes and patients’ satisfaction rates of the “sliding” technique for end-stage Peyronie’s disease with severe shortening of the penis and erectile dysfunction. BJU Int. 2016;117:814–20.
Gentile G, Franceschelli A, Massenio P, Tuccio A, Cocci A, Divenuto L, et al. Patient’s satisfaction after 2-piece inflatable penile prosthesis implantation: An Italian multicentric study. Arch Ital Urol Androl. 2016;88:1–3.
Menard J, Tremeaux JC, Faix A, Pierrevelcin J, Staerman F. Erectile function and sexual satisfaction before and after penile prosthesis implantation in radical prostatectomy patients: a comparison with patients with vasculogenic erectile dysfunction. J Sex Med. 2011;8:3479–86.
Sedigh O, Rolle L, Negro CLA, Ceruti C, Timpano M, Galletto E, et al. Early insertion of inflatable prosthesis for intractable ischemic priapism: our experience and review of the literature. Int J Impot Res. 2011;23:158–64.
Diblasio CJ, Kurta JM, Botta S, Malcolm JB, Wan JY, Derweesh IH, et al. Peyronie’s disease compromises the durability and component-malfunction rates in patients implanted with an inflatable penile prosthesis. BJU Int. 2010;106:691–4.
Wilson SK, Delk JR, Mulcahy JJ, Cleves M, Salem EA. Upsizing of inflatable penile implant cylinders in patients with corporal fibrosis. J Sex Med. 2006;3:736–42.
Manning M, Martínez FJ, Alken P, Jünemann KP. Spontaneous tumescence after implantation of three-piece hydraulic penile prostheses: a short-term experience. Int J Impot Res. 2003;15:152–5.
Wilson SK, Cleves MA, Delk JR. Long-term followup of treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesis. J Urol. 2001;165:825–9.
Chiang HS, Wu CC, Wen TC. 10 Years of experience with penile prosthesis implantation in Taiwanese patients. J Urol. 2000;163:476–80.
Hawks-Ladds N, Babar M, Labagnara K, Loloi J, Patel RD, Aalami Harandi A, et al. Risk factors for reoperation of inflatable penile prosthesis among an ethnically diverse urban population in a high-volume center. Int J Impot Res. 2024;37:37–44.
Falcone M, Capogrosso P, Cirigliano L, Geretto P, Preto M, Timpano M, et al. The outcomes of penile prosthesis in neurologic patients: a multicentric retrospective series. Ther Adv Urol. 2023;15:17562872231194921.
Preto M, Falcone M, Plamadeala N, Schifano N, Bettocchi C, Colombo F, et al. Risk of unfavorable outcomes after penile prosthesis implantation – results from a national registry (INSIST-ED). Int J Impot Res. 2023;36:842–7.
Nelson CP, Bloom DA, Kinast R, Wei JT, Park JM. Patient-reported sexual function after oral mucosa graft urethroplasty for hypospadias. Urology. 2005;66:1086–9.
Egydio PH, Kuehhas FE. Distal penile shaft reconstruction and reinforcement: the “Double-Windsocks” technique. J Sex Med. 2013;10:2571–8.
Dave CN, Khalaf A, Patel HD, Kohn TP, Burnett AL. Neurogenic bladder is an independent risk factor for complications associated with inflatable penile prosthesis implantation. Int J Impot Res. 2020;32:520–4.
Pederzoli F, Chappidi MR, Collica S, Kates M, Joice GA, Sopko NA, et al. Analysis of hospital readmissions after prosthetic urologic surgery in the United States: nationally representative estimates of causes, costs, and predictive factors. J Sex Med. 2017;14:1059–65.
Antonini G, Busetto GM, De Berardinis E, Giovannone R, Vicini P, Del Giudice F, et al. Minimally invasive infrapubic inflatable penile prosthesis implant for erectile dysfunction: evaluation of efficacy, satisfaction profile and complications. Int J Impot Res. 2016;28:4–8.
Papagiannopoulos D, Yura E, Levine L. Examining postoperative outcomes after employing a surgical algorithm for management of Peyronie’s disease: a single-institution retrospective review. J Sex Med. 2015;12:1474–80.
Segal RL, Cabrini MR, Bivalacqua TJ, Burnett AL. Penile straightening maneuvers employed during penile prosthesis surgery: technical options and outcomes. Int J Impot Res. 2014;26:182–5.
Lindeborg L, Fode M, Fahrenkrug L, Sonksen J. Satisfaction and complications with the Titan® one-touch release penile implant. Scand J Urol. 2014;48:105–9.
Akin Y, Sahiner IF, Usta MF. The impact of diabetes mellitus on penile length in men undergoing inflatable penile prosthesis implantation. Turk J Urol. 2014;39:161–4.
Mulcahy JJ, Carson CC. Long-term infection rates in diabetic patients implanted with antibiotic-impregnated versus nonimpregnated inflatable penile prostheses: 7-year outcomes. Eur Urol. 2011;60:167–72.
Wilson SK, Haxhimolla H, Kua B, Testa G, Love C, Rossello M, et al. Survival From revision surgery for new rigicon Infla10 three-piece inflatable penile prosthesis is comparable to preceding devices. Urology. 2023;180:257–61.
Wilson SK, Wen L, Rossello M, Maria P, Carrion R, Perito P, et al. Initial safety outcomes for the Rigicon Infla10® inflatable penile prosthesis. BJU Int. 2023;131:729–33.
Shumaker L, Zulia N, Kennedy E, Beilan J, Ortiz N, Baumgarten A. Delayed closed-suction drain removal following inflatable penile prosthesis placement: a multi-institutional experience. J Sex Med. 2023;20:1440–5.
Micallef D, Wightman S, Naqi M, Modgil V, Pearce I. Is the infrapubic approach a safe option for patients with poorly controlled diabetes mellitus and obesity undergoing inflatable penile prosthesis surgery? J Clin Urol. 2022;18:61–8.
Szell NM, McIntosh GV, Dimatteo AD, Campbell T, Shaw MK. Retropubic dilation with a foley catheter balloon: a novel technique for penile prosthesis reservoir placement. J Am Osteopath Assoc. 2016;116:594–8.
Bozkurt YE, Akdeniz CB, Gümüş BH. Long-term results of three-part penile prosthesis implantation with ectopic reservoir placement in the treatment of erectile dysfunction: is supramuscular tubulation a reliable method? Basic Clin Androl. 2024;34:8.
La Croce G, Schifano N, Pescatori E, Caraceni E, Colombo F, Bettocchi C, et al. Which patient may benefit the most from penile prosthesis implantation? Andrology. 2022;10:1567–74.
Palmisano F, Boeri L, Ievoli R, Sánchez-Curbelo J, Spinelli M, Gregori A, et al. Ten-year experience with penile prosthetic surgery for the treatment of erectile dysfunction: outcomes of a tertiary referral center and predictors of early prosthetic infection. Asian J Androl. 2022;24:32–39.
Chen T, Li S, Eisenberg ML. The association between hemoglobin A1c levels and inflatable penile prosthesis infection: analysis of US insurance claims data. J Sex Med. 2021;18:1104–9.
Kisa E, Keskin MZ, Yucel C, Ucar M, Yalbuzdag O, Ilbey YO. Comparison of penile prosthesis types’ complications: a retrospective analysis of single center. Arch Ital Urol Androl. 2020;92. https://doi.org/10.4081/aiua.2020.4.386.
Çayan S, Aşcı R, Efesoy O, Bolat MS, Akbay E, Yaman Ö. Comparison of long-term results and couples’ satisfaction with penile implant types and brands: lessons learned from 883 patients with erectile dysfunction who underwent penile prosthesis implantation. J Sex Med. 2019;16:1092–9.
Canguven O, Talib R, El Ansari W, Khalafalla K, Al Ansari A. Is Hba1c level of diabetic patients associated with penile prosthesis implantation infections? Aging Male. 2019;22:28–33.
Golan R, Patel NA, Sun T, Barbieri CE, Sedrakyan A, Kashanian JA. Impact of pelvic radiation therapy on inflatable penile prosthesis reoperation rates. J Sex Med. 2018;15:1653–8.
Sevinc C, Ozkaptan O, Balaban M, Yucetas U, Karadeniz T. Outcome of penile prosthesis implantation: are malleable prostheses an appropriate treatment option in patients with erectile dysfunction caused by prior radical surgery? Asian J Androl. 2016;18.
Mohamed ER, Hammady AR, Eldahshoury MZ, Elsharkawi AM, Riad AM, Elmogazy HM, et al. Surgical outcomes and complications of Tube® (Promedon) malleable penile prostheses in diabetic versus non-diabetic patients with erectile dysfunction. Arab J Urol. 2016;14:305–11.
Pozza D, Pozza M, Musy M, Pozza C. 500 penile prostheses implanted by a surgeon in Italy in the last 30 years. Arch Ital Urol Androl. 2015;87:216–21.
Zabar KJ, Ahmadi A, Jalal AA. Penile prosthesis implantation for the treatment of erectile dysfunction. Bahrain Med Bull. 2009;31.
Fathy A, Shamloul R, Abdelrahim A, Zeidan A, El-Dakhly R, Ghanem H. Experience with Tube® (Promedon) malleable penile implant. Urol Int. 2007;79:244–7.
Wilson SK, Wen L, Carrion R, Eid F, Lentz A, Shah B, et al. Safety outcomes of the first Rigi10TM malleable penile prostheses implanted worldwide. Int J Impot Res. 2023;36:833–7.
Salman B, Elsherif E, Elgharabawy M, Badawy A. Early versus delayed penile prosthesis insertion for refractory ischemic priapism. Arab J Urol. 2023;21:76–81.
Habous M, Omar M, Farag M, Abdelwahab O, Laban O, Binsaleh S, et al. Malleable penile implant rod diameter predicts complications and patient satisfaction. Sex Med. 2022;10:100486–100486.
Kim YD, Yang SO, Lee JK, Jung TY, Shim HB. Usefulness of a malleable penile prosthesis in patients with a spinal cord injury. Int J Urol. 2008;15:919–23.
Topuz B, Ebiloğlu T, Zor M, Kaya E, Sarıkaya S, Emrah Coğuplugil A, et al. Penile prosthesis implantation: a single center 25 years of experience. Prog Urol. 2021;31:663–70.
Durazi MH, Jalal AA. Penile prosthesis implantation for treatment of postpriapism erectile dysfunction. Urol J. 2008;5:115–9.
Ferguson KH, Cespedes RD. Prospective long-term results and quality-of-life assessment after Dura-II penile prosthesis placement. Urology. 2003;61:437–41.
Elhawy MM, Fawzy AM. Outcomes of low-flow priapism and role of integrated penile prosthesis management. Afr J Urol. 2021;27:8.
Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified “sliding” technique. BJU Int. 2015;116:965–72.
Pathak AS, Chang JH, Parekh AR, Aboseif SR. Use of rectus fascia graft for corporeal reconstruction during placement of penile implant. Urology. 2005;65:1198–201.
Antonini G, De Berardinis E, Del Giudice F, Busetto GM, Lauretti S, Fragas R, et al. Inflatable penile prosthesis placement, scratch technique and postoperative vacuum therapy as a combined approach to definitive treatment of Peyronie’s disease. J Urol. 2018;200:642–7.
Chung PH, Scott JF, Morey AF. High patient satisfaction of inflatable penile prosthesis insertion with synchronous penile plication for erectile dysfunction and Peyronie’s disease. J Sex Med. 2014;11:1593–8.
Kadioglu A, Sanli O, Akman T, Cakan M, Erol B, Mamadov F. Surgical treatment of Peyronie’s disease: a single center experience with 145 patients. Eur Urol. 2008;53:432–9.
Chaudhary M, Sheikh N, Asterling S, Ahmad I, Greene D. Peyronie’s disease with erectile dysfunction: penile modeling over inflatable penile prostheses. Urology. 2005;65:760–4.
Sansalone S, Garaffa G, Djinovic R, Egydio P, Vespasiani G, Miano R, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with peyronie’s disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med. 2012;9:316–21.
Levine LA, Dimitriou RJ. A surgical algorithm for penile prosthesis placement in men with erectile failure and Peyronie’s disease. Int J Impot Res. 2000;12:147–51.
Egydio PH, Kuehhas FE, Sansalone S. Penile length and girth restoration in severe Peyronie’s disease using circular and longitudinal grafting. BJU Int. 2013;111:213–9.
Moncada I, Krishnappa P, Zaccaro C, Fraile A, Romero-Otero J, Martinez-Salamanca JI, et al. Penile prosthesis implantation is safe and effective in Peyronie’s disease patients with and without erectile dysfunction. Int J Impot Res. 2024;37:61–5.
Spinozzi L, Droghetti M, Palmisano F, Piazza P, Fontanella L, Gentile G, et al. Use of soft penile prosthesis in grafting surgery for Peyronie’s disease and mild erectile dysfunction: still an option? Arch Esp Urol. 2024;77:270–7.
Tausch TJ, Chung PH, Siegel JA, Gliga L, Klein AK, Morey AF. Intraoperative decision-making for precise penile straightening during inflatable penile prosthesis surgery. Urology. 2015;86:1048–52.
Krishnappa P, Tripathi A, Shah R. Surgical outcomes and patient satisfaction with the low-cost, semi-rigid shah penile prosthesis: a boon to the developing countries. Sex Med. 2021;9:100399.
Akdemir F, Okulu E, Kaylgil. Long-term outcomes of AMS Spectra® penile prosthesis implantation and satisfaction rates. Int J Impot Res. 2017;29:184–8.
Katz BF, Gaunay GS, Barazani Y, Nelson CJ, Moreira DM, Dinlenc CZ, et al. Use of a preoperative checklist reduces risk of penile prosthesis infection. J Urol. 2014;192:130–5.
Serefoglu EC, Mandava SH, Gokce A, Chouhan JD, Wilson SK, Hellstrom WJG. Long-term revision rate due to infection in hydrophilic-coated inflatable penile prostheses: 11-year follow-up. J Sex Med. 2012;9:2182–6.
Henry GD, Donatucci CF, Conners W, Greenfield JM, Carson CC, Wilson SK, et al. An outcomes analysis of over 200 revision surgeries for penile prosthesis implantation: a multicenter study. J Sex Med. 2012;9:309–15.
Haobus M, Almannie R, Aziz M, Farag M, Ralph D, Mulhall J, et al. Correlation of fasting blood sugar at the time of penile prosthesis surgery with the level of glycated hemoglobin and the outcome of surgery. Afr J Urol. 2021;27:90.
Tausch TJ, Zhao LC, Morey AF, Siegel JA, Belsante MJ, Seideman CA, et al. Malleable penile prosthesis is a cost-effective treatment for refractory ischemic priapism. J Sex Med. 2015;12:824–6.
Hsu GL, Chen HS, Huang SJ. Does tunica anatomy matter in penile implant? Transl Androl Urol. 2015;4:406–12.
Zacharakis E, De Luca F, Raheem AA, Garaffa G, Christopher N, Muneer A, et al. Early insertion of a malleable penile prosthesis in ischaemic priapism allows later upsizing of the cylinders. Scand J Urol. 2015;49:468–71.
Habous M, Tealab A, Farag M, Soliman T, Williamson B, Mahmoud S, et al. Malleable penile implant is an effective therapeutic option in men with Peyronie’s disease and erectile dysfunction. Sex Med. 2018;6:24–9.
Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the combAT study. Eur Urol. 2010;57:123–31.
European Association of Urology. EAU Guidelines on Sexual Medicine. Arnhem, The Netherlands: European Association of Urology; 2025.
Raheem OA, Hsieh TC. Penile prosthetic surgery for the management of Peyronie’s disease. Transl Androl Urol. 2017;6:S815–S821.
Patel J, Zakkar B, Polchert M, Tannenbaum J, Dick B, Raheem O. Recent technological development of penile prosthesis: a literature review. Transl Androl Urol. 2024;13:165–84.
Yavuz U, Ciftci S, Ustuner M, Yilmaz H, Culha M. Surgical treatment of erectile dysfunction and Peyronie’s disease using malleable prosthesis. Urol J. 2015;12:2428–33.
Acknowledgements
Marta Pezzoli, for her contribution to this Systematic Review. This Systematic Review was performed under the auspices of the: European Association of Urology Guidelines Office Board; European Association of Urology Sexual & Reproductive Health Guidelines Panel.
Funding
European Association of Urology.
Author information
Authors and Affiliations
Consortia
Contributions
AC, PC, SM, AS were responsible for designing the review protocol and writing the protocol; AC, PC, SM, AS was responsible for writing the report; AC, PC, SM, CB, LB, JC, AK, JIMS, VM, GIV, ECS were responsible for conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results. CB, LB, JC, AK, NCC, GH, THJ, UM, JIMS, VM, GIV, ECS, TT, PV contributed to designing the review and provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
Ege Can Serefoglu is Editor-in-Chief of International Journal of Impotence Research. Luca Boeri, Marco Falcone, and Murat Gul are Associate Editors of International Journal of Impotence Research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cocci, A., Capogrosso, P., Minhas, S. et al. Penile prosthesis implantation: a systematic review of intraoperative and postoperative complications. Int J Impot Res (2025). https://doi.org/10.1038/s41443-025-01108-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41443-025-01108-4